What Is a Peptic Ulcer?
A peptic ulcer is a sore that develops on the lining of the stomach, small intestine, or esophagus. These ulcers occur when the protective mucus layer that shields these organs from stomach acid is compromised, leading to irritation and erosion. Peptic ulcers can be classified into two main types: gastric ulcers, which occur in the stomach, and duodenal ulcers, which occur in the upper part of the small intestine (duodenum).
Causes of Peptic Ulcers
Understanding the causes of peptic ulcers is crucial for effective treatment and prevention. The most common causes include:
- Helicobacter pylori (H. pylori) infection: This bacterium is a primary culprit in many peptic ulcer cases. It can damage the stomach’s protective lining, leading to ulcer formation.
- Long-term use of NSAIDs: Nonsteroidal anti-inflammatory drugs, such as ibuprofen and aspirin, can irritate the stomach lining and increase the risk of ulcers.
- Excessive alcohol consumption: Alcohol can erode the stomach lining and increase acid production, contributing to ulcer development.
- Smoking: Tobacco use can interfere with the stomach’s ability to heal and increase acid production.
- Stress: While stress alone doesn’t cause ulcers, it can exacerbate symptoms and slow healing.
Diagnosis of Peptic Ulcers
Diagnosing a peptic ulcer typically involves a combination of medical history, physical examination, and diagnostic tests. Common methods include:
- Endoscopy: A thin tube with a camera is inserted through the mouth to visualize the stomach and duodenum.
- Upper GI series: This X-ray test involves swallowing a barium solution to highlight the digestive tract.
- H. pylori tests: Blood, breath, or stool tests can determine if an H. pylori infection is present.
Peptic Ulcer Symptoms
Recognizing the symptoms of a peptic ulcer is essential for timely treatment. Symptoms can vary in intensity and may include:
Common Symptoms
- Abdominal pain: This is the most common symptom, often described as a burning or gnawing sensation in the stomach area. The pain may improve or worsen with eating.
- Nausea and vomiting: Some individuals may experience nausea, and in severe cases, vomiting may occur.
- Loss of appetite: Ulcers can lead to a decreased desire to eat due to pain or discomfort.
- Weight loss: Unintentional weight loss may occur due to reduced food intake or malabsorption.
- Indigestion: Many people with peptic ulcers report symptoms of indigestion, including bloating and gas.
Severe Symptoms to Watch For
While many symptoms can be managed with lifestyle changes and medication, some signs indicate a more serious condition that requires immediate medical attention:
- Blood in vomit or stool: This may appear as red blood or dark, tarry stools, indicating bleeding in the digestive tract.
- Severe abdominal pain: Sudden, intense pain may signal a perforated ulcer, which is a medical emergency.
- Difficulty swallowing: If you experience pain while swallowing, it may indicate complications.
If you suspect you have a peptic ulcer or are experiencing any of these symptoms, it’s essential to consult a healthcare professional for proper diagnosis and treatment. Resources like Yesil Health AI (yesilhealth.com) can provide evidence-based health answers to help you understand your condition better.
In conclusion, understanding what a peptic ulcer is and recognizing its symptoms can empower you to seek timely medical intervention. With the right treatment and lifestyle adjustments, managing peptic ulcers is entirely possible, allowing you to lead a healthier, more comfortable life. 🌟

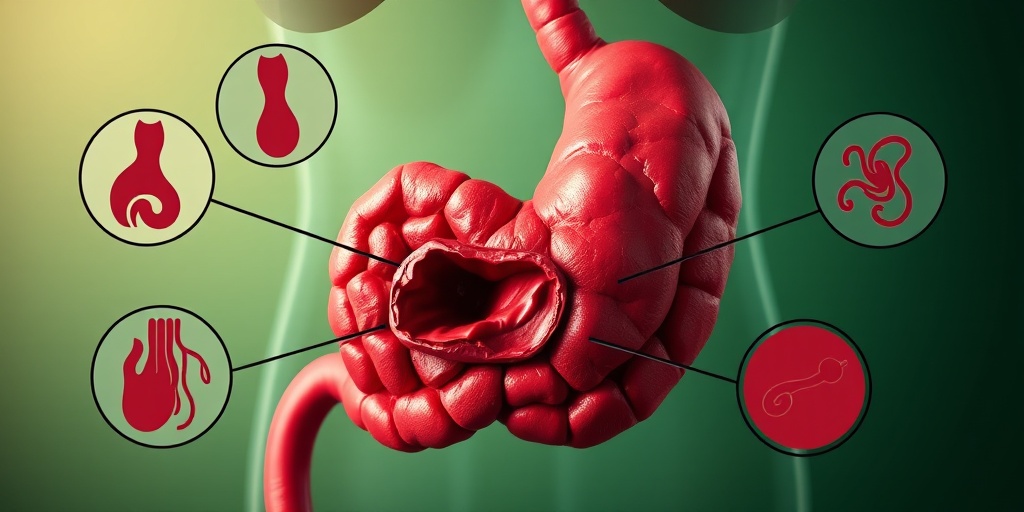
Causes of Peptic Ulcers
Peptic ulcers are open sores that develop on the lining of the stomach, small intestine, or esophagus. Understanding the causes of peptic ulcers is crucial for effective prevention and treatment. Let’s explore the primary factors that contribute to the development of these painful conditions.
1. Helicobacter pylori Infection
One of the most common causes of peptic ulcers is an infection with the bacterium Helicobacter pylori (H. pylori). This spiral-shaped bacterium can damage the protective lining of the stomach, leading to inflammation and ulcer formation. Studies have shown that a significant percentage of individuals with peptic ulcers test positive for H. pylori, making it a primary target for treatment.
2. Nonsteroidal Anti-Inflammatory Drugs (NSAIDs)
Another major contributor to peptic ulcers is the use of nonsteroidal anti-inflammatory drugs (NSAIDs), such as ibuprofen and aspirin. These medications can irritate the stomach lining and inhibit the production of protective mucus, increasing the risk of ulcer development. Long-term use or high doses of NSAIDs can significantly elevate this risk.
3. Excessive Alcohol Consumption
Excessive alcohol intake can also lead to the formation of peptic ulcers. Alcohol can irritate and erode the mucous lining of the stomach, making it more susceptible to damage from stomach acid. Additionally, alcohol can increase acid production, further exacerbating the risk of ulceration.
4. Smoking
Smoking is another lifestyle factor that can contribute to the development of peptic ulcers. It not only increases stomach acid production but also impairs the healing process of existing ulcers. Smokers are more likely to develop ulcers and experience complications compared to non-smokers.
5. Stress
While stress alone does not directly cause peptic ulcers, it can exacerbate existing conditions. Stress can lead to increased acid production and may encourage unhealthy behaviors, such as poor diet and increased alcohol consumption, which can further contribute to ulcer formation.
6. Other Medical Conditions
Certain medical conditions, such as liver disease, kidney disease, and Zollinger-Ellison syndrome, can increase the risk of developing peptic ulcers. These conditions can affect the body’s ability to produce protective mucus or regulate acid production, leading to ulcer formation.
Risk Factors for Peptic Ulcers
Understanding the risk factors for peptic ulcers can help individuals take proactive steps to reduce their chances of developing these painful sores. Here are some key risk factors to consider:
1. Age
As people age, the risk of developing peptic ulcers increases. Older adults may have a higher likelihood of H. pylori infection and may also take NSAIDs for chronic pain, further elevating their risk.
2. Family History
A family history of peptic ulcers can increase an individual’s risk. Genetic factors may play a role in how the body responds to H. pylori infection or how it produces stomach acid.
3. Chronic Use of Medications
Individuals who regularly use medications such as NSAIDs, corticosteroids, or anticoagulants are at a higher risk for developing peptic ulcers. It’s essential to discuss any long-term medication use with a healthcare provider to understand the associated risks.
4. Dietary Habits
While diet alone does not cause peptic ulcers, certain dietary habits can increase the risk. A diet high in spicy foods, caffeine, and acidic foods may irritate the stomach lining and contribute to ulcer formation.
5. Psychological Factors
Psychological factors, such as anxiety and depression, can also play a role in the development of peptic ulcers. These conditions can lead to increased stress levels and unhealthy coping mechanisms, such as smoking or excessive alcohol consumption.
6. Other Health Conditions
Individuals with certain health conditions, such as diabetes or chronic lung disease, may have an increased risk of developing peptic ulcers. These conditions can affect the body’s ability to heal and regulate stomach acid production.
By understanding the causes and risk factors of peptic ulcers, individuals can take steps to minimize their risk and seek appropriate treatment if necessary. If you suspect you have a peptic ulcer, it’s essential to consult with a healthcare professional for proper diagnosis and management. 🩺

Peptic Ulcer Diagnosis
Diagnosing a peptic ulcer is a crucial step in managing this common gastrointestinal condition. Peptic ulcers can occur in the stomach (gastric ulcers) or the upper part of the small intestine (duodenal ulcers). Understanding the symptoms and the diagnostic process can help you seek timely treatment and avoid complications.
Recognizing the Symptoms
The first step in diagnosing a peptic ulcer is recognizing its symptoms. Common signs include:
- Abdominal pain: Often described as a burning sensation, this pain typically occurs between meals or during the night.
- Nausea and vomiting: Some individuals may experience nausea, which can sometimes lead to vomiting.
- Loss of appetite: Many people with peptic ulcers find that they are less hungry due to discomfort.
- Weight loss: Unintentional weight loss can occur as a result of reduced appetite and food intake.
- Indigestion: Symptoms may include bloating, belching, and heartburn.
Medical History and Physical Examination
When you visit a healthcare provider, they will begin by taking a detailed medical history. This includes asking about:
- Your symptoms and their duration
- Any medications you are currently taking, especially nonsteroidal anti-inflammatory drugs (NSAIDs)
- Your alcohol consumption and smoking habits
- Any history of gastrointestinal issues in your family
A physical examination may also be conducted to check for tenderness in the abdomen and other signs of complications.
Diagnostic Tests
If a peptic ulcer is suspected, your doctor may recommend several diagnostic tests, including:
- Endoscopy: This procedure involves inserting a thin, flexible tube with a camera into the digestive tract to visualize the ulcer directly.
- Upper GI series: This X-ray test involves drinking a barium solution to highlight the stomach and duodenum.
- Helicobacter pylori testing: Since this bacterium is a common cause of peptic ulcers, tests may include breath, blood, or stool tests to detect its presence.
Early diagnosis is essential for effective treatment and to prevent serious complications associated with peptic ulcers. If you suspect you have an ulcer, don’t hesitate to consult a healthcare professional! 🩺
Peptic Ulcer Complications
While many peptic ulcers can be treated effectively, they can lead to serious complications if left untreated. Understanding these complications is vital for anyone diagnosed with a peptic ulcer.
Common Complications of Peptic Ulcers
Here are some of the most common complications associated with peptic ulcers:
- Bleeding: One of the most serious complications, bleeding can occur if the ulcer erodes into a blood vessel. Symptoms may include vomiting blood or passing black, tarry stools.
- Perforation: This occurs when the ulcer creates a hole in the wall of the stomach or duodenum, leading to the leakage of digestive juices into the abdominal cavity. This is a medical emergency and requires immediate attention.
- Gastric outlet obstruction: Swelling and scarring from an ulcer can block the passage of food from the stomach to the small intestine, causing severe vomiting and weight loss.
- Infection: An untreated ulcer can lead to peritonitis, an infection of the abdominal cavity, which can be life-threatening.
Recognizing Complications
It’s crucial to recognize the signs of these complications early. Symptoms that may indicate a complication include:
- Severe abdominal pain
- Sudden changes in bowel habits
- Signs of shock, such as rapid heartbeat, weakness, or fainting
If you experience any of these symptoms, seek medical attention immediately. Early intervention can significantly improve outcomes and prevent further complications. 🚑
Preventing Complications
To minimize the risk of complications, it’s essential to follow your healthcare provider’s recommendations for treatment and lifestyle changes. This may include:
- Taking prescribed medications as directed
- Avoiding NSAIDs and other irritants
- Implementing dietary changes to reduce stomach acid
- Quitting smoking and limiting alcohol consumption
By being proactive about your health, you can manage your peptic ulcer effectively and reduce the risk of complications. Remember, knowledge is power! 💪
Peptic Ulcer Treatment Options
Peptic ulcers are painful sores that develop on the lining of the stomach, small intestine, or esophagus. They can cause significant discomfort and may lead to serious complications if left untreated. Fortunately, there are several effective treatment options available for managing peptic ulcers. Let’s explore these options in detail.
1. Medications
Medications are often the first line of defense against peptic ulcers. They work by reducing stomach acid, promoting healing, and alleviating pain. Here are some common types of medications used:
- Proton Pump Inhibitors (PPIs): These drugs, such as omeprazole and lansoprazole, significantly reduce stomach acid production, allowing the ulcer to heal.
- H2-Receptor Antagonists: Medications like ranitidine and famotidine also decrease acid production but are generally less potent than PPIs.
- Antacids: Over-the-counter antacids can provide quick relief by neutralizing stomach acid, but they do not promote healing.
- Antibiotics: If the ulcer is caused by an infection with Helicobacter pylori (H. pylori), antibiotics such as amoxicillin or clarithromycin may be prescribed to eradicate the bacteria.
2. Lifestyle Changes
In addition to medications, making certain lifestyle changes can significantly aid in the treatment and prevention of peptic ulcers:
- Avoid Trigger Foods: Spicy foods, caffeine, and alcohol can exacerbate ulcer symptoms. Keeping a food diary may help identify personal triggers.
- Quit Smoking: Smoking can interfere with the stomach’s ability to heal and increase the risk of ulcer recurrence.
- Manage Stress: High-stress levels can worsen ulcer symptoms. Techniques such as meditation, yoga, or deep-breathing exercises can be beneficial.
3. Surgical Options
In rare cases where ulcers do not respond to medication or if complications arise, surgical intervention may be necessary. Surgical options include:
- Vagotomy: This procedure involves cutting the vagus nerve to reduce acid production.
- Pyloroplasty: This surgery helps to drain the stomach and reduce the risk of ulcers.
- Partial Gastrectomy: In severe cases, part of the stomach may be removed to eliminate the ulcer.
Preventing Peptic Ulcers
Preventing peptic ulcers is crucial for maintaining digestive health and avoiding the discomfort associated with these sores. Here are some effective strategies to help prevent the development of peptic ulcers:
1. Maintain a Healthy Diet
A balanced diet plays a significant role in preventing peptic ulcers. Consider the following dietary tips:
- Eat Regular Meals: Skipping meals can increase stomach acid production. Aim for regular, balanced meals throughout the day.
- Include Fiber-Rich Foods: Foods high in fiber, such as fruits, vegetables, and whole grains, can help protect the stomach lining.
- Limit Processed Foods: Highly processed foods can irritate the stomach lining. Focus on whole, natural foods instead.
2. Avoid NSAIDs
Nonsteroidal anti-inflammatory drugs (NSAIDs), such as ibuprofen and aspirin, can increase the risk of developing peptic ulcers. If you need pain relief, consult your healthcare provider for safer alternatives.
3. Manage Stress Effectively
Chronic stress can contribute to the development of peptic ulcers. Incorporating stress management techniques into your daily routine can be beneficial:
- Practice Relaxation Techniques: Activities like meditation, deep breathing, and yoga can help reduce stress levels.
- Engage in Regular Exercise: Physical activity is a great way to relieve stress and improve overall health.
4. Regular Health Check-ups
Regular visits to your healthcare provider can help monitor your digestive health and catch any potential issues early. Discuss any symptoms you may experience, such as persistent stomach pain or changes in appetite.
By following these treatment options and preventive measures, you can effectively manage and reduce the risk of peptic ulcers. Remember, if you suspect you have a peptic ulcer, it’s essential to consult with a healthcare professional for proper diagnosis and treatment. 🩺

Frequently Asked Questions about Peptic Ulcers
What is a peptic ulcer?
A peptic ulcer is a sore that develops on the lining of the stomach, small intestine, or esophagus. It occurs when the protective mucus layer is reduced, allowing stomach acid to damage the tissue.
What are the common symptoms of a peptic ulcer?
- Abdominal pain: Often described as a burning sensation.
- Nausea: Feeling sick to the stomach.
- Loss of appetite: Not feeling hungry.
- Weight loss: Unintentional weight loss can occur.
- Indigestion: Discomfort or pain in the stomach area.
How is a peptic ulcer diagnosed?
Diagnosis typically involves a combination of medical history, physical examination, and tests such as endoscopy, barium swallow, or tests for Helicobacter pylori infection.
What are the treatment options for peptic ulcers?
Treatment for peptic ulcers may include:
- Medications: Antacids, proton pump inhibitors, and antibiotics if H. pylori is present.
- Lifestyle changes: Avoiding irritants like NSAIDs, alcohol, and smoking.
- Surgery: In severe cases, surgical intervention may be necessary.
Can diet affect peptic ulcers?
Yes, certain foods can exacerbate symptoms. It’s advisable to avoid spicy foods, caffeine, and acidic foods while focusing on a balanced diet rich in fiber.
Is there a link between stress and peptic ulcers?
While stress does not directly cause peptic ulcers, it can exacerbate symptoms and hinder healing. Managing stress through relaxation techniques can be beneficial.
How can I manage peptic ulcer pain at home?
- Over-the-counter medications: Antacids can provide temporary relief.
- Warm compress: Applying a warm compress to the abdomen may help ease discomfort.
- Herbal remedies: Some people find relief with chamomile or ginger tea.
When should I see a doctor for peptic ulcer symptoms?
If you experience severe abdominal pain, vomiting blood, or black stools, it is crucial to seek medical attention immediately. These could be signs of a serious complication.
What is the ICD-10 code for peptic ulcers?
The ICD-10 code for peptic ulcer is K25 for gastric ulcers and K26 for duodenal ulcers. Specific codes may vary based on the ulcer’s characteristics.
Are there any specialists for peptic ulcer disease?
Yes, peptic ulcer disease specialists include gastroenterologists who focus on diagnosing and treating digestive system disorders, including ulcers.