What Is a Polyp?
A polyp is a growth that occurs on the surface of a mucous membrane, which can be found in various parts of the body, including the colon, stomach, and nasal passages. These growths can vary in size and shape, and while many polyps are benign (non-cancerous), some can develop into cancer over time if left untreated. Understanding what polyps are and how they can affect your health is crucial for early detection and prevention.
Polyps are typically classified as either sessile (flat) or pedunculated (attached to the surface by a stalk). They can be discovered during routine medical examinations, such as colonoscopies, where doctors can remove them for further analysis. Regular screenings are essential, especially for individuals over the age of 50 or those with a family history of polyps or colorectal cancer.
Symptoms of Polyps
Many polyps do not cause noticeable symptoms, which is why they can go undetected for years. However, some individuals may experience:
- Rectal bleeding
- Changes in bowel habits, such as diarrhea or constipation
- Abdominal pain or discomfort
- Unexplained weight loss
If you experience any of these symptoms, it is essential to consult a healthcare professional for evaluation and potential screening.
Types of Polyps
There are several types of polyps, each with distinct characteristics and potential health implications. Understanding these types can help you recognize the importance of regular health check-ups.
1. Adenomatous Polyps
Adenomatous polyps are the most common type of polyp found in the colon. They are considered precursors to colorectal cancer, meaning they have the potential to become cancerous over time. There are three subtypes of adenomatous polyps:
- Tubular adenomas: These are the most common and have a lower risk of becoming cancerous.
- Tubulovillous adenomas: These have features of both tubular and villous adenomas and carry a moderate risk of cancer.
- Villous adenomas: These are less common but have a higher risk of becoming cancerous.
2. Hyperplastic Polyps
Hyperplastic polyps are generally small and considered benign. They are typically found in the colon and are not associated with an increased risk of colorectal cancer. However, their presence may warrant further investigation, especially if they are large or if there are multiple polyps.
3. Inflammatory Polyps
Inflammatory polyps often occur in individuals with inflammatory bowel disease (IBD), such as ulcerative colitis or Crohn’s disease. These polyps are usually benign but can indicate underlying inflammation that requires management.
4. Sessile Serrated Polyps
Sessile serrated polyps are a type of polyp that can also develop into colorectal cancer. They are often flat and can be challenging to detect during routine screenings. Early removal is crucial to prevent potential progression to cancer.
5. Nasal Polyps
Nasal polyps are soft, painless growths that develop in the lining of the nasal passages or sinuses. They are often associated with allergies, asthma, or chronic sinus infections. While nasal polyps are not cancerous, they can cause symptoms such as nasal congestion, loss of smell, and sinus pressure.
Conclusion
Understanding the different types of polyps and their potential implications is vital for maintaining your health. Regular screenings and consultations with healthcare professionals can help detect polyps early, allowing for timely intervention. If you’re looking for more information on health-related topics, consider visiting Yesil Health AI for evidence-based answers to your health questions.
Remember, being proactive about your health can make a significant difference in preventing serious conditions associated with polyps. Stay informed, stay healthy! 🌟

Polyp Symptoms
Polyps are abnormal growths that can develop in various parts of the body, most commonly in the colon, stomach, and nasal passages. While many polyps are benign, some can lead to serious health issues, including cancer. Recognizing the symptoms of polyps is crucial for early detection and treatment. Here are some common symptoms associated with polyps:
1. Gastrointestinal Symptoms
When polyps form in the gastrointestinal tract, they can cause a range of symptoms, including:
- Rectal bleeding: This is one of the most common symptoms of colon polyps. You may notice blood in your stool or on toilet paper.
- Change in bowel habits: This can include diarrhea, constipation, or a change in the consistency of your stool.
- Abdominal pain: Some individuals may experience cramping or discomfort in the abdominal area.
- Unexplained weight loss: If you are losing weight without trying, it could be a sign of an underlying issue, including polyps.
2. Nasal Polyps Symptoms
Nasal polyps can lead to a variety of symptoms that affect your respiratory health:
- Blocked nasal passages: This can cause difficulty breathing through the nose.
- Reduced sense of smell: Many people with nasal polyps report a diminished ability to smell.
- Frequent sinus infections: Chronic sinusitis can occur due to the obstruction caused by polyps.
- Facial pain or pressure: This can be particularly noticeable around the forehead and cheeks.
3. Other Symptoms
Polyps can also manifest in other areas of the body, leading to different symptoms:
- Skin polyps: These may appear as small, soft bumps on the skin, often painless.
- Polyps in the bladder: Symptoms may include blood in the urine or frequent urination.
It’s important to note that many polyps do not cause symptoms, especially in their early stages. Regular screenings, such as colonoscopies, are essential for early detection, particularly for colorectal polyps. If you experience any of the symptoms mentioned above, consult a healthcare professional for further evaluation. 🩺
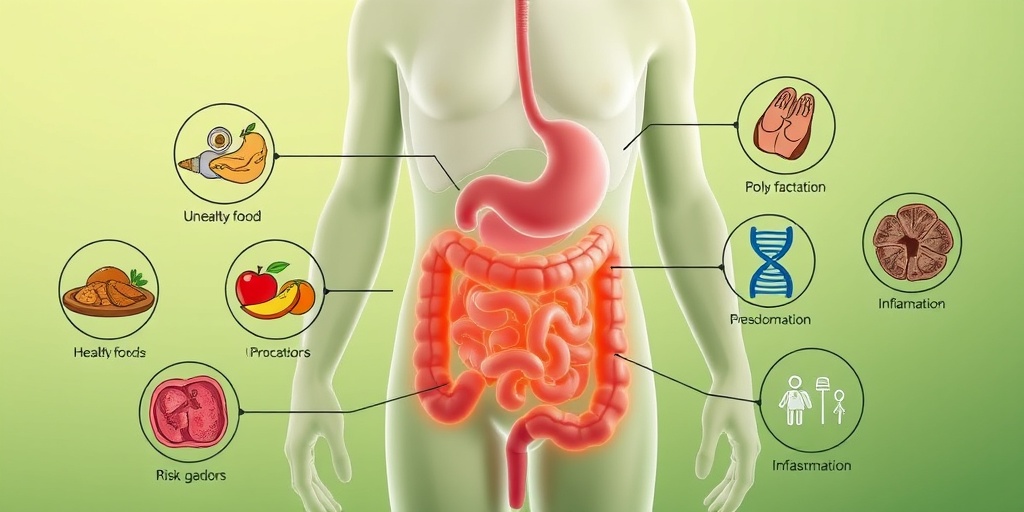
Causes of Polyps
The exact cause of polyps is not always clear, but several factors can contribute to their development. Understanding these causes can help in prevention and early detection. Here are some of the primary causes of polyps:
1. Genetic Factors
Some individuals may have a genetic predisposition to developing polyps. Conditions such as:
- Familial adenomatous polyposis (FAP): A hereditary condition that causes numerous polyps in the colon and rectum.
- Lynch syndrome: Also known as hereditary nonpolyposis colorectal cancer (HNPCC), this condition increases the risk of colorectal cancer and polyps.
2. Lifestyle Factors
Certain lifestyle choices can increase the risk of developing polyps:
- Diet: A diet high in red and processed meats and low in fruits and vegetables may contribute to polyp formation.
- Obesity: Being overweight is linked to an increased risk of colorectal polyps.
- Smoking: Tobacco use has been associated with a higher risk of developing polyps.
- Alcohol consumption: Excessive alcohol intake may also play a role in polyp development.
3. Age and Gender
Age is a significant risk factor for polyps, with most cases occurring in individuals over the age of 50. Additionally, men are generally at a higher risk than women for developing certain types of polyps, particularly colorectal polyps.
4. Inflammatory Conditions
Chronic inflammatory conditions of the gastrointestinal tract, such as:
- Ulcerative colitis: This condition can lead to the development of polyps in the colon.
- Crohn’s disease: Similar to ulcerative colitis, Crohn’s disease can also increase the risk of polyps.
Understanding the causes of polyps can empower individuals to make informed lifestyle choices and seek regular medical check-ups. If you have concerns about polyps or related symptoms, don’t hesitate to reach out to a healthcare provider for guidance. 🩺
Risk Factors for Polyps
Polyps are abnormal growths that can develop in various parts of the body, most commonly in the colon and rectum. Understanding the risk factors associated with polyps is crucial for prevention and early detection. Here, we’ll explore the key factors that may increase your likelihood of developing polyps.
Age
One of the most significant risk factors for polyps is age. Individuals over the age of 50 are at a higher risk of developing colorectal polyps. As we age, our cells undergo changes that can lead to abnormal growths. Regular screenings become increasingly important as you reach this age milestone.
Family History
If you have a family history of polyps or colorectal cancer, your risk is elevated. Genetic factors play a role in the development of polyps, and conditions such as familial adenomatous polyposis (FAP) can significantly increase your chances of developing multiple polyps. It’s essential to discuss your family history with your healthcare provider to determine an appropriate screening schedule.
Dietary Factors
Your diet can also influence your risk of developing polyps. Diets high in red and processed meats, along with low fiber intake, have been linked to an increased risk. Conversely, a diet rich in fruits, vegetables, and whole grains may help reduce your risk. Consider incorporating more polyphenols—found in foods like berries, nuts, and green tea—into your diet, as they have protective properties against polyp formation. 🍏🥦
Obesity and Physical Inactivity
Being overweight or obese can increase your risk of developing polyps. Excess body weight is associated with inflammation and hormonal changes that may promote polyp growth. Additionally, a sedentary lifestyle can contribute to obesity, making regular physical activity essential for maintaining a healthy weight and reducing your risk. Aim for at least 150 minutes of moderate exercise each week. 🏃♂️💪
Smoking and Alcohol Consumption
Both smoking and excessive alcohol consumption have been linked to an increased risk of polyps. Tobacco use can lead to various health issues, including the development of polyps in the colon. Similarly, heavy drinking can contribute to inflammation and other changes in the digestive tract. Reducing or eliminating these habits can significantly lower your risk. 🚭🍷
Medical Conditions
Certain medical conditions can also increase your risk of developing polyps. Conditions such as inflammatory bowel disease (IBD), including Crohn’s disease and ulcerative colitis, are associated with a higher incidence of colorectal polyps. If you have IBD, it’s crucial to work closely with your healthcare provider to monitor your condition and schedule regular screenings.
Polyp Diagnosis
Diagnosing polyps typically involves a combination of medical history, physical examinations, and diagnostic tests. Early detection is key to effective treatment and prevention of potential complications, such as colorectal cancer. Here’s how healthcare professionals diagnose polyps:
Medical History and Symptoms
Your healthcare provider will begin by taking a detailed medical history, including any symptoms you may be experiencing. Common symptoms of polyps can include:
- Rectal bleeding
- Changes in bowel habits
- Abdominal pain or discomfort
- Unexplained weight loss
While many polyps do not cause symptoms, reporting any unusual changes can help your doctor determine the need for further investigation.
Colonoscopy
The most common and effective method for diagnosing colorectal polyps is through a colonoscopy. During this procedure, a long, flexible tube with a camera is inserted into the rectum and guided through the colon. This allows the doctor to visually inspect the lining of the colon for any abnormal growths. If polyps are found, they can often be removed during the procedure for further examination.
Biopsy
If polyps are removed during a colonoscopy, they are sent to a laboratory for a biopsy. This process involves examining the tissue under a microscope to determine whether the polyp is benign (non-cancerous) or malignant (cancerous). Understanding the nature of the polyp is crucial for determining the appropriate follow-up and treatment options.
Imaging Tests
In some cases, imaging tests such as a CT colonography (virtual colonoscopy) may be used to detect polyps. This non-invasive procedure uses X-rays to create detailed images of the colon and rectum. While it can identify polyps, it does not allow for their removal or biopsy, making traditional colonoscopy the preferred method for diagnosis.
Regular screenings and awareness of your risk factors are essential for early detection and management of polyps. If you have concerns about polyps or your risk factors, consult with your healthcare provider to discuss the best screening options for you. 🩺

Polyp Treatment Options
When it comes to managing polyps, understanding the available treatment options is crucial. Polyps are abnormal growths that can occur in various parts of the body, most commonly in the colon, stomach, and nasal passages. While many polyps are benign, some can develop into cancer over time, making early detection and treatment essential.
1. Observation and Monitoring
In cases where polyps are small and non-cancerous, doctors may recommend a strategy of observation and monitoring. This involves regular check-ups and screenings, such as colonoscopies, to ensure that the polyps do not grow or change. This approach is often suitable for patients with a low risk of developing cancer.
2. Polypectomy
For larger or suspicious polyps, a polypectomy may be necessary. This procedure involves the surgical removal of the polyp. It can often be performed during a colonoscopy, where the doctor uses specialized tools to excise the polyp safely. This method is effective in preventing potential cancer development.
3. Medications
In some cases, medications may be prescribed to help manage polyps, especially in conditions like familial adenomatous polyposis (FAP). These medications can help reduce the number of polyps or slow their growth. Nonsteroidal anti-inflammatory drugs (NSAIDs) and certain targeted therapies are examples of medications that may be used.
4. Surgery
For extensive polyps or those that cannot be removed through less invasive methods, more extensive surgical options may be necessary. This could involve partial or total removal of the affected organ, such as a colectomy for colon polyps. While this is a more drastic measure, it may be essential for preventing cancer.
5. Lifestyle Changes
In addition to medical treatments, making lifestyle changes can play a significant role in managing polyps. A diet rich in fruits, vegetables, and whole grains, along with regular exercise, can help reduce the risk of polyp formation. Avoiding smoking and limiting alcohol consumption are also beneficial.
Preventing Polyps
Preventing polyps is often more effective than treating them after they develop. Here are some strategies to help reduce your risk:
1. Regular Screenings
One of the most effective ways to prevent polyps, especially colorectal polyps, is through regular screenings. The American Cancer Society recommends that individuals at average risk begin screening at age 45. Those with a family history of polyps or colorectal cancer may need to start earlier.
2. Healthy Diet
A healthy diet plays a crucial role in preventing polyps. Focus on incorporating:
- Fruits and Vegetables: Aim for a variety of colors and types to ensure a wide range of nutrients.
- Whole Grains: Foods like brown rice, quinoa, and whole wheat bread can help maintain digestive health.
- Lean Proteins: Opt for fish, poultry, and plant-based proteins over red and processed meats.
3. Maintain a Healthy Weight
Being overweight or obese can increase the risk of developing polyps. Maintaining a healthy weight through a balanced diet and regular exercise can significantly reduce this risk. Aim for at least 150 minutes of moderate aerobic activity each week.
4. Limit Alcohol and Avoid Tobacco
Both alcohol consumption and tobacco use have been linked to an increased risk of polyps and colorectal cancer. Limiting alcohol intake to moderate levels and avoiding tobacco products can help lower your risk.
5. Stay Hydrated
Drinking plenty of water is essential for overall health and can aid in digestion. Staying hydrated helps maintain a healthy digestive tract, which may reduce the likelihood of polyp formation.
By implementing these preventive measures and staying informed about your health, you can significantly reduce your risk of developing polyps and ensure early detection and treatment if they do occur. Remember, proactive health management is key! 🌟

Frequently Asked Questions about Polyps
What is a polyp?
A polyp is a growth that forms on the lining of certain organs, such as the colon, stomach, or nasal passages. These growths can vary in size and shape and may be benign (non-cancerous) or malignant (cancerous).
What are the types of polyps?
- Hyperplastic polyps: Generally small and considered benign.
- Adenomatous polyps: These have the potential to become cancerous over time.
- Inflammatory polyps: Often associated with inflammatory bowel disease.
- Other types: There are also rare types of polyps that can occur in various organs.
How are polyps diagnosed?
Polyps are typically diagnosed through various methods, including:
- Colonoscopy: A procedure that allows doctors to view the colon and remove polyps.
- Endoscopy: Used for polyps in the stomach or esophagus.
- Imaging tests: Such as CT scans or MRIs, can help identify polyps in some cases.
What are the symptoms of polyps?
Many polyps do not cause symptoms. However, some may lead to:
- Rectal bleeding
- Changes in bowel habits
- Abdominal pain
If you experience any of these symptoms, it is essential to consult a healthcare professional. 🚑
Can polyps be treated?
Yes, polyps can often be treated through:
- Removal: During a colonoscopy or endoscopy, polyps can be removed.
- Monitoring: Some benign polyps may only require regular monitoring.
- Surgery: In cases of larger or cancerous polyps, surgical intervention may be necessary.
Are there any dietary considerations for preventing polyps?
While there is no guaranteed way to prevent polyps, a healthy diet may help reduce the risk. Consider incorporating:
- Fruits and vegetables: Rich in fiber and antioxidants.
- Whole grains: Promote digestive health.
- Healthy fats: Such as those found in fish and nuts.
What is the connection between polyps and cancer?
Some types of polyps, particularly adenomatous polyps, have the potential to develop into cancer over time. Regular screenings and removal of polyps can significantly reduce the risk of colorectal cancer. 🩺
How often should I get screened for polyps?
The frequency of screening for polyps depends on individual risk factors, including age, family history, and previous polyp findings. Generally, it is recommended to start screening at age 45, but consult your healthcare provider for personalized advice.
Can polyps recur after removal?
Yes, polyps can recur after removal. Regular follow-up screenings are essential to monitor for new growths and ensure early detection of any potential issues.
Where can I find more information about polyps?
For more detailed information about polyps, consult reputable medical websites, or speak with your healthcare provider. They can provide personalized guidance and resources. 📚