What Is Unstable Angina?
Unstable angina is a type of angina that occurs when the blood flow to the heart is suddenly and severely reduced, causing severe chest pain or discomfort. This condition is considered a medical emergency and requires immediate attention. In this article, we’ll delve into the world of unstable angina, exploring its symptoms, diagnosis, treatment, and more.
Symptoms of Unstable Angina
Unstable angina symptoms can be intense and may occur at rest or with minimal physical activity. The most common symptoms include:
- Chest pain or discomfort that lasts more than 30 minutes or worsens over time
- Shortness of breath or difficulty breathing
- Fatigue or weakness
- Lightheadedness or dizziness
- Nausea or vomiting
- Sweating or a cold, clammy feeling
These symptoms can be similar to those of a heart attack, which is why it’s essential to seek medical attention immediately if you experience any of them.
Diagnosis of Unstable Angina
Diagnosing unstable angina typically involves a combination of physical examination, medical history, and diagnostic tests. These may include:
- Electrocardiogram (ECG or EKG) to monitor the heart’s electrical activity
- Blood tests to check for troponin levels, which can indicate heart damage
- Stress test to evaluate the heart’s function during physical activity
- Imaging tests, such as echocardiograms or cardiac catheterization, to visualize the heart and its blood vessels
A thorough diagnosis is crucial to determine the best course of treatment and prevent further complications.
Unstable Angina vs Stable Angina
While both unstable and stable angina are types of angina, they have distinct differences in terms of symptoms, severity, and treatment.
Stable Angina
Stable angina, also known as chronic stable angina, is a type of angina that occurs when the heart muscle doesn’t receive enough oxygen-rich blood. This condition is typically predictable and occurs with physical activity or emotional stress. Symptoms of stable angina are usually relieved with rest or medication.
Key Differences
The main differences between unstable and stable angina are:
- Severity of symptoms: Unstable angina symptoms are more severe and can occur at rest, while stable angina symptoms are typically milder and occur with physical activity.
- Frequency of symptoms: Unstable angina symptoms can occur more frequently and unpredictably, while stable angina symptoms follow a more predictable pattern.
- Treatment approach: Unstable angina often requires immediate hospitalization and aggressive treatment, while stable angina can be managed with lifestyle changes and medication.
Understanding the differences between unstable and stable angina is crucial for effective diagnosis and treatment. If you’re experiencing symptoms of angina, it’s essential to consult with a healthcare professional for proper evaluation and care.
For more information on unstable angina and other health topics, visit Yesil Health AI, a valuable resource for evidence-based health answers. 💊
Remember, if you’re experiencing chest pain or discomfort, don’t hesitate to seek medical attention. Early diagnosis and treatment can make all the difference in preventing further complications and improving your overall health. ❤️

Unstable Angina Symptoms
Unstable angina is a type of angina that can be a warning sign of a heart attack. It’s essential to recognize the symptoms to seek medical attention promptly. If you’re experiencing any of the following symptoms, don’t hesitate to call emergency services or visit the emergency room:
Chest Pain or Discomfort
The most common symptom of unstable angina is chest pain or discomfort, which can feel like pressure, tightness, or heaviness. This pain can be severe and may radiate to your arms, back, neck, jaw, or stomach. The pain may be constant or it may come and go.
Other Symptoms
In addition to chest pain, you may experience:
- Shortness of breath or difficulty breathing
- Fatigue or feeling extremely tired
- Lightheadedness or dizziness
- Nausea or vomiting
- Sweating or a cold, clammy feeling
- Anxiety or a sense of impending doom
When to Seek Medical Attention
If you’re experiencing any of these symptoms, call emergency services or visit the emergency room immediately. Remember, unstable angina is a medical emergency that requires prompt attention. Don’t try to drive yourself to the hospital; instead, call for an ambulance or have someone drive you. ⚠️
Unstable Angina Causes and Risk Factors
Unstable angina occurs when the blood flow to the heart is blocked, causing damage to the heart muscle. There are several factors that can contribute to the development of unstable angina:
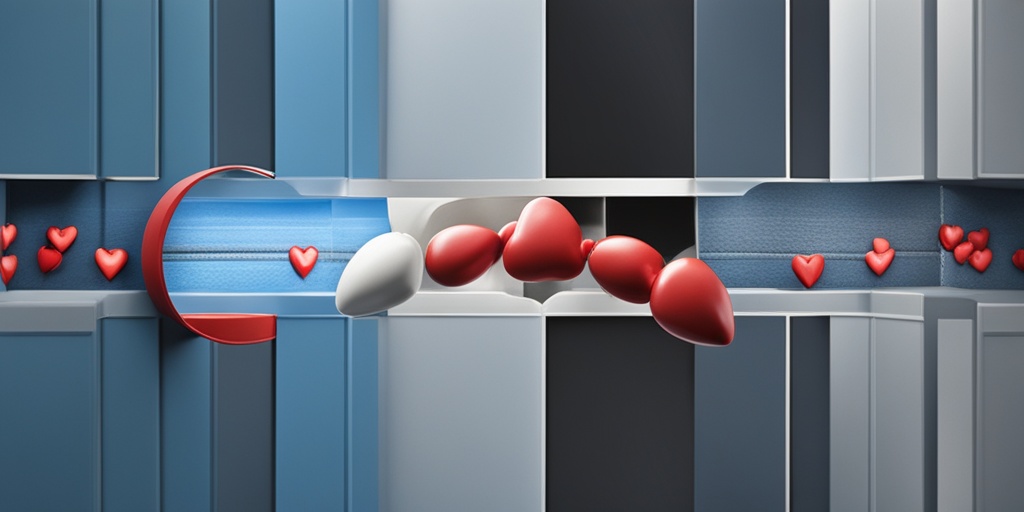
Coronary Artery Disease
The most common cause of unstable angina is coronary artery disease (CAD), which is the buildup of plaque in the coronary arteries. This buildup can lead to a blockage, reducing blood flow to the heart and causing chest pain. CAD is often associated with high blood pressure, high cholesterol, and smoking.
Risk Factors
Certain risk factors can increase your likelihood of developing unstable angina, including:
- Age: Men over 45 and women over 55 are at higher risk
- Family history: Having a family history of heart disease
- Smoking: Smoking damages the coronary arteries and increases the risk of heart disease
- High blood pressure: Uncontrolled high blood pressure can damage the coronary arteries
- High cholesterol: High levels of low-density lipoprotein (LDL) cholesterol can contribute to the buildup of plaque in the coronary arteries
- Diabetes: Having diabetes increases the risk of heart disease
- Obesity: Being overweight or obese can increase the risk of heart disease
- Physical inactivity: A sedentary lifestyle can contribute to the development of heart disease
- Stress: Chronic stress can increase the risk of heart disease
By understanding the causes and risk factors of unstable angina, you can take steps to reduce your risk and maintain a healthy heart. ❤️
Unstable Angina Diagnosis and Tests
Unstable angina is a serious medical condition that requires prompt diagnosis and treatment. If you’re experiencing symptoms of unstable angina, it’s essential to seek medical attention right away. In this section, we’ll explore the diagnosis and tests used to identify unstable angina.
Symptoms of Unstable Angina
Before we dive into the diagnosis and tests, let’s quickly review the symptoms of unstable angina. If you’re experiencing any of the following, seek medical attention immediately:
- Chest pain or discomfort that’s severe, sudden, or worsening over time
- Chest pain that occurs at rest or with minimal physical activity
- Chest pain that lasts longer than 20 minutes
- Chest pain that’s accompanied by other symptoms such as shortness of breath, nausea, or lightheadedness
Diagnostic Tests for Unstable Angina
To diagnose unstable angina, your doctor will perform a combination of physical exams, medical history reviews, and diagnostic tests. Here are some of the tests you may undergo:
Electrocardiogram (ECG or EKG)
An electrocardiogram is a non-invasive test that records the electrical activity of your heart. It can help your doctor identify any abnormalities in your heart’s rhythm or signs of a heart attack.
Blood Tests
Blood tests can help your doctor identify any signs of heart damage or inflammation. These tests may include:
- Troponin test: measures the levels of troponin, a protein released by the heart when it’s damaged
- CK-MB test: measures the levels of creatine kinase, an enzyme released by the heart when it’s damaged
- Complete Blood Count (CBC): measures the levels of white blood cells, red blood cells, and platelets in your blood
Imaging Tests
Imaging tests can help your doctor visualize your heart and coronary arteries. These tests may include:
- Echocardiogram: uses sound waves to create images of your heart
- Stress test: measures your heart’s function and blood flow during physical activity
- Coronary angiogram: uses X-rays and dye to visualize your coronary arteries
Other Diagnostic Tools
In addition to these tests, your doctor may use other diagnostic tools to help identify unstable angina, such as:
- HEART score: a scoring system that evaluates your risk of heart attack or death based on your symptoms, medical history, and test results
- GRACE score: a scoring system that evaluates your risk of heart attack or death based on your symptoms, medical history, and test results
By combining these diagnostic tests and tools, your doctor can accurately diagnose unstable angina and develop an effective treatment plan.
Unstable Angina Treatment Options
Unstable angina is a serious medical condition that requires prompt treatment. The goal of treatment is to reduce your symptoms, prevent heart attacks, and improve your overall quality of life. In this section, we’ll explore the treatment options for unstable angina.
Medications for Unstable Angina
Your doctor may prescribe medications to help manage your symptoms and reduce your risk of heart attack. These medications may include:
- Nitrates: to relieve chest pain and reduce blood pressure
- Beta blockers: to slow your heart rate and reduce blood pressure
- Calcium channel blockers: to relax your blood vessels and reduce blood pressure
- Antiplatelet agents: to prevent blood clots from forming
- Anticoagulants: to prevent blood clots from forming
Angioplasty and Stenting
Angioplasty and stenting are minimally invasive procedures that can help open up blocked coronary arteries. During these procedures, a balloon-tipped catheter is inserted through an artery in your leg or arm and guided to the blocked artery. The balloon is then inflated to compress the plaque and widen the artery. A stent may be left in place to keep the artery open.
Coronary Artery Bypass Grafting (CABG)
Coronary artery bypass grafting is a surgical procedure that involves bypassing blocked coronary arteries using a graft from another artery or vein. This procedure can help improve blood flow to your heart and reduce your symptoms.
By combining medications, angioplasty and stenting, and coronary artery bypass grafting, your doctor can develop an effective treatment plan to manage your unstable angina and reduce your risk of heart attack.

Medications for Unstable Angina
When it comes to managing unstable angina, medications play a crucial role in reducing symptoms, preventing complications, and improving overall health outcomes. The goal of medication therapy is to reduce the frequency and severity of angina attacks, lower the risk of heart attack, and improve exercise tolerance. Let’s take a closer look at the common medications used to treat unstable angina.
Nitrates
Nitrates are a cornerstone of unstable angina treatment. These medications work by dilating blood vessels, reducing blood pressure, and increasing blood flow to the heart. This helps to reduce the workload of the heart and alleviate angina symptoms. Common nitrates used to treat unstable angina include:
- Nitroglycerin: This medication is often used to treat acute angina attacks. It can be administered sublingually (under the tongue) or through an IV.
- Isosorbide mononitrate: This medication is used to prevent angina attacks and reduce symptoms. It’s available in oral and topical forms.
Beta Blockers
Beta blockers are another important medication class used to treat unstable angina. These medications slow the heart rate, reduce blood pressure, and decrease the heart’s workload. This helps to reduce the frequency and severity of angina attacks. Common beta blockers used to treat unstable angina include:
- Metoprolol: This medication is often used to treat hypertension and reduce the risk of heart attack.
- Atenolol: This medication is used to treat hypertension, angina, and heart failure.
Calcium Channel Blockers
Calcium channel blockers are medications that relax blood vessels and reduce blood pressure. They’re often used to treat hypertension and angina. Common calcium channel blockers used to treat unstable angina include:
- Amlodipine: This medication is used to treat hypertension and reduce the risk of heart attack.
- Verapamil: This medication is used to treat hypertension, angina, and heart failure.
Antiplatelet Agents
Antiplatelet agents are medications that prevent platelets from clumping together and forming blood clots. They’re often used to reduce the risk of heart attack and stroke. Common antiplatelet agents used to treat unstable angina include:
- Aspirin: This medication is often used in low doses to reduce the risk of heart attack and stroke.
- Clopidogrel: This medication is used to reduce the risk of heart attack and stroke in people with acute coronary syndrome.
Lifestyle Changes for Unstable Angina
While medications are essential for managing unstable angina, lifestyle changes can also play a crucial role in reducing symptoms, improving overall health, and reducing the risk of complications. Let’s take a closer look at the lifestyle changes that can help.
Quit Smoking
Smoking is a significant risk factor for heart disease and unstable angina. Quitting smoking can help reduce the risk of heart attack, stroke, and other cardiovascular complications. 💡
Exercise Regularly
Regular exercise can help improve cardiovascular health, reduce symptoms of angina, and improve overall fitness. It’s essential to talk to your doctor before starting any new exercise program, especially if you have unstable angina. 🏋️♀️
Healthy Eating
Eating a healthy, balanced diet can help reduce the risk of heart disease and unstable angina. Focus on consuming plenty of fruits, vegetables, whole grains, and lean protein sources. Avoid foods high in salt, sugar, and unhealthy fats. 🥗
Manage Stress
Stress can exacerbate symptoms of unstable angina and increase the risk of heart attack. Engage in stress-reducing activities like yoga, meditation, or deep breathing exercises to help manage stress. 🙏
Get Enough Sleep
Getting enough sleep is essential for overall health and can help reduce symptoms of unstable angina. Aim for 7-8 hours of sleep per night and establish a consistent sleep schedule. 😴
By combining medications with lifestyle changes, individuals with unstable angina can reduce symptoms, improve overall health, and reduce the risk of complications. Remember to work closely with your healthcare provider to develop a personalized treatment plan that’s right for you. 💊

Frequently Asked Questions about Unstable Angina
What is Unstable Angina?
Unstable angina is a type of angina that occurs when the blood flow to the heart is suddenly reduced, causing severe chest pain or discomfort. It is a medical emergency that requires immediate attention.
What are the Symptoms of Unstable Angina?
The symptoms of unstable angina are similar to those of a heart attack, and may include:
- Chest pain or discomfort that is severe, sudden, and lasts longer than 20 minutes
- Pain or discomfort in the arms, back, neck, jaw, or stomach
- Shortness of breath or difficulty breathing
- Feeling of weakness, fatigue, or lightheadedness
- Nausea or vomiting
How is Unstable Angina Diagnosed?
Unstable angina is diagnosed through a combination of medical history, physical examination, and diagnostic tests, including:
- Electrocardiogram (ECG or EKG)
- Blood tests to measure troponin levels
- Imaging tests, such as echocardiogram or cardiac catheterization
What is the Difference between Unstable Angina and Stable Angina?
Unstable angina is a more severe and unpredictable form of angina, whereas stable angina is a predictable and recurring pattern of chest pain or discomfort. Unstable angina is a medical emergency, whereas stable angina can be managed with medication and lifestyle changes.
How is Unstable Angina Treated?
Treatment for unstable angina usually involves a combination of medications, lifestyle changes, and medical procedures, including:
- Medications to reduce pain, lower blood pressure, and prevent blood clots
- Angioplasty or stenting to open blocked arteries
- Coronary artery bypass grafting (CABG) surgery
- Lifestyle changes, such as quitting smoking, exercising regularly, and eating a healthy diet
What is the ICD-10 Code for Unstable Angina?
The ICD-10 code for unstable angina is I20.0.
Can Unstable Angina be Prevented?
While unstable angina cannot be completely prevented, reducing the risk factors for heart disease, such as high blood pressure, high cholesterol, and smoking, can help prevent or delay its onset. 💡




