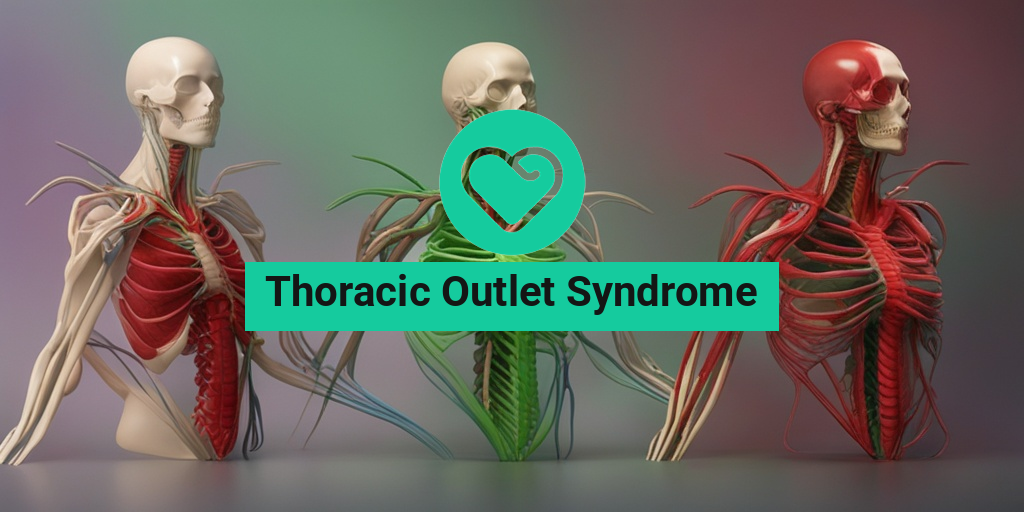
What Is Thoracic Outlet Syndrome?
Thoracic Outlet Syndrome (TOS) is a group of disorders that affect the nerves and blood vessels in the thoracic outlet, a region of the body that includes the neck, shoulder, and upper chest. The thoracic outlet is a narrow passageway that serves as a gateway for nerves, arteries, and veins that connect the arm to the neck and chest. When the nerves or blood vessels in this region become compressed or irritated, it can lead to a range of symptoms, including pain, numbness, tingling, and weakness in the neck, shoulder, and arm.
The Anatomy of Thoracic Outlet Syndrome
The thoracic outlet is a complex region that consists of several structures, including the scalene muscles, the first rib, and the clavicle (collarbone). The nerves that originate from the neck and travel down to the arm, known as the brachial plexus, pass through this region. The subclavian artery and vein, which supply blood to the arm, also pass through the thoracic outlet.
When the nerves or blood vessels in the thoracic outlet become compressed or irritated, it can lead to TOS. This compression can occur due to a variety of reasons, including:
- Anatomical abnormalities, such as a cervical rib or an abnormal first rib
- Muscle imbalances, such as tight scalene muscles or weak shoulder muscles
- Injury or trauma, such as a fall or a car accident
- Poor posture, which can put pressure on the nerves and blood vessels in the thoracic outlet
Thoracic Outlet Syndrome Symptoms
The symptoms of Thoracic Outlet Syndrome can vary depending on the severity of the compression and the individual’s overall health. However, common symptoms of TOS include:
Neurological Symptoms
Many people with TOS experience neurological symptoms, such as:
- Numbness or tingling in the arm, hand, or fingers
- Weakeness in the arm or hand
- Pain in the neck, shoulder, or arm
- Tingling or burning sensations in the arm or hand
Vascular Symptoms
Some people with TOS may experience vascular symptoms, such as:
- Coldness in the arm or hand
- Discoloration of the arm or hand
- Weakened pulse in the arm
If you’re experiencing any of these symptoms, it’s essential to consult with a healthcare professional for an accurate diagnosis and treatment plan. In the meantime, you can explore evidence-based health answers on Yesil Health AI, a valuable resource for health information.
👍

Thoracic Outlet Syndrome Causes and Risk Factors
Thoracic outlet syndrome (TOS) is a complex condition that affects the nerves and blood vessels in the thoracic outlet, a region that includes the neck, shoulder, and upper chest. While the exact causes of TOS are still not fully understood, research has identified several factors that can contribute to its development.
Genetic Predisposition
Some people may be born with a genetic predisposition to develop TOS. For example, individuals with a family history of TOS or those with certain genetic conditions, such as Marfan syndrome, may be more likely to develop the condition.
Physical Trauma
Physical trauma, such as a car accident, fall, or sports injury, can cause damage to the nerves and blood vessels in the thoracic outlet, leading to TOS. This type of trauma can cause inflammation, scarring, and compression of the nerves and blood vessels, which can lead to symptoms of TOS.
Poor Posture
Poor posture can put strain on the muscles and joints in the neck and shoulder region, leading to compression of the nerves and blood vessels in the thoracic outlet. This compression can cause symptoms of TOS, such as pain, numbness, and tingling in the arms and hands.
Repetitive Strains
Repetitive strains, such as those experienced by athletes, musicians, or individuals who perform repetitive tasks, can cause inflammation and compression of the nerves and blood vessels in the thoracic outlet. This can lead to symptoms of TOS, such as pain, numbness, and tingling in the arms and hands.
Other Medical Conditions
Certain medical conditions, such as cervical spine disorders, rotator cuff injuries, and tumors, can cause compression of the nerves and blood vessels in the thoracic outlet, leading to TOS.
Lifestyle Factors
Lifestyle factors, such as smoking, obesity, and poor nutrition, can contribute to the development of TOS. These factors can lead to inflammation, poor circulation, and compression of the nerves and blood vessels in the thoracic outlet, increasing the risk of developing TOS.
Thoracic Outlet Syndrome Diagnosis
Diagnosing thoracic outlet syndrome (TOS) can be challenging, as the symptoms can be similar to those of other conditions. A thorough medical history, physical examination, and diagnostic tests are necessary to rule out other conditions and confirm a diagnosis of TOS.
Medical History
A thorough medical history is essential in diagnosing TOS. Your doctor will ask about your symptoms, including their severity, duration, and any factors that trigger or relieve them. They will also ask about your medical history, including any previous injuries or conditions that may be contributing to your symptoms.
Physical Examination
A physical examination is necessary to assess the range of motion, strength, and sensation in your neck, shoulder, and arm. Your doctor may perform various tests, such as the Adson’s test, Wright’s test, and Roos test, to assess the compression of the nerves and blood vessels in the thoracic outlet.
Diagnostic Tests
Diagnostic tests, such as electromyography (EMG), nerve conduction studies (NCS), and imaging studies (e.g., X-rays, MRI, CT scans), may be necessary to confirm a diagnosis of TOS. These tests can help identify compression or damage to the nerves and blood vessels in the thoracic outlet.
Differential Diagnosis
A differential diagnosis is necessary to rule out other conditions that may be causing your symptoms. Your doctor may consider other conditions, such as cervical spine disorders, rotator cuff injuries, and peripheral neuropathy, before making a diagnosis of TOS.
👍 Remember, an accurate diagnosis of TOS is essential for effective treatment and management of the condition. If you suspect you may have TOS, consult with your doctor to discuss your symptoms and determine the best course of action.

Thoracic Outlet Syndrome Treatment
Thoracic outlet syndrome (TOS) is a complex condition that requires a comprehensive treatment plan to alleviate symptoms and improve quality of life. The goal of treatment is to reduce compression on the nerves and blood vessels in the thoracic outlet, relieve pain and discomfort, and restore normal function to the affected arm and hand.
Conservative Treatment Options
The initial treatment approach for TOS typically involves conservative methods, which can be effective in managing symptoms and improving function. These may include:
- Pain management: Over-the-counter pain medications, such as NSAIDs, or prescription medications may be prescribed to reduce pain and inflammation.
- Physical therapy: A customized exercise program can help improve posture, strengthen muscles, and increase range of motion. (We’ll dive deeper into exercises and physical therapy later in this article!)
- Posture correction: Improving posture can help reduce compression on the nerves and blood vessels in the thoracic outlet.
- Activity modification: Avoiding activities that aggravate symptoms and taking regular breaks to rest the affected arm and hand can help reduce discomfort.
Surgical Treatment Options
In some cases, surgery may be necessary to relieve compression on the nerves and blood vessels in the thoracic outlet. Surgical options may include:
- Scalene muscle release: This procedure involves releasing the scalene muscles, which can help reduce compression on the nerves and blood vessels.
- Rib resection: Removing a portion of the first rib can help relieve compression on the nerves and blood vessels.
- Brachial plexus decompression: This procedure involves releasing the brachial plexus, a network of nerves that can become compressed in TOS.
Thoracic Outlet Syndrome Exercises and Physical Therapy
Exercise and physical therapy play a crucial role in the management of thoracic outlet syndrome. A well-structured exercise program can help improve posture, strengthen muscles, and increase range of motion, ultimately reducing symptoms and improving function.
Stretching Exercises
Stretching exercises can help improve flexibility and reduce tension in the muscles of the neck, shoulder, and arm. Some examples of stretching exercises that may be beneficial for TOS include:
- Chin tucks: Stand or sit with good posture and slowly tuck your chin towards your chest, holding for 30 seconds.
- Shoulder rolls: Roll your shoulders forward and backward in a circular motion, repeating for 10-15 repetitions.
- Chest stretches: Stand in a doorway with your hands on the doorframe at shoulder height. Lean forward, stretching your chest and shoulders, holding for 30 seconds.
Strengthening Exercises
Strengthening exercises can help improve muscle tone and reduce fatigue in the muscles of the neck, shoulder, and arm. Some examples of strengthening exercises that may be beneficial for TOS include:
- Shoulder blade squeezes: Sit or stand with good posture and squeeze your shoulder blades together, holding for 5-10 seconds.
- Arm raises: Hold light weights or resistance bands and raise your arms to shoulder height, holding for 5-10 seconds.
- Neck strengthening exercises: Perform exercises that target the muscles of the neck, such as isometric neck flexion and extension.
It’s essential to work with a healthcare professional, such as a physical therapist, to develop a customized exercise program that addresses your specific needs and goals. They can help you progress through exercises, modify them as needed, and provide guidance on proper technique. 💪
Remember, a comprehensive treatment plan for thoracic outlet syndrome should include a combination of conservative and surgical options, as well as a commitment to regular exercise and physical therapy. By working together with your healthcare team, you can develop a personalized plan that helps you manage symptoms, improve function, and regain control over your daily life. 🌟

Thoracic Outlet Syndrome Surgery
Thoracic outlet syndrome (TOS) surgery is a last resort for individuals who have not responded to conservative treatments and are experiencing severe symptoms. The goal of surgery is to relieve compression on the nerves and blood vessels in the thoracic outlet, thereby alleviating pain, numbness, and weakness in the affected arm and hand.
Types of Thoracic Outlet Syndrome Surgery
There are several types of surgeries that can be performed to treat TOS, including:
- Scalene lymph node removal: This surgery involves removing the scalene lymph node, which can compress the nerves and blood vessels in the thoracic outlet.
- First rib resection: This surgery involves removing the first rib, which can compress the nerves and blood vessels in the thoracic outlet.
- Brachial plexus neurolysis: This surgery involves releasing the compressed nerves in the brachial plexus, which can help to alleviate pain and numbness in the arm and hand.
What to Expect During Thoracic Outlet Syndrome Surgery
The surgery is usually performed under general anesthesia, and the procedure can take several hours to complete. The surgeon will make an incision in the neck or chest area, depending on the type of surgery being performed. The surgeon will then carefully dissect the tissues to expose the compressed nerves and blood vessels, and remove any structures that are causing compression.
Risks and Complications of Thoracic Outlet Syndrome Surgery
As with any surgery, there are risks and complications associated with TOS surgery. These can include:
- Infection: As with any surgery, there is a risk of infection with TOS surgery.
- Nerve damage: There is a risk of nerve damage during the surgery, which can result in numbness, tingling, or weakness in the arm and hand.
- Bleeding: There is a risk of bleeding during the surgery, which can lead to complications.
Thoracic Outlet Syndrome Complications
Thoracic outlet syndrome can lead to several complications if left untreated or if treatment is delayed. Some of the possible complications include:
Chronic Pain
Chronic pain is a common complication of TOS. If the compression on the nerves and blood vessels is not relieved, it can lead to chronic pain in the neck, shoulder, and arm.
Nerve Damage
If the compression on the nerves is not relieved, it can lead to permanent nerve damage. This can result in numbness, tingling, and weakness in the arm and hand.
Vascular Complications
TOS can also lead to vascular complications, such as blood clots, aneurysms, and thrombosis. These complications can be life-threatening if left untreated.
Disability
If TOS is not treated, it can lead to disability and a decreased quality of life. Individuals may experience difficulty performing daily activities, such as dressing, grooming, and feeding themselves.
It’s essential to seek medical attention if you’re experiencing symptoms of TOS. Early diagnosis and treatment can help to prevent complications and improve outcomes. 💊
Frequently Asked Questions about Thoracic Outlet Syndrome
What is Thoracic Outlet Syndrome?
Thoracic Outlet Syndrome (TOS) is a group of disorders that occur when the nerves or blood vessels in the thoracic outlet, which is the space between the collarbone and the first rib, become compressed or irritated.
What are the Symptoms of Thoracic Outlet Syndrome?
Common symptoms of TOS include:
- Pain or numbness in the neck, shoulder, or arm
- Weakened grip or difficulty holding objects
- Tingling or burning sensations in the fingers
- Swelling or discoloration of the arm or hand
- Fatigue or weakness in the arm or hand
How is Thoracic Outlet Syndrome Diagnosed?
TOS can be diagnosed through a combination of physical examination, medical history, and diagnostic tests such as:
- Adson’s test
- Wright’s test
- Roos test
- Electromyography (EMG)
- Nerve conduction studies (NCS)
- Imaging tests such as X-rays, CT scans, or MRI
What are the Treatment Options for Thoracic Outlet Syndrome?
Treatment for TOS typically involves a combination of:
- Physical therapy exercises to improve posture, strengthen muscles, and increase range of motion
- Pain management medications
- Therapeutic injections
- Surgery to relieve compression on the nerves or blood vessels
Can Thoracic Outlet Syndrome be Prevented?
While TOS cannot be completely prevented, certain lifestyle changes can reduce the risk of developing the condition:
- Maintaining good posture
- Taking regular breaks to stretch and move
- Avoiding heavy lifting or bending
- Improving overall physical fitness
What is the ICD-10 Code for Thoracic Outlet Syndrome?
The ICD-10 code for Thoracic Outlet Syndrome is G54.0.
Can Thoracic Outlet Syndrome be Treated with Physical Therapy?
Yes, physical therapy can be an effective treatment for TOS. A physical therapist can help improve posture, strengthen muscles, and increase range of motion to reduce compression on the nerves or blood vessels.
What are the Exercises for Thoracic Outlet Syndrome?
Common exercises for TOS include:
- Shoulder rolls
- Chest stretches
- Neck stretches
- Arm circles
- Finger spreads
Can Thoracic Outlet Syndrome be Rated by the VA?
Yes, the Department of Veterans Affairs (VA) recognizes TOS as a service-connected condition and provides disability ratings for eligible veterans.
What is the Connection between Thoracic Outlet Syndrome and Other Conditions?
TOS can be associated with other conditions such as:
- Cervical spinal stenosis
- Rotator cuff injuries
- Carpal tunnel syndrome
- Ulnar nerve entrapment
I hope this FAQ helps! 😊