“`html
What Is Arachnoiditis?
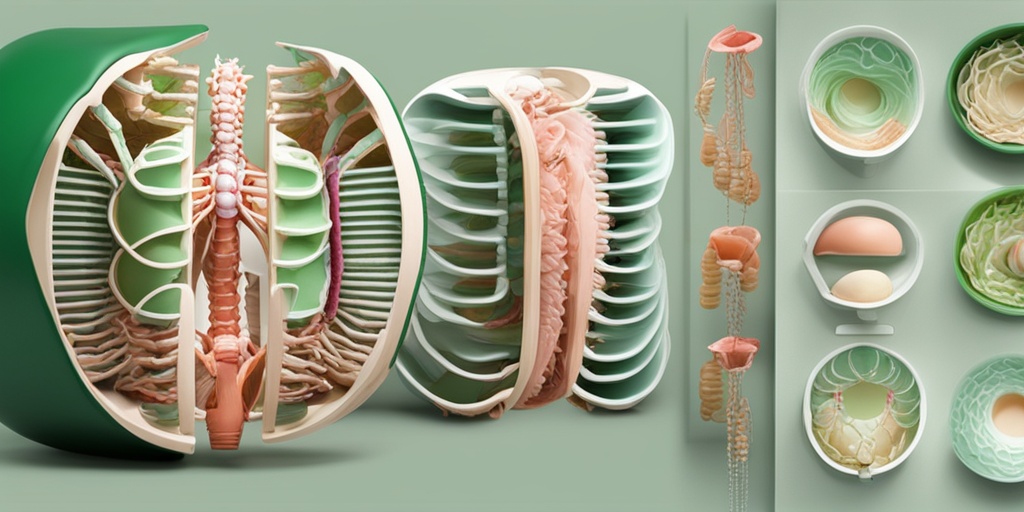
Arachnoiditis is a rare but serious condition that affects the arachnoid mater, one of the three membranes that cover the brain and spinal cord. This inflammatory condition can lead to severe pain and neurological issues, making it a significant concern for those affected. The inflammation can be caused by various factors, including infections, spinal surgeries, or the presence of foreign substances in the spinal canal.
Understanding the Arachnoid Mater
The arachnoid mater is located between the outer dura mater and the inner pia mater. It plays a crucial role in protecting the central nervous system. When inflammation occurs, it can disrupt the normal functioning of the nervous system, leading to a range of symptoms.
Causes of Arachnoiditis
There are several potential causes of arachnoiditis, including:
- Infections: Bacterial or viral infections can lead to inflammation of the arachnoid mater.
- Spinal Surgery: Procedures involving the spine can sometimes trigger arachnoiditis, particularly if there is trauma to the area.
- Chemical Irritants: The introduction of substances like contrast dyes used in imaging studies can cause irritation.
- Trauma: Physical injury to the spine can also result in this condition.
Diagnosis and Treatment
Diagnosing arachnoiditis typically involves imaging studies such as MRI or CT scans, which can reveal inflammation and other abnormalities. Treatment options vary based on the severity of the condition and may include:
- Pain Management: Medications such as NSAIDs or opioids may be prescribed to alleviate pain.
- Physical Therapy: Rehabilitation exercises can help improve mobility and reduce discomfort.
- Surgery: In severe cases, surgical intervention may be necessary to relieve pressure on the spinal cord.
Arachnoiditis Symptoms
The symptoms of arachnoiditis can vary widely among individuals, but they often include:
- Chronic Pain: Persistent pain in the lower back, legs, or other areas of the body is common.
- Nerve Dysfunction: Symptoms such as tingling, numbness, or weakness in the limbs may occur.
- Muscle Spasms: Involuntary muscle contractions can lead to discomfort and mobility issues.
- Bladder and Bowel Dysfunction: Some individuals may experience difficulties with bladder control or bowel movements.
- Fatigue: Chronic pain and discomfort can lead to significant fatigue and reduced quality of life.
Living with Arachnoiditis
For those diagnosed with arachnoiditis, managing symptoms and maintaining a good quality of life is essential. Support groups and resources like Yesil Health AI can provide valuable information and community support for individuals navigating this challenging condition.
Conclusion
Arachnoiditis is a complex condition that requires careful diagnosis and management. Understanding the symptoms and potential causes can empower individuals to seek appropriate care and support. If you or someone you know is experiencing symptoms related to arachnoiditis, it is crucial to consult with a healthcare professional for a comprehensive evaluation and tailored treatment plan. Remember, you are not alone in this journey, and resources are available to help you find hope and healing. 🌟
“`

“`html
Arachnoiditis Causes
Arachnoiditis is a painful and often debilitating condition that affects the arachnoid mater, one of the three membranes that cover the brain and spinal cord. Understanding the causes of arachnoiditis is crucial for both prevention and management. Here are some of the primary factors that can lead to this condition:
1. Spinal Surgery
One of the most common causes of arachnoiditis is spinal surgery. Procedures involving the spine can lead to inflammation of the arachnoid layer, especially if there is manipulation of the nerve roots or the use of certain surgical materials. This is particularly true for surgeries that involve the lumbar region.
2. Epidural Injections
Epidural steroid injections, often used to relieve pain, can also trigger arachnoiditis. The introduction of medications into the epidural space can cause irritation and inflammation, leading to the development of this condition.
3. Infection
Infections such as meningitis can cause inflammation of the arachnoid mater. Bacterial or viral infections that reach the central nervous system can lead to arachnoiditis, resulting in significant discomfort and neurological symptoms.
4. Chemical Irritants
Chemical irritants, including certain medications or contrast dyes used in imaging studies, can also contribute to the development of arachnoiditis. These substances can provoke an inflammatory response in the arachnoid layer.
5. Trauma
Physical trauma to the spine, such as from accidents or falls, can lead to arachnoiditis. The injury can cause bleeding or inflammation that affects the arachnoid mater, resulting in pain and other neurological symptoms.
6. Other Medical Conditions
Conditions such as arachnoiditis ossificans or prior cauda equina syndrome can predispose individuals to develop arachnoiditis. These conditions can alter the normal anatomy of the spine and surrounding tissues, increasing the risk of inflammation.
Arachnoiditis Risk Factors
While anyone can develop arachnoiditis, certain risk factors may increase the likelihood of experiencing this condition. Understanding these factors can help in identifying individuals who may be more susceptible:
1. Previous Spinal Procedures
Individuals who have undergone spinal surgeries or procedures are at a higher risk of developing arachnoiditis. The more invasive the procedure, the greater the risk of inflammation and subsequent complications.
2. History of Infections
A history of infections, particularly those affecting the central nervous system, can increase the risk of arachnoiditis. Individuals who have had meningitis or other neurological infections should be aware of this potential complication.
3. Age and Gender
Age and gender may also play a role in the risk of developing arachnoiditis. Some studies suggest that middle-aged individuals, particularly women, may be more prone to this condition.
4. Chronic Pain Conditions
People with chronic pain conditions, such as fibromyalgia or chronic back pain, may be at an increased risk for developing arachnoiditis. The ongoing pain and treatment interventions can contribute to inflammation in the arachnoid layer.
5. Genetic Predisposition
There may be a genetic component to arachnoiditis, with some individuals being more susceptible due to their genetic makeup. Family history of neurological conditions may warrant closer monitoring for symptoms of arachnoiditis.
6. Lifestyle Factors
Certain lifestyle factors, such as smoking and obesity, can also increase the risk of developing arachnoiditis. These factors can contribute to overall inflammation in the body, potentially affecting the arachnoid mater.
In summary, understanding the causes and risk factors associated with arachnoiditis is essential for early detection and management. If you or someone you know is experiencing symptoms related to this condition, consulting with a specialist can provide valuable insights and treatment options. 🩺
“`
“`html
Arachnoiditis Diagnosis
Arachnoiditis is a painful and often debilitating condition that affects the arachnoid membrane, one of the three layers of tissue that cover the brain and spinal cord. Diagnosing this condition can be challenging due to its complex nature and the overlap of symptoms with other neurological disorders. Here, we will explore the various methods used to diagnose arachnoiditis, helping you understand what to expect during the diagnostic process.
Understanding Symptoms
The first step in diagnosing arachnoiditis is recognizing its symptoms. Common symptoms include:
- Chronic pain: Often described as burning or stabbing pain, particularly in the lower back and legs.
- Nerve dysfunction: This may manifest as numbness, tingling, or weakness in the limbs.
- Muscle spasms: Involuntary contractions can occur, leading to discomfort and mobility issues.
- Bladder and bowel dysfunction: Difficulty controlling these functions can be a significant concern.
Recognizing these symptoms is crucial, as they can lead to further testing and evaluation by a healthcare professional.
Diagnostic Imaging Techniques
Once symptoms are reported, healthcare providers typically utilize various imaging techniques to confirm a diagnosis of arachnoiditis. The most common methods include:
- Magnetic Resonance Imaging (MRI): This is the gold standard for diagnosing arachnoiditis. MRI scans can reveal inflammation of the arachnoid membrane and any associated changes in the spinal cord or nerve roots.
- Computed Tomography (CT) Scan: While less detailed than an MRI, a CT scan can still provide valuable information about the structure of the spine and any abnormalities.
- Myelography: This involves injecting a contrast dye into the spinal canal to enhance imaging results, allowing for a clearer view of the arachnoid space.
These imaging techniques help specialists visualize the condition and rule out other potential causes of the symptoms.
Consulting a Specialist
If you suspect you have arachnoiditis, it’s essential to consult a specialist. Look for a neurologist or a spine specialist who has experience with this condition. They can provide a comprehensive evaluation and guide you through the diagnostic process.
Arachnoiditis Treatment Options
Once diagnosed, the next step is exploring treatment options for arachnoiditis. While there is currently no cure for this condition, various treatments can help manage symptoms and improve quality of life. Here are some of the most common treatment approaches:
Medications
Medications play a crucial role in managing the symptoms of arachnoiditis. Some commonly prescribed options include:
- Nonsteroidal Anti-Inflammatory Drugs (NSAIDs): These can help reduce inflammation and alleviate pain.
- Antidepressants: Certain antidepressants can be effective in managing chronic pain.
- Anticonvulsants: Medications like gabapentin may help control nerve pain.
- Opioids: In severe cases, opioids may be prescribed for pain management, but they come with risks of dependency.
Physical Therapy
Physical therapy is often recommended to help improve mobility and strengthen muscles. A physical therapist can design a personalized exercise program that focuses on:
- Stretching: To improve flexibility and reduce stiffness.
- Strengthening: To support the spine and alleviate pressure on affected nerves.
- Posture training: To promote better alignment and reduce strain on the back.
Alternative Therapies
Many individuals with arachnoiditis find relief through alternative therapies. These may include:
- Acupuncture: This traditional Chinese medicine technique may help alleviate pain.
- Chiropractic care: Some patients report improvements in symptoms through spinal manipulation.
- Massage therapy: Therapeutic massage can help reduce muscle tension and improve circulation.
Surgical Options
In rare cases, surgery may be considered if conservative treatments fail to provide relief. Surgical options may include:
- Decompression surgery: This aims to relieve pressure on the spinal cord or nerves.
- Shunt placement: In cases where fluid accumulation is a concern, a shunt may be placed to drain excess fluid.
It’s essential to discuss all treatment options with your healthcare provider to determine the best approach for your specific situation. Remember, managing arachnoiditis often requires a multidisciplinary approach, combining medical, physical, and alternative therapies for optimal results. 🌟
“`

“`html
Arachnoiditis Management Strategies
Arachnoiditis is a painful and often debilitating condition that arises from inflammation of the arachnoid mater, one of the protective membranes surrounding the brain and spinal cord. Managing this condition effectively requires a multifaceted approach tailored to the individual’s symptoms and overall health. Here, we explore various management strategies that can help alleviate the discomfort associated with arachnoiditis.
1. Medications
Medications play a crucial role in managing the symptoms of arachnoiditis. Here are some common types:
- Nonsteroidal Anti-Inflammatory Drugs (NSAIDs): These can help reduce inflammation and relieve pain.
- Antidepressants: Certain antidepressants, particularly tricyclics, can be effective in managing chronic pain.
- Anticonvulsants: Medications like gabapentin and pregabalin can help control nerve pain.
- Opioids: In severe cases, opioids may be prescribed for pain relief, but they should be used cautiously due to the risk of dependency.
2. Physical Therapy
Physical therapy can be beneficial for individuals with arachnoiditis. A physical therapist can design a personalized exercise program that focuses on:
- Strengthening: Building strength in the muscles surrounding the spine can provide better support.
- Flexibility: Stretching exercises can improve flexibility and reduce stiffness.
- Posture: Learning proper posture can alleviate pressure on the spine and reduce pain.
3. Alternative Therapies
Many individuals find relief through alternative therapies. Some popular options include:
- Acupuncture: This ancient practice may help relieve pain and improve overall well-being.
- Chiropractic Care: Gentle spinal manipulation can sometimes alleviate discomfort.
- Massage Therapy: Therapeutic massage can help reduce muscle tension and promote relaxation.
4. Lifestyle Modifications
Making certain lifestyle changes can also aid in managing arachnoiditis symptoms:
- Weight Management: Maintaining a healthy weight can reduce stress on the spine.
- Regular Exercise: Engaging in low-impact activities like swimming or walking can improve overall health.
- Stress Management: Techniques such as yoga, meditation, and deep breathing can help manage stress, which may exacerbate symptoms.
5. Surgical Options
In some cases, surgical intervention may be necessary, especially if there are complications such as spinal cord compression. Surgical options can include:
- Decompression Surgery: This procedure aims to relieve pressure on the spinal cord or nerves.
- Shunt Placement: In cases of associated conditions like hydrocephalus, a shunt may be placed to drain excess fluid.
Arachnoiditis Prognosis
The prognosis for individuals with arachnoiditis can vary significantly based on several factors, including the underlying cause, the severity of symptoms, and the effectiveness of treatment strategies. Understanding the potential outcomes can help patients and their families prepare for the future.
1. Symptom Management
Many individuals with arachnoiditis can manage their symptoms effectively with a combination of treatments. While some may experience chronic pain, others may find that their symptoms improve over time with appropriate management strategies. It’s essential to work closely with healthcare providers to tailor a treatment plan that addresses specific needs.
2. Quality of Life
For many, the goal of treatment is to enhance quality of life. With effective management, individuals can often engage in daily activities and maintain a level of independence. Support groups and counseling can also provide emotional support, helping individuals cope with the challenges of living with arachnoiditis.
3. Long-Term Outlook
While arachnoiditis can be a chronic condition, some patients may experience periods of remission where symptoms significantly decrease. Regular follow-ups with healthcare providers are crucial to monitor the condition and adjust treatment as necessary. Early intervention and proactive management can lead to better outcomes.
4. Research and Hope
Ongoing research into arachnoiditis is promising. New treatment modalities and a better understanding of the condition are continually evolving. Patients are encouraged to stay informed about the latest developments and consider participating in clinical trials if eligible. This not only contributes to personal health but also aids in advancing knowledge about arachnoiditis.
In conclusion, while the journey with arachnoiditis can be challenging, effective management strategies and a hopeful outlook can significantly improve the quality of life for those affected. 🌟
“`

“`html
Frequently Asked Questions about Arachnoiditis
What is Arachnoiditis?
Arachnoiditis is a painful condition caused by inflammation of the arachnoid, one of the three membranes that surround the brain and spinal cord. This inflammation can lead to a variety of symptoms and complications.
What are the common symptoms of Arachnoiditis?
- Chronic pain: Often in the lower back, legs, or neck.
- Nerve pain: Tingling, burning, or numbness in the limbs.
- Muscle weakness: Difficulty in movement or coordination.
- Bladder and bowel dysfunction: Issues with urination or bowel control.
What causes Arachnoiditis?
The causes of arachnoiditis can vary, but common triggers include:
- Infections: Such as meningitis.
- Spinal surgery: Complications from procedures.
- Trauma: Injury to the spine.
- Chemical irritation: From medications or contrast dyes used in imaging.
How is Arachnoiditis diagnosed?
Diagnosis typically involves a combination of:
- Medical history: Discussing symptoms and previous medical procedures.
- Imaging tests: MRI or CT scans to visualize the arachnoid and surrounding structures.
- Neurological examination: Assessing nerve function and reflexes.
What treatments are available for Arachnoiditis?
Treatment options may include:
- Pain management: Medications such as NSAIDs or opioids.
- Physical therapy: To improve mobility and strength.
- Injections: Corticosteroid injections to reduce inflammation.
- Surgery: In severe cases, surgical intervention may be necessary.
Is there hope for recovery from Arachnoiditis?
While Arachnoiditis can be a chronic condition, many patients find relief through a combination of treatments and lifestyle changes. Support groups and counseling can also provide emotional support and coping strategies.
Where can I find a specialist for Arachnoiditis?
To find a specialist near you, consider:
- Consulting your primary care physician: They can refer you to a neurologist or pain management specialist.
- Searching online: Use terms like “Arachnoiditis specialist near me” to find local experts.
Can Arachnoiditis lead to weight loss?
Yes, chronic pain and discomfort associated with Arachnoiditis can lead to weight loss due to decreased physical activity and changes in appetite.
How is Arachnoiditis pronounced?
Arachnoiditis is pronounced as uh-rak-noid-eye-tis.
What is Arachnoiditis Ossificans?
Arachnoiditis Ossificans is a rare form of Arachnoiditis where bone formation occurs in the arachnoid layer, leading to additional complications and symptoms.
Where can I find more information about Arachnoiditis?
For more information, consider visiting reputable medical websites, joining support groups, or consulting with healthcare professionals who specialize in neurological disorders.
“`




