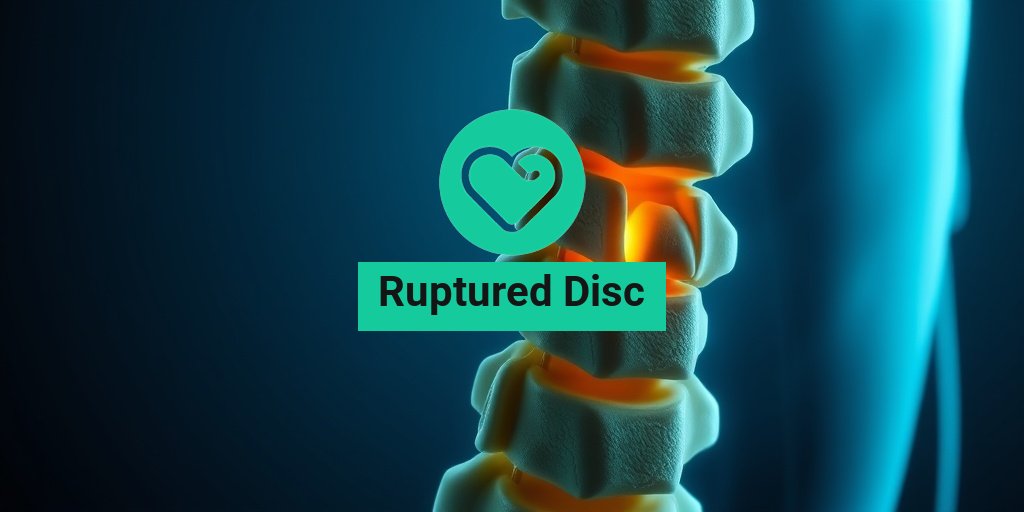
What Is a Ruptured Disc?
A ruptured disc, often referred to as a herniated or slipped disc, occurs when the soft inner gel of a spinal disc protrudes through a tear in the tougher exterior. This condition can happen in any part of the spine but is most common in the lower back (lumbar region) and neck (cervical region). The discs act as cushions between the vertebrae, providing support and flexibility to the spine. When a disc ruptures, it can lead to significant discomfort and a range of other symptoms.
Causes of a Ruptured Disc
Several factors can contribute to the development of a ruptured disc, including:
- Aging: As we age, our discs lose hydration and elasticity, making them more susceptible to injury.
- Injury: Sudden trauma from accidents or falls can cause a disc to rupture.
- Repetitive Strain: Jobs or activities that involve heavy lifting or twisting can put excessive pressure on the discs.
- Genetics: A family history of disc problems can increase your risk.
Types of Ruptured Discs
Ruptured discs can be classified into two main types:
- Protruded Disc: The disc bulges out but does not break through the outer layer.
- Extruded Disc: The inner gel breaks through the outer layer, potentially pressing on nearby nerves.
Ruptured Disc Symptoms
The symptoms of a ruptured disc can vary widely depending on the location of the rupture and whether it is pressing on nearby nerves. Here are some common symptoms to watch for:
Lower Back Symptoms
If the ruptured disc is in the lower back, you may experience:
- Severe Pain: This pain can be sharp or dull and may radiate down the legs (sciatica).
- Numbness or Tingling: You might feel a tingling sensation or numbness in your legs or feet.
- Weakness: Muscle weakness in the legs can occur, making it difficult to walk or stand.
Neck Symptoms
For a ruptured disc in the neck, symptoms may include:
- Neck Pain: Pain that can radiate to the shoulders, arms, and hands.
- Numbness or Tingling: Similar to lower back symptoms, you may experience tingling or numbness in the arms or hands.
- Weakness: Weakness in the arms or hands can affect grip strength.
When to Seek Medical Attention
If you experience severe pain, numbness, or weakness that affects your daily activities, it’s crucial to consult a healthcare professional. Early diagnosis and treatment can help prevent further complications and improve recovery outcomes.
For more detailed information about ruptured disc treatment options, including non-surgical and surgical interventions, consider visiting Yesil Health AI for evidence-based health answers.
Understanding the symptoms and causes of a ruptured disc is essential for effective management and recovery. If you suspect you have a ruptured disc, don’t hesitate to seek medical advice. Remember, early intervention can make a significant difference in your healing journey! 🌟

Ruptured Disc Causes
A ruptured disc, also known as a herniated disc, occurs when the soft inner gel of the disc protrudes through a tear in the tougher exterior. This condition can lead to significant pain and discomfort, often affecting mobility. Understanding the causes of a ruptured disc is crucial for prevention and effective treatment.
1. Age-Related Degeneration
As we age, our spinal discs naturally lose hydration and elasticity. This degeneration makes them more susceptible to injury. The risk of a ruptured disc increases as the discs become less flexible and more brittle, making them prone to tearing even with minor strain.
2. Injury or Trauma
Acute injuries, such as those sustained in sports or accidents, can lead to a ruptured disc. A sudden impact or heavy lifting can cause the disc to rupture, especially if proper lifting techniques are not used. It’s essential to be cautious during physical activities to minimize the risk of injury.
3. Repetitive Strain
Engaging in repetitive motions, particularly those that involve heavy lifting or twisting, can contribute to the wear and tear of spinal discs. Over time, this repetitive strain can lead to a rupture, especially in individuals who perform such activities regularly.
4. Poor Posture
Poor posture, whether sitting or standing, can place undue stress on the spine. This stress can weaken the discs and increase the likelihood of a rupture. Maintaining proper posture is vital for spinal health and can help prevent a ruptured disc.
5. Obesity
Excess body weight can put additional pressure on the spine, increasing the risk of disc problems. Maintaining a healthy weight through diet and exercise can significantly reduce the chances of experiencing a ruptured disc.
Ruptured Disc Risk Factors
Identifying the risk factors associated with a ruptured disc can help individuals take proactive steps to protect their spinal health. Here are some key risk factors to consider:
1. Age
As mentioned earlier, age is a significant risk factor. Individuals aged 30 to 50 are more likely to experience a ruptured disc due to the natural degeneration of spinal discs over time.
2. Occupation
Jobs that require heavy lifting, repetitive motions, or prolonged sitting can increase the risk of a ruptured disc. Professions such as construction work, nursing, and office jobs can all contribute to spinal stress.
3. Genetics
Family history plays a role in the likelihood of developing a ruptured disc. If you have a family member who has experienced disc issues, you may be at a higher risk.
4. Sedentary Lifestyle
A lack of physical activity can weaken the muscles that support the spine, making it more vulnerable to injury. Regular exercise is essential for maintaining a strong and healthy back.
5. Smoking
Smoking can hinder blood flow to the discs, leading to degeneration and increasing the risk of a rupture. Quitting smoking can improve overall health and reduce the risk of spinal issues.
6. Previous Back Problems
If you have a history of back problems, such as previous herniated discs or chronic back pain, you may be at a higher risk for experiencing a ruptured disc in the future. It’s essential to manage existing conditions with the help of a healthcare professional.
By understanding the causes and risk factors associated with a ruptured disc, individuals can take proactive measures to protect their spinal health and reduce the likelihood of injury. Regular check-ups, maintaining a healthy lifestyle, and practicing good posture are all effective strategies for prevention. 🏋️♂️💪
Ruptured Disc Diagnosis
Diagnosing a ruptured disc can be a complex process, as the symptoms often overlap with other conditions. A ruptured disc, also known as a herniated disc, occurs when the soft inner gel of the disc leaks out through a tear in the tougher exterior. This can lead to pain, numbness, and weakness in the affected area. Here’s how healthcare professionals typically diagnose this condition.
Initial Consultation
The first step in diagnosing a ruptured disc is a thorough consultation with a healthcare provider. During this visit, the doctor will:
- Review your medical history
- Discuss your symptoms, including the location and intensity of pain
- Ask about any previous injuries or conditions that may contribute to your symptoms
Physical Examination
After the initial consultation, a physical examination is conducted. The doctor will:
- Check your reflexes
- Assess your muscle strength
- Evaluate your range of motion
- Look for signs of nerve damage, such as numbness or tingling
Imaging Tests
If a ruptured disc is suspected, your doctor may recommend imaging tests to confirm the diagnosis. Common tests include:
- X-rays: While X-rays cannot show a ruptured disc, they can help rule out other issues, such as fractures.
- Magnetic Resonance Imaging (MRI): This is the most effective method for visualizing soft tissues, including discs. An MRI can clearly show the location and extent of the rupture.
- Computed Tomography (CT) Scan: A CT scan can provide detailed images of the spine and help identify a ruptured disc.
Once the diagnosis is confirmed, your healthcare provider will discuss the best treatment options tailored to your specific condition.
Ruptured Disc Treatment Options
Treating a ruptured disc involves a combination of non-surgical and surgical options, depending on the severity of the condition and the symptoms experienced. Here’s a breakdown of the most common treatment options available.
Non-Surgical Treatments
Most patients with a ruptured disc find relief through non-surgical treatments. These options include:
- Physical Therapy: A physical therapist can design a personalized exercise program to strengthen the muscles around the spine, improve flexibility, and reduce pain.
- Medications: Over-the-counter pain relievers, such as ibuprofen or acetaminophen, can help manage pain. In some cases, your doctor may prescribe stronger medications or muscle relaxants.
- Injections: Corticosteroid injections can reduce inflammation and alleviate pain. These are typically administered directly into the affected area.
- Rest and Activity Modification: Taking a break from activities that exacerbate the pain can be beneficial. Gradually returning to normal activities is essential for recovery.
Surgical Treatments
If non-surgical treatments do not provide relief after several weeks, or if you experience severe symptoms such as significant weakness or loss of bladder control, surgery may be necessary. Common surgical options include:
- Discectomy: This procedure involves removing the portion of the disc that is pressing on the nerve. It is one of the most common surgeries for a ruptured disc.
- Laminectomy: In this surgery, a portion of the vertebra is removed to relieve pressure on the spinal cord or nerves.
- Spinal Fusion: In some cases, the surgeon may recommend fusing two or more vertebrae together to stabilize the spine.
Recovery and Rehabilitation
Recovery from a ruptured disc varies depending on the treatment method. Non-surgical treatments may lead to improvement within a few weeks, while surgical recovery can take several months. Engaging in a rehabilitation program is crucial to regain strength and mobility. Your healthcare provider will guide you on the best practices for a successful recovery.
In conclusion, if you suspect you have a ruptured disc, it’s essential to seek medical advice promptly. Early diagnosis and appropriate treatment can significantly improve your quality of life and help you return to your daily activities. 🌟

Ruptured Disc Recovery
Recovering from a ruptured disc can be a challenging journey, but understanding the process can help ease your concerns. A ruptured disc, often referred to as a herniated disc, occurs when the soft inner gel of the disc leaks out through a tear in the outer layer. This can lead to pain, numbness, and weakness in the affected area. Here’s what you need to know about recovery.
Understanding the Recovery Timeline
The recovery time for a ruptured disc varies significantly based on several factors, including the severity of the rupture, the location of the disc, and the treatment approach. Generally, recovery can take anywhere from a few weeks to several months. Here’s a breakdown of what to expect:
- Initial Phase (1-2 weeks): During this time, rest is crucial. You may experience significant pain and discomfort, and it’s essential to avoid activities that could exacerbate your condition.
- Rehabilitation Phase (3-6 weeks): As pain decreases, physical therapy often begins. This phase focuses on strengthening the muscles around the spine and improving flexibility.
- Long-Term Recovery (6 weeks to several months): Full recovery can take time. Many individuals find that they can return to normal activities within a few months, but some may require ongoing therapy.
Treatment Options for Recovery
There are several treatment options available for those suffering from a ruptured disc. These can range from conservative methods to surgical interventions:
- Physical Therapy: A tailored exercise program can help strengthen the back and improve mobility.
- Medications: Over-the-counter pain relievers or prescription medications can help manage pain and inflammation.
- Injections: Corticosteroid injections may provide temporary relief from pain and inflammation.
- Surgery: In severe cases, surgical options such as discectomy or spinal fusion may be necessary to relieve pressure on the nerves.
Self-Care Strategies
In addition to professional treatment, there are several self-care strategies that can aid in recovery:
- Rest: Allow your body time to heal. Avoid heavy lifting and strenuous activities.
- Ice and Heat Therapy: Applying ice can reduce inflammation, while heat can help relax tense muscles.
- Maintain Good Posture: Proper posture can alleviate pressure on the spine and promote healing.
- Stay Active: Engage in light activities as tolerated, such as walking, to promote circulation and healing.
Ruptured Disc Prevention Tips
Preventing a ruptured disc is often more manageable than recovering from one. By adopting certain lifestyle habits, you can significantly reduce your risk. Here are some effective prevention tips:
Maintain a Healthy Weight
Excess weight puts additional strain on your spine. Maintaining a healthy weight through a balanced diet and regular exercise can help reduce the risk of a ruptured disc. Aim for a diet rich in fruits, vegetables, lean proteins, and whole grains. 🍏🥦
Practice Good Posture
Whether sitting at a desk or lifting heavy objects, maintaining good posture is crucial. Keep your back straight, shoulders back, and avoid slouching. When lifting, use your legs instead of your back to avoid unnecessary strain. 🏋️♂️
Stay Active
Regular physical activity strengthens the muscles that support your spine. Incorporate exercises that focus on core strength, flexibility, and balance. Activities like yoga and Pilates can be particularly beneficial. 🧘♀️
Use Proper Lifting Techniques
When lifting heavy objects, always bend at the knees and keep the object close to your body. Avoid twisting your back while lifting, as this can increase the risk of injury. 📦
Listen to Your Body
If you experience persistent pain or discomfort, don’t ignore it. Early intervention can prevent more severe issues, including a ruptured disc. Consult a healthcare professional if you have concerns. 🩺
By following these prevention tips and understanding the recovery process, you can take proactive steps to protect your spine and maintain your overall health. Remember, your spine is vital to your well-being, so treat it with care! 🌟

Frequently Asked Questions about Ruptured Discs
What is a ruptured disc?
A ruptured disc occurs when the soft inner material of a spinal disc protrudes through the outer layer, potentially pressing on nearby nerves. This condition can lead to pain, numbness, or weakness in the affected area.
What are the symptoms of a ruptured disc?
Symptoms can vary depending on the location of the rupture. Common signs include:
- Lower back pain
- Neck pain
- Numbness or tingling in the arms or legs
- Muscle weakness
- Difficulty with movement
How is a ruptured disc treated?
Treatment options for a ruptured disc may include:
- Physical therapy
- Medications for pain relief
- Injections to reduce inflammation
- Surgery in severe cases
What is the recovery time for a ruptured disc?
Recovery time can vary widely based on the severity of the rupture and the treatment method used. Generally, individuals may take several weeks to months to fully recover, especially if surgery is involved.
How does a ruptured disc differ from a herniated disc?
While the terms are often used interchangeably, a ruptured disc specifically refers to the disc’s outer layer breaking, whereas a herniated disc typically describes the inner material pushing out. Both conditions can cause similar symptoms.
Can dogs experience ruptured discs?
Yes, dogs can suffer from ruptured discs, particularly in their neck or back. Symptoms may include pain, difficulty walking, or weakness in the limbs. If you suspect your dog has this condition, consult a veterinarian promptly.
What are the differences between a ruptured disc and a bulging disc?
A bulging disc occurs when the disc protrudes but remains intact, while a ruptured disc involves a tear in the outer layer. Both can lead to similar symptoms, but the severity and treatment options may differ.
Is surgery always necessary for a ruptured disc?
No, surgery is not always required. Many individuals find relief through conservative treatments such as physical therapy and medication. However, if symptoms persist or worsen, surgical options may be considered.
What lifestyle changes can help manage a ruptured disc?
To manage symptoms and promote healing, consider the following lifestyle changes:
- Maintain a healthy weight
- Engage in low-impact exercises
- Practice good posture
- Avoid heavy lifting
When should I see a doctor for a ruptured disc?
If you experience severe pain, numbness, or weakness that affects your daily activities, it is important to seek medical attention. Early intervention can help prevent further complications.