“`html
What Is Rheumatoid Arthritis?
Rheumatoid arthritis (RA) is a chronic inflammatory disorder that primarily affects the joints. Unlike osteoarthritis, which is caused by wear and tear on the joints, rheumatoid arthritis is an autoimmune condition. This means that the body’s immune system mistakenly attacks its own tissues, leading to inflammation and damage in the joints. Over time, this can result in joint deformity and loss of function.
Understanding the Autoimmune Aspect
In rheumatoid arthritis, the immune system targets the synovium, the lining of the membranes that surround the joints. This inflammation can spread to other parts of the body, including the skin, eyes, lungs, heart, and blood vessels. The exact cause of RA remains unclear, but genetic, environmental, and hormonal factors are believed to play a role.
Who Is Affected?
Rheumatoid arthritis can affect anyone, but it is more common in women than men. It typically develops between the ages of 30 and 60, although it can occur at any age. Early diagnosis and treatment are crucial to managing the disease effectively and preventing long-term damage.
Rheumatoid Arthritis Symptoms
The symptoms of rheumatoid arthritis can vary widely from person to person, and they may come and go in cycles of flare-ups and remission. Here are some of the most common symptoms:
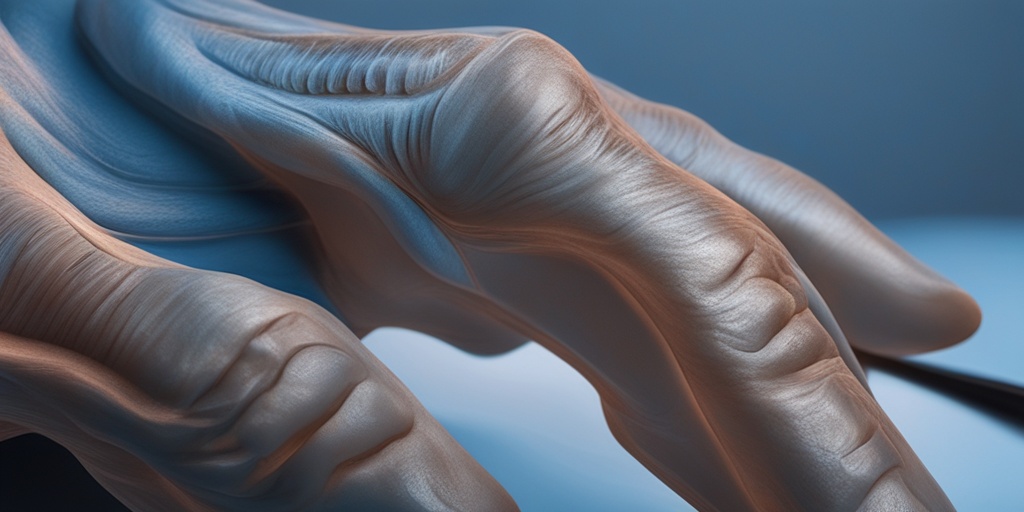
- Joint Pain and Swelling: The most characteristic symptom of RA is pain and swelling in the joints, particularly in the hands, wrists, and knees. This pain is often symmetrical, meaning it affects both sides of the body equally.
- Stiffness: Many individuals with rheumatoid arthritis experience stiffness, especially in the morning or after sitting for long periods. This stiffness can last for several hours.
- Fatigue: Chronic fatigue is a common complaint among those with RA. This can be due to the body’s ongoing battle with inflammation.
- Fever: Some people may experience a low-grade fever during flare-ups.
- Loss of Appetite: Inflammation can affect appetite, leading to weight loss in some individuals.
- Rheumatoid Nodules: These are firm lumps that can develop under the skin, often near affected joints.
Recognizing Early Signs
Early recognition of rheumatoid arthritis symptoms is vital for effective management. If you notice persistent joint pain, swelling, or stiffness, it’s essential to consult a healthcare professional for a proper evaluation. Diagnostic tests, including blood tests and imaging studies, can help confirm the diagnosis.
Impact on Daily Life
Rheumatoid arthritis can significantly impact daily activities and quality of life. The pain and stiffness can make it challenging to perform routine tasks, such as typing, cooking, or even walking. Emotional well-being can also be affected, leading to feelings of frustration or depression.
For those seeking more information on managing rheumatoid arthritis, Yesil Health AI (yesilhealth.com) offers evidence-based health answers and resources that can help you navigate your journey with this condition.
Conclusion
Understanding rheumatoid arthritis is the first step toward effective management. By recognizing the symptoms and seeking timely medical advice, individuals can take control of their health and improve their quality of life. Remember, you are not alone in this journey—support and resources are available to help you every step of the way! 🌟
“`
“`html
Rheumatoid Arthritis Causes
Rheumatoid arthritis (RA) is a chronic inflammatory disorder that primarily affects the joints, but it can also have systemic effects on the body. Understanding the causes of rheumatoid arthritis is crucial for effective management and treatment. While the exact cause remains unclear, several factors are believed to contribute to the onset of this condition.
Genetic Factors
Research indicates that genetics play a significant role in the development of rheumatoid arthritis. Individuals with a family history of RA are at a higher risk of developing the condition themselves. Specific genes, such as the HLA-DRB1 gene, have been linked to an increased susceptibility to RA. If you have relatives with rheumatoid arthritis, it’s essential to be aware of your risk.
Environmental Triggers
Environmental factors can also trigger rheumatoid arthritis in genetically predisposed individuals. Some of the most common environmental triggers include:
- Infections: Certain viral and bacterial infections may initiate the autoimmune response that leads to RA.
- Smoking: Tobacco use is a well-established risk factor for developing rheumatoid arthritis, particularly in those with a genetic predisposition.
- Pesticides: Studies have suggested a link between exposure to specific pesticides and an increased risk of RA.
Hormonal Factors
Hormones may also play a role in the development of rheumatoid arthritis. The condition is more prevalent in women than men, suggesting that hormonal differences could influence susceptibility. Fluctuations in hormone levels, particularly during pregnancy or menopause, may exacerbate symptoms or trigger the onset of RA.
Immune System Dysfunction
Rheumatoid arthritis is classified as an autoimmune disease, meaning that the body’s immune system mistakenly attacks its own tissues. This dysfunction can lead to chronic inflammation in the joints and surrounding tissues. While the precise mechanisms behind this immune response are still being studied, it is clear that a combination of genetic and environmental factors contributes to this process.
Rheumatoid Arthritis Risk Factors
Identifying the risk factors for rheumatoid arthritis can help individuals take proactive steps to reduce their chances of developing this debilitating condition. Here are some of the most significant risk factors associated with rheumatoid arthritis:
Age
Rheumatoid arthritis can occur at any age, but it is most commonly diagnosed in middle-aged individuals. The risk of developing RA increases with age, particularly for those over 40 years old.
Gender
As mentioned earlier, women are significantly more likely to develop rheumatoid arthritis than men. The ratio is approximately 3:1, indicating that hormonal and genetic factors may contribute to this disparity.
Family History
A family history of rheumatoid arthritis or other autoimmune diseases increases the likelihood of developing RA. If you have relatives with RA, it’s essential to monitor your health and consult with a healthcare professional if you experience symptoms.
Obesity
Being overweight or obese is another risk factor for rheumatoid arthritis. Excess body weight can contribute to inflammation and increase the strain on joints, potentially triggering or worsening RA symptoms.
Smoking
As previously mentioned, smoking is a significant risk factor for rheumatoid arthritis. Not only does it increase the likelihood of developing RA, but it can also exacerbate symptoms in those already diagnosed. Quitting smoking can be a crucial step in managing your health.
Occupational Exposures
Certain occupations that involve repetitive joint stress or exposure to harmful substances may increase the risk of developing rheumatoid arthritis. If you work in an environment with high exposure to chemicals or physical strain, it’s essential to take precautions to protect your joints.
In summary, while the exact causes of rheumatoid arthritis remain elusive, a combination of genetic, environmental, hormonal, and lifestyle factors contribute to its development. By understanding these causes and risk factors, individuals can take proactive steps to manage their health and seek early intervention if necessary. 🌟
“`

“`html
Rheumatoid Arthritis Diagnosis
Diagnosing Rheumatoid Arthritis (RA) can be a complex process, as it often mimics other conditions and presents with a variety of symptoms. Early diagnosis is crucial for effective management and can significantly improve the quality of life for those affected. Here’s what you need to know about the diagnosis of RA.
Understanding the Symptoms
The first step in diagnosing rheumatoid arthritis is recognizing its symptoms. Common signs include:
- Joint Pain: Persistent pain in the joints, especially in the hands, wrists, and knees.
- Swelling: Inflammation and swelling around the joints.
- Stiffness: Morning stiffness that lasts for more than 30 minutes.
- Fatigue: A general feeling of tiredness and lack of energy.
- Fever: Low-grade fever may accompany other symptoms.
These symptoms can vary in intensity and may come and go, making it essential to consult a healthcare professional if you experience them.
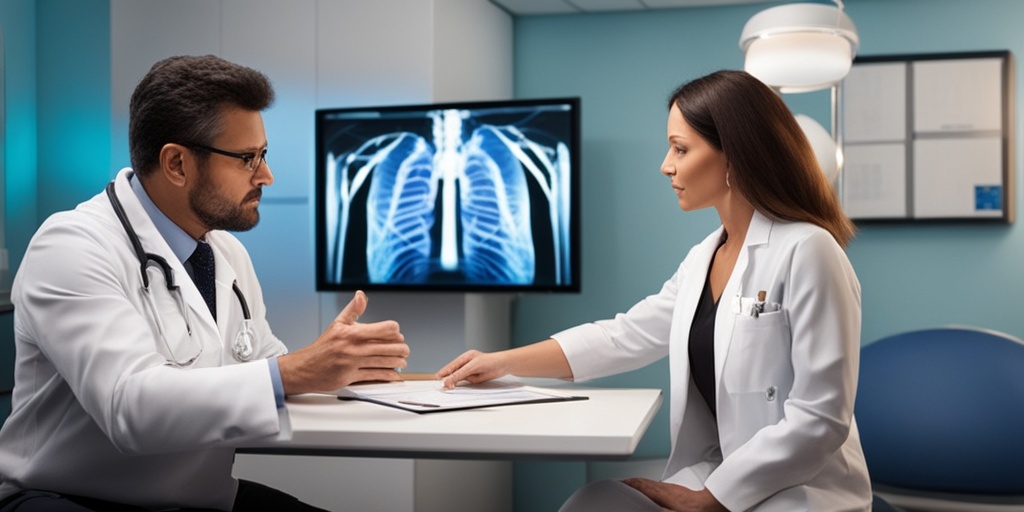
Medical History and Physical Examination
Your doctor will begin the diagnosis by taking a detailed medical history and performing a physical examination. They will ask about:
- Your symptoms and their duration.
- Any family history of autoimmune diseases.
- Previous health issues or conditions.
During the physical exam, the doctor will check for swelling, redness, and warmth in the joints, as well as assess your range of motion.
Laboratory Tests
To confirm a diagnosis of rheumatoid arthritis, your doctor may order several laboratory tests, including:
- Rheumatoid Factor (RF): This blood test checks for the presence of rheumatoid factor, an antibody often found in people with RA.
- Anti-Citrullinated Protein Antibody (ACPA): This test detects antibodies that are more specific to RA.
- Complete Blood Count (CBC): This test helps identify anemia and inflammation levels.
- Erythrocyte Sedimentation Rate (ESR): This test measures inflammation in the body.
These tests, combined with your symptoms and physical examination findings, will help your doctor determine if you have rheumatoid arthritis.
Imaging Tests
In some cases, imaging tests such as X-rays, ultrasounds, or MRIs may be used to assess joint damage and inflammation. These tests can provide valuable information about the extent of the disease and help guide treatment decisions.
Rheumatoid Arthritis Treatment Options
Once diagnosed, managing rheumatoid arthritis effectively is essential to minimize symptoms and prevent joint damage. Treatment plans are often tailored to the individual and may include a combination of medications, lifestyle changes, and alternative therapies.
Medications
Several types of medications are commonly prescribed for rheumatoid arthritis:
- Nonsteroidal Anti-Inflammatory Drugs (NSAIDs): These help reduce pain and inflammation.
- Corticosteroids: Medications like prednisone can quickly reduce inflammation and suppress the immune system.
- DMARDs (Disease-Modifying Antirheumatic Drugs): These drugs, such as methotrexate, can slow the progression of RA and prevent joint damage.
- Biologics: Targeted therapies that modify the immune response, such as TNF inhibitors, are often used for moderate to severe cases.
It’s essential to work closely with your healthcare provider to find the right medication regimen for your specific needs.
Lifestyle Changes
In addition to medications, certain lifestyle changes can help manage rheumatoid arthritis:
- Diet: A balanced diet rich in anti-inflammatory foods, such as fruits, vegetables, whole grains, and omega-3 fatty acids, can be beneficial. Some people find relief by following a rheumatoid arthritis diet.
- Exercise: Regular physical activity can help maintain joint function and reduce stiffness. Low-impact exercises like swimming and walking are often recommended.
- Stress Management: Techniques such as yoga, meditation, and deep breathing can help manage stress, which may exacerbate symptoms.
Alternative Therapies
Some individuals explore alternative therapies to complement their treatment plan. Options may include:
- Acupuncture: This traditional Chinese medicine technique may help relieve pain and improve function.
- Massage Therapy: Gentle massage can help reduce muscle tension and improve circulation.
- Supplements: Some people find relief with supplements like fish oil or turmeric, but it’s essential to consult with a healthcare provider before starting any new supplement.
Managing rheumatoid arthritis is a multifaceted approach that requires collaboration between patients and healthcare providers. By understanding the diagnosis and exploring various treatment options, individuals can take proactive steps toward living a fulfilling life despite their condition. 🌟
“`
“`html
Rheumatoid Arthritis Lifestyle Changes
Living with rheumatoid arthritis (RA) can be challenging, but making certain lifestyle changes can significantly improve your quality of life. These changes can help manage symptoms, reduce flare-ups, and enhance overall well-being. Here are some effective lifestyle adjustments to consider:
1. Adopt a Healthy Diet
Your diet plays a crucial role in managing rheumatoid arthritis symptoms. Incorporating anti-inflammatory foods can help reduce joint pain and stiffness. Consider the following dietary tips:
- Omega-3 Fatty Acids: Foods like salmon, walnuts, and flaxseeds are rich in omega-3s, which can help decrease inflammation.
- Fruits and Vegetables: Aim for a colorful plate! Berries, leafy greens, and cruciferous vegetables are packed with antioxidants.
- Whole Grains: Opt for whole grains like brown rice and quinoa instead of refined grains to maintain stable energy levels.
- Limit Processed Foods: Reduce intake of processed foods high in sugar and unhealthy fats, which can exacerbate inflammation.
2. Stay Active
Regular physical activity is essential for maintaining joint function and overall health. Here are some tips for staying active:
- Low-Impact Exercises: Activities like swimming, cycling, and walking are gentle on the joints while providing cardiovascular benefits.
- Strength Training: Incorporating light weights or resistance bands can help build muscle strength, supporting your joints.
- Flexibility and Balance: Yoga and tai chi can improve flexibility and balance, reducing the risk of falls.
3. Manage Stress
Stress can trigger flare-ups of rheumatoid arthritis symptoms. Implementing stress management techniques can be beneficial:
- Meditation and Mindfulness: Practicing mindfulness can help you stay grounded and reduce anxiety.
- Deep Breathing Exercises: Simple breathing techniques can help calm your mind and body.
- Engage in Hobbies: Spend time doing activities you love, whether it’s painting, gardening, or reading.
4. Prioritize Sleep
Quality sleep is vital for healing and managing rheumatoid arthritis. Here are some tips to improve your sleep:
- Establish a Routine: Go to bed and wake up at the same time every day to regulate your body clock.
- Create a Comfortable Sleep Environment: Ensure your bedroom is dark, quiet, and cool.
- Avoid Stimulants: Limit caffeine and electronic devices before bedtime to promote better sleep.
5. Stay Hydrated
Drinking enough water is essential for joint lubrication and overall health. Aim for at least 8 glasses of water a day, and consider herbal teas as a hydrating option. 💧
Rheumatoid Arthritis Outlook and Prognosis
The outlook for individuals diagnosed with rheumatoid arthritis can vary widely based on several factors, including the severity of the disease, the effectiveness of treatment, and lifestyle choices. Understanding the prognosis can help you manage expectations and plan for the future.
Understanding the Disease Progression
Rheumatoid arthritis is a chronic autoimmune condition that primarily affects the joints. It can lead to joint damage and disability if not managed properly. However, with early diagnosis and appropriate treatment, many individuals can lead fulfilling lives. Here are some key points regarding the prognosis:
- Early Intervention: Starting treatment early can significantly improve long-term outcomes and reduce the risk of joint damage.
- Individual Variability: Each person’s experience with RA is unique. Some may experience mild symptoms, while others may face more severe challenges.
- Response to Treatment: Many patients respond well to medications, including rheumatoid arthritis medications like DMARDs and biologics, which can help control symptoms and slow disease progression.
Long-Term Management Strategies
Managing rheumatoid arthritis is a lifelong commitment. Regular check-ups with your healthcare provider are essential to monitor disease activity and adjust treatment as needed. Here are some strategies for long-term management:
- Regular Monitoring: Routine blood tests and imaging can help assess disease activity and treatment effectiveness.
- Stay Informed: Educate yourself about RA and stay updated on new treatments and research.
- Support Systems: Engage with support groups or counseling to share experiences and coping strategies.
Quality of Life Considerations
While rheumatoid arthritis can be a challenging condition, many individuals find ways to adapt and thrive. Emphasizing a positive outlook, maintaining social connections, and focusing on personal goals can enhance your quality of life. Remember, you are not alone in this journey! 🌈
“`

“`html
Frequently Asked Questions about Rheumatoid Arthritis
What is Rheumatoid Arthritis?
Rheumatoid Arthritis is a chronic inflammatory disorder that primarily affects the joints. It occurs when the immune system mistakenly attacks the synovium, the lining of the membranes that surround the joints, leading to inflammation, pain, and potential joint damage.
What are the common symptoms of Rheumatoid Arthritis?
- Joint pain and swelling
- Stiffness, especially in the morning
- Fatigue and weakness
- Fever
- Weight loss
How is Rheumatoid Arthritis diagnosed?
Diagnosis typically involves a combination of physical examinations, blood tests (including rheumatoid factor and anti-CCP antibodies), and imaging tests like X-rays or MRIs to assess joint damage.
What treatments are available for Rheumatoid Arthritis?
Treatment options for Rheumatoid Arthritis include:
- Nonsteroidal anti-inflammatory drugs (NSAIDs)
- Disease-modifying antirheumatic drugs (DMARDs)
- Biologic agents
- Corticosteroids
- Physical therapy
Can diet affect Rheumatoid Arthritis symptoms?
Yes, certain dietary choices may help manage symptoms. A diet rich in omega-3 fatty acids, antioxidants, and whole foods can be beneficial. It’s advisable to avoid processed foods and excessive sugar.
What is the difference between Rheumatoid Arthritis and Osteoarthritis?
Rheumatoid Arthritis is an autoimmune condition that affects the lining of the joints, while osteoarthritis is a degenerative joint disease caused by wear and tear on the joints. Symptoms and treatment approaches differ significantly between the two.
Are there any specific medications for Rheumatoid Arthritis?
Yes, there are several medications specifically designed for Rheumatoid Arthritis, including:
- Methotrexate
- Hydroxychloroquine
- Biologics like adalimumab and etanercept
Can Rheumatoid Arthritis lead to other health issues?
Yes, individuals with Rheumatoid Arthritis may be at higher risk for other health problems, including cardiovascular disease, lung disease, and osteoporosis due to chronic inflammation and medication side effects.
Is there a blood test for Rheumatoid Arthritis?
Yes, blood tests can help diagnose Rheumatoid Arthritis. Common tests include the rheumatoid factor test and anti-CCP antibody test, which can indicate the presence of the disease.
How can I manage my Rheumatoid Arthritis symptoms at home?
Managing symptoms at home can include:
- Regular exercise to maintain joint function
- Applying heat or cold to affected joints
- Practicing stress-reduction techniques like yoga or meditation
- Maintaining a healthy weight
Can I still lead an active life with Rheumatoid Arthritis?
Absolutely! Many individuals with Rheumatoid Arthritis lead fulfilling and active lives. With proper treatment and lifestyle adjustments, you can manage symptoms effectively.
Where can I find support for living with Rheumatoid Arthritis?
Support groups, both online and in-person, can provide valuable resources and community. Organizations like the Arthritis Foundation offer information and support for those living with Rheumatoid Arthritis.
“`