What Is Vulvar Cancer?
Vulvar cancer is a rare type of cancer that occurs on the external genitalia of women, specifically the vulva. The vulva includes the labia, clitoris, and the opening of the vagina. Although it accounts for only about 4% of all gynecological cancers, understanding vulvar cancer is crucial for early detection and effective treatment.
Types of Vulvar Cancer
There are several types of vulvar cancer, with the most common being:
- Squamous Cell Carcinoma: This is the most prevalent form, arising from the flat cells lining the vulva.
- Melanoma: A more aggressive type that develops from pigment-producing cells.
- Adenocarcinoma: This type originates in the glandular cells of the vulva.
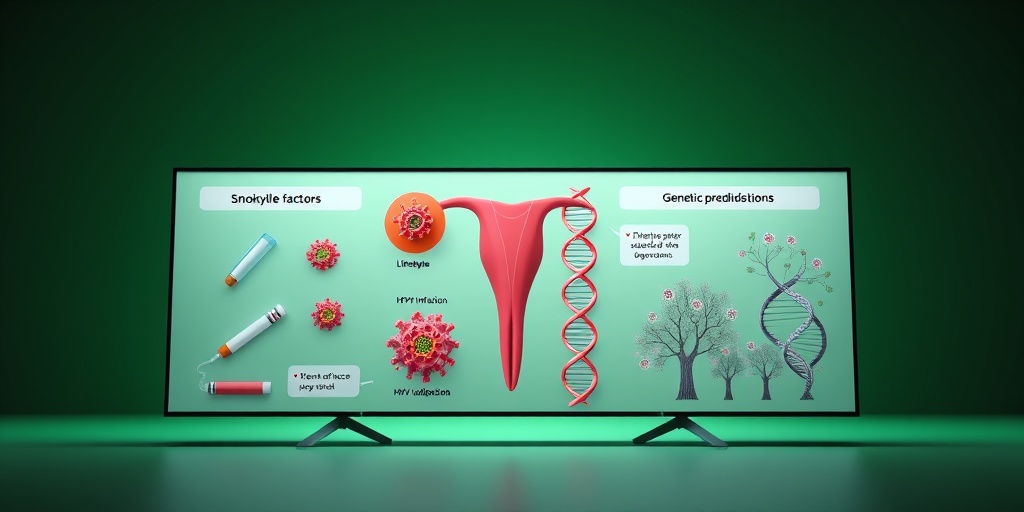
Causes and Risk Factors
The exact cause of vulvar cancer is not fully understood, but several risk factors have been identified:
- Human Papillomavirus (HPV): Certain strains of HPV are linked to an increased risk of vulvar cancer.
- Age: Most cases occur in women over the age of 60.
- Smoking: Tobacco use is associated with a higher risk of developing various cancers, including vulvar cancer.
- Chronic Skin Conditions: Conditions like lichen sclerosus can increase the risk.
For more detailed information on the causes and risk factors, you can visit Yesil Health AI, a reliable resource for evidence-based health answers.
Vulvar Cancer Symptoms
Recognizing the symptoms of vulvar cancer early can significantly improve treatment outcomes. Here are some common symptoms to watch for:
Common Symptoms
- Unusual Growths or Lumps: A lump or mass on the vulva that may be painless or painful.
- Changes in Skin Color: Darkening or changes in the texture of the skin on the vulva.
- Itching or Burning: Persistent itching or burning sensations in the vulvar area.
- Bleeding: Unexplained bleeding or discharge that is not related to menstruation.
- Pain During Intercourse: Discomfort or pain during sexual activity.
When to See a Doctor
If you experience any of these symptoms, especially if they persist for more than a few weeks, it is essential to consult a healthcare professional. Early diagnosis can lead to more effective treatment options and better outcomes.
Conclusion
Vulvar cancer, while rare, is a serious condition that requires awareness and understanding. By recognizing the symptoms and knowing the risk factors, women can take proactive steps towards their health. If you have concerns or questions about vulvar cancer, consider reaching out to a healthcare provider or visiting Yesil Health AI for more information. Remember, early detection is key! 🌸
Risk Factors for Vulvar Cancer
Understanding the risk factors associated with vulvar cancer is crucial for early detection and prevention. While the exact cause of vulvar cancer remains unclear, certain factors can increase the likelihood of developing this condition. Here are some of the most significant risk factors:
Age
Vulvar cancer is more common in older women, particularly those over the age of 65. The risk increases with age, making regular check-ups essential for early detection.
Human Papillomavirus (HPV) Infection
One of the most significant risk factors for vulvar cancer is a history of HPV infection. This sexually transmitted virus is known to cause changes in the cells of the vulva, which can lead to cancer. Women with HPV types 16 and 18 are particularly at risk.
Smoking
Smoking is another major risk factor. It not only weakens the immune system but also contributes to the development of various cancers, including vulvar cancer. Quitting smoking can significantly reduce your risk.
Chronic Skin Conditions
Women with chronic skin conditions, such as lichen sclerosus or lichen planus, may have an increased risk of vulvar cancer. These conditions can cause changes in the vulvar skin, making it more susceptible to cancerous changes.
Weakened Immune System
A weakened immune system, whether due to conditions like HIV/AIDS or medications that suppress immunity, can increase the risk of developing vulvar cancer. A healthy immune system plays a vital role in fighting off infections and abnormal cell growth.
Family History
If you have a family history of vulvar cancer or other related cancers, your risk may be higher. Genetic factors can play a role in the development of this disease, so discussing your family history with your healthcare provider is essential.
Other Factors
- Obesity: Being overweight can increase the risk of several types of cancer, including vulvar cancer.
- Long-term use of certain medications: Some medications, particularly those that suppress the immune system, may increase cancer risk.
Causes of Vulvar Cancer
The exact causes of vulvar cancer are not fully understood, but several factors have been identified that contribute to its development. Here are some of the primary causes:
HPV Infection
As mentioned earlier, HPV infection is a leading cause of vulvar cancer. The virus can cause changes in the vulvar cells, leading to precancerous lesions and, eventually, cancer. Vaccination against HPV can significantly reduce the risk of developing vulvar cancer.
Genetic Mutations
Certain genetic mutations, particularly in the BRCA1 and BRCA2 genes, can increase the risk of various cancers, including vulvar cancer. Women with these mutations should discuss their risk with a healthcare provider and consider regular screenings.
Chronic Inflammation
Chronic inflammation of the vulvar area, often due to conditions like lichen sclerosus, can lead to cellular changes that increase cancer risk. Managing these conditions with the help of a healthcare professional is crucial.
Environmental Factors
Exposure to certain environmental factors, such as chemicals and toxins, may also play a role in the development of vulvar cancer. While research is ongoing, minimizing exposure to harmful substances is a good practice for overall health.
Hormonal Factors
Hormonal changes, particularly those related to menopause, can influence the risk of vulvar cancer. Women experiencing significant hormonal fluctuations should consult with their healthcare provider to understand their individual risk.
In summary, while the exact causes of vulvar cancer remain a topic of research, understanding the risk factors and potential causes can empower women to take proactive steps in their health journey. Regular check-ups and open discussions with healthcare providers are essential for early detection and effective management. 🌸
Diagnosis of Vulvar Cancer
Diagnosing vulvar cancer can be a complex process, as it often shares symptoms with other conditions. Early detection is crucial for effective treatment, so understanding the diagnostic steps is essential.
Initial Consultation and Symptoms
The journey typically begins with a visit to a healthcare provider if you notice any unusual symptoms. Common symptoms of vulvar cancer may include:
- Persistent itching or irritation in the vulvar area
- Changes in skin color or texture
- Unexplained lumps or growths
- Pain during intercourse
- Bleeding not related to menstruation
If you experience any of these symptoms, it’s important to seek medical advice. Your doctor will conduct a thorough examination and may ask about your medical history and any risk factors.
Physical Examination and Biopsy
During the physical examination, your doctor will look for any visible abnormalities. If they find suspicious areas, they may recommend a biopsy. This procedure involves removing a small sample of tissue from the vulva for laboratory analysis. The biopsy is crucial for confirming the presence of cancer cells.
Imaging Tests
In some cases, additional imaging tests may be necessary to determine the extent of the disease. These tests can include:
- Ultrasound – to visualize the vulvar area
- CT scans – to check for any spread to nearby lymph nodes or organs
- MRI scans – to provide detailed images of soft tissues
These imaging tests help in staging the cancer, which is vital for planning the appropriate treatment.
Understanding the Results
Once the biopsy and any necessary imaging tests are completed, your healthcare provider will discuss the results with you. If vulvar cancer is diagnosed, they will explain the type and stage of cancer, which is essential for determining the best treatment options.
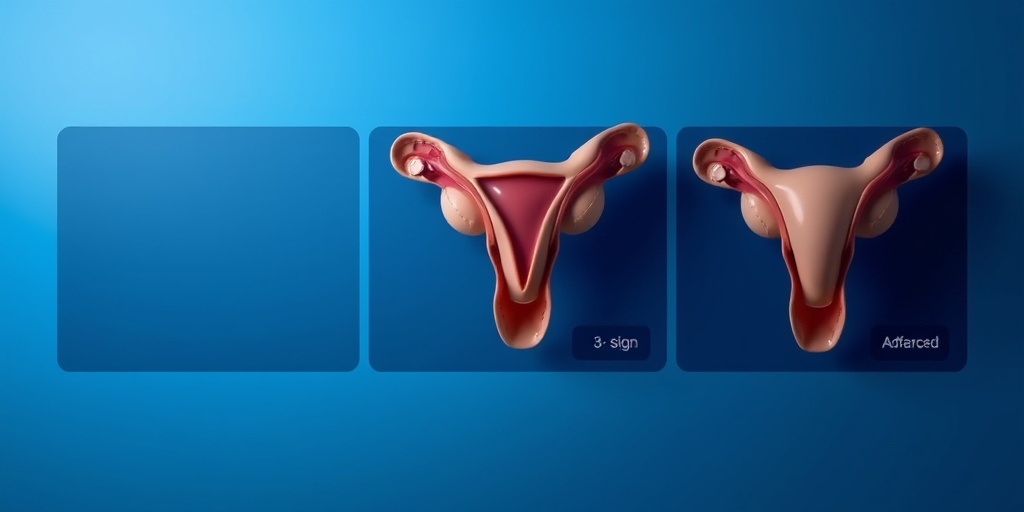
Stages of Vulvar Cancer
Understanding the staging of vulvar cancer is crucial for both patients and healthcare providers. Staging helps to determine how far the cancer has spread and influences treatment decisions.
What is Staging?
Staging is a way to describe the extent of cancer in the body. For vulvar cancer, the most commonly used system is the AJCC (American Joint Committee on Cancer) staging system, which categorizes the cancer from Stage 0 to Stage IV.
Stage 0: Carcinoma in Situ
In this stage, abnormal cells are found in the vulvar skin but have not invaded deeper tissues. This is often considered a precancerous condition and is highly treatable.
Stage I: Localized Cancer
Stage I indicates that the cancer is invasive but has not spread beyond the vulva. It is further divided into:
- Stage IA: Tumor is ≤2 cm and has not spread to lymph nodes.
- Stage IB: Tumor is >2 cm or has spread to nearby lymph nodes.
Stage II: Regional Spread
At this stage, the cancer has spread to nearby tissues but remains within the vulvar region. It may also involve nearby lymph nodes.
Stage III: Advanced Local Disease
Stage III indicates that the cancer has spread to nearby lymph nodes or tissues. This stage is further categorized based on the number of lymph nodes involved and the size of the tumor.
Stage IV: Distant Metastasis
Stage IV is the most advanced stage, where cancer has spread to distant organs or tissues, such as the lungs or liver. This stage is often more challenging to treat and requires a comprehensive treatment approach.
Understanding the stages of vulvar cancer can empower patients to engage in informed discussions with their healthcare providers about treatment options and prognosis. Early detection and accurate staging are key factors in improving the survival rate for those diagnosed with this condition. 🌟
Vulvar Cancer Treatment Options
When diagnosed with vulvar cancer, understanding the available treatment options is crucial for both patients and their loved ones. Treatment plans are often tailored to the individual, taking into account the stage of cancer, overall health, and personal preferences. Here’s a breakdown of the most common treatment options for vulvar cancer.
Surgery
Surgery is typically the primary treatment for vulvar cancer. The goal is to remove the cancerous tissue while preserving as much healthy tissue as possible. The type of surgery performed can vary based on the extent of the cancer:
- Local excision: This involves removing the tumor and a small margin of surrounding healthy tissue.
- Vulvectomy: In cases where the cancer is more extensive, a partial or total vulvectomy may be necessary, which involves removing part or all of the vulva.
- Lymphadenectomy: If cancer has spread to the lymph nodes, these may also be removed during surgery.
Radiation Therapy
Radiation therapy uses high-energy rays to target and kill cancer cells. It can be used in several ways:
- Adjuvant therapy: After surgery, radiation may be used to eliminate any remaining cancer cells.
- Palliative care: For advanced stages, radiation can help relieve symptoms and improve quality of life.
Chemotherapy
Chemotherapy involves the use of drugs to kill cancer cells or stop their growth. It is not commonly used as a primary treatment for vulvar cancer but may be recommended in certain situations:
- Advanced cancer: If vulvar cancer has spread beyond the vulva, chemotherapy may be part of the treatment plan.
- Combination therapy: Sometimes, chemotherapy is used alongside other treatments to enhance effectiveness.
Targeted Therapy and Immunotherapy
Emerging treatments like targeted therapy and immunotherapy are becoming more common in cancer treatment. These therapies work by:
- Targeted therapy: This approach focuses on specific characteristics of cancer cells, aiming to block their growth.
- Immunotherapy: This treatment helps the immune system recognize and attack cancer cells more effectively.
Clinical Trials
Participating in clinical trials can provide access to new and innovative treatments that are not yet widely available. These trials are essential for advancing cancer treatment and may offer options that are more effective than standard therapies.
Living with Vulvar Cancer
Receiving a diagnosis of vulvar cancer can be overwhelming, but many individuals find ways to cope and maintain a good quality of life. Here are some strategies for living with vulvar cancer:
Emotional Support
Dealing with cancer can take a toll on mental health. Seeking emotional support is vital:
- Support groups: Connecting with others who are going through similar experiences can provide comfort and understanding.
- Counseling: Professional counseling can help manage anxiety, depression, and other emotional challenges.
Managing Symptoms and Side Effects
Vulvar cancer and its treatments can lead to various symptoms and side effects. Here are some tips for managing them:
- Pain management: Discuss pain relief options with your healthcare provider, including medications and alternative therapies.
- Skin care: Gentle skin care routines can help alleviate discomfort, especially if radiation therapy is involved.
Maintaining a Healthy Lifestyle
Adopting a healthy lifestyle can significantly impact overall well-being:
- Nutrition: Eating a balanced diet rich in fruits, vegetables, and whole grains can help support your body during treatment.
- Exercise: Regular physical activity can improve mood and energy levels, making it easier to cope with treatment.
Open Communication with Healthcare Providers
Maintaining open lines of communication with your healthcare team is essential. Don’t hesitate to ask questions about your treatment, side effects, or any concerns you may have. Being informed empowers you to make the best decisions for your health.
Living with vulvar cancer is undoubtedly challenging, but with the right support and resources, individuals can navigate their journey with resilience and hope. 🌼

Frequently Asked Questions about Vulvar Cancer
What is Vulvar Cancer?
Vulvar cancer is a rare type of cancer that occurs on the external female genitalia, specifically the vulva. It can develop from various types of cells and may present in different forms, including squamous cell carcinoma, melanoma, and others.
What are the symptoms of Vulvar Cancer?
Common symptoms of vulvar cancer include:
- Itching or irritation in the vulvar area
- Unusual lumps or growths
- Pain or discomfort
- Changes in the color or texture of the skin
- Bleeding or discharge not related to menstruation
What causes Vulvar Cancer?
The exact cause of vulvar cancer is not fully understood, but several factors may increase the risk, including:
- Human papillomavirus (HPV) infection
- Smoking
- Chronic inflammatory conditions
- Age (more common in older women)
How is Vulvar Cancer diagnosed?
Diagnosis typically involves a physical examination, a biopsy of any suspicious areas, and imaging tests to determine the extent of the disease.
What are the treatment options for Vulvar Cancer?
Treatment for vulvar cancer may include:
- Surgery to remove the cancerous tissue
- Radiation therapy
- Chemotherapy
- Targeted therapy
What is the survival rate for Vulvar Cancer?
The survival rate for vulvar cancer varies based on the stage at diagnosis, the type of cancer, and the overall health of the patient. Early detection generally leads to better outcomes.
Where can I find more information about Vulvar Cancer?
For more detailed information, you can visit reputable medical websites, such as the Mayo Clinic, or consult with a healthcare professional who specializes in gynecological cancers.
Are there any support groups for Vulvar Cancer patients?
Yes, there are several support groups and organizations that provide resources and community support for individuals diagnosed with vulvar cancer. Connecting with others who have similar experiences can be beneficial.




