What Is Pudendal Neuralgia?
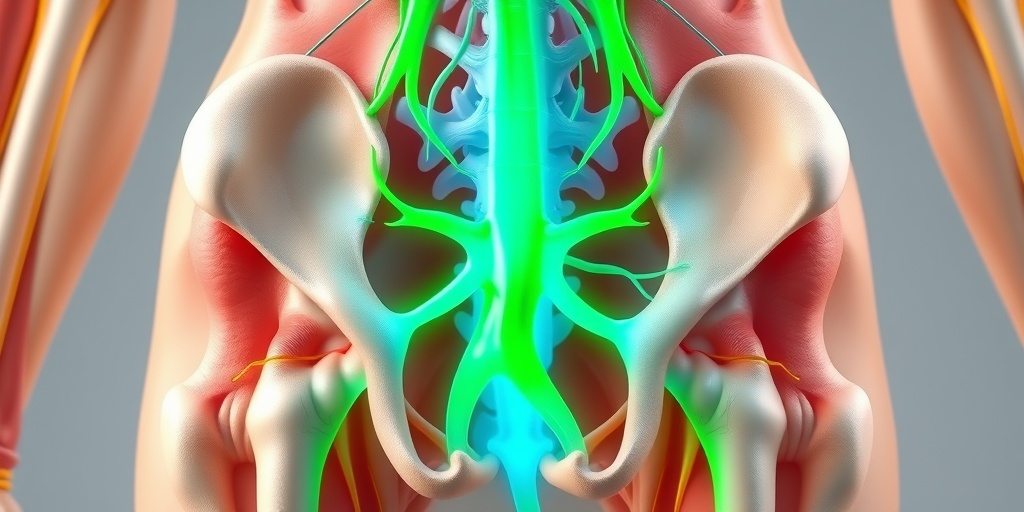
Pudendal neuralgia is a condition characterized by chronic pain in the pelvic region, specifically affecting the pudendal nerve, which is responsible for sensation in the genital area and the function of the pelvic floor. This nerve can become entrapped or irritated due to various factors, leading to discomfort and a range of symptoms that can significantly impact a person’s quality of life.
The pudendal nerve originates from the sacral plexus and travels through the pelvis, innervating the external genitalia, perineum, and anal region. When this nerve is compromised, it can result in a condition that is often misunderstood and misdiagnosed, making awareness and education crucial for those affected.
Causes of Pudendal Neuralgia
Understanding the causes of pudendal neuralgia is essential for effective treatment. Some common factors include:
- Trauma or Injury: Direct trauma to the pelvic area, such as from childbirth or surgery, can lead to nerve damage.
- Prolonged Sitting: Activities that involve long periods of sitting, like cycling or sitting at a desk, can compress the pudendal nerve.
- Pelvic Floor Dysfunction: Issues with the pelvic floor muscles can contribute to nerve entrapment.
- Infections: Certain infections in the pelvic region can irritate the nerve.
- Chronic Conditions: Conditions like diabetes or multiple sclerosis may also play a role in nerve health.
Pudendal Neuralgia Symptoms
The symptoms of pudendal neuralgia can vary widely among individuals, but they often include:
- Chronic Pain: This is the hallmark symptom, often described as sharp, burning, or aching pain in the pelvic area.
- Discomfort During Sitting: Many individuals find that sitting exacerbates their pain, leading to a need for special cushions designed for pudendal neuralgia.
- Sexual Dysfunction: Pain during intercourse or a decrease in sexual desire can occur due to nerve irritation.
- Urinary Issues: Some may experience urgency, frequency, or pain during urination.
- Anal Pain: Discomfort in the anal region can also be a symptom, affecting bowel movements.
Recognizing Symptoms Early
Early recognition of symptoms is vital for effective management. If you experience persistent pelvic pain, especially if it worsens with sitting or during sexual activity, it’s important to consult a healthcare professional. They can help determine if pudendal neuralgia is the underlying cause and guide you toward appropriate treatment options.
Seeking Help
Finding a pudendal neuralgia specialist can be a game-changer. These professionals are equipped to provide tailored treatment plans that may include physical therapy, medications, or even nerve blocks. Resources like Yesil Health AI can also offer evidence-based answers to your health questions, helping you navigate your treatment journey.
In conclusion, pudendal neuralgia is a complex condition that requires a comprehensive approach to diagnosis and treatment. By understanding the symptoms and seeking help early, individuals can find relief and improve their quality of life. If you suspect you may be suffering from this condition, don’t hesitate to reach out to a healthcare provider for guidance. 🌟
Pudendal Neuralgia Causes
Pudendal neuralgia is a condition characterized by chronic pain in the pelvic region, often affecting the genital area, perineum, and buttocks. Understanding the causes of pudendal neuralgia is crucial for effective treatment and management. Here are some of the primary causes:
1. Nerve Compression
One of the most common causes of pudendal neuralgia is compression of the pudendal nerve. This can occur due to:
- Prolonged Sitting: Sitting for extended periods, especially on hard surfaces, can put pressure on the pudendal nerve.
- Injury: Trauma to the pelvic area, such as from accidents or surgical procedures, can lead to nerve damage or compression.
- Childbirth: The process of childbirth can stretch or compress the pudendal nerve, leading to pain.
2. Pelvic Floor Dysfunction
Pelvic floor dysfunction can also contribute to pudendal neuralgia. This condition occurs when the muscles of the pelvic floor do not function properly, leading to:
- Muscle Tension: Tight or spasming pelvic floor muscles can irritate the pudendal nerve.
- Weakness: Weak pelvic muscles may not provide adequate support, leading to nerve compression.
3. Infections and Inflammation
Infections in the pelvic region, such as sexually transmitted infections (STIs) or urinary tract infections (UTIs), can cause inflammation that affects the pudendal nerve. Conditions like prostatitis in men can also lead to similar symptoms.
4. Structural Abnormalities
Some individuals may have anatomical variations or abnormalities that predispose them to pudendal neuralgia. These can include:
- Pelvic Tumors: Growths in the pelvic area can exert pressure on the pudendal nerve.
- Bone Spurs: Bony growths in the pelvis can also lead to nerve compression.
5. Other Medical Conditions
Several medical conditions can contribute to the development of pudendal neuralgia, including:
- Diabetes: This condition can lead to nerve damage over time, increasing the risk of pudendal neuralgia.
- Multiple Sclerosis: MS can affect nerve function and lead to various types of neuropathic pain.
Pudendal Neuralgia Risk Factors
Identifying the risk factors associated with pudendal neuralgia can help individuals understand their likelihood of developing this condition. Here are some key risk factors to consider:
1. Gender
Pudendal neuralgia is more commonly reported in women than in men. This may be due to factors such as childbirth and hormonal changes that can affect nerve health.
2. Age
While pudendal neuralgia can occur at any age, it is more frequently diagnosed in middle-aged individuals. As people age, the risk of nerve compression and other related conditions may increase.
3. Lifestyle Factors
Certain lifestyle choices can elevate the risk of developing pudendal neuralgia:
- Prolonged Sitting: Occupations or activities that require long periods of sitting can increase the risk.
- High-Impact Sports: Activities that involve repetitive pelvic movements, such as cycling or running, may contribute to nerve irritation.
4. Previous Pelvic Surgery
Individuals who have undergone pelvic surgery may be at a higher risk for pudendal neuralgia due to potential nerve damage or scarring that can occur during the procedure.
5. Chronic Conditions
Chronic conditions such as diabetes, inflammatory bowel disease, or pelvic inflammatory disease can increase the likelihood of developing pudendal neuralgia due to their effects on nerve health and pelvic anatomy.
Understanding the causes and risk factors of pudendal neuralgia is essential for early diagnosis and effective treatment. If you suspect you may be experiencing symptoms of this condition, consulting with a healthcare professional is crucial for proper evaluation and management. 🩺

Pudendal Neuralgia Diagnosis
Pudendal neuralgia is a condition that can cause significant discomfort and distress, often leading to a challenging journey toward diagnosis. Understanding the diagnostic process is crucial for those experiencing symptoms. Here’s what you need to know about diagnosing pudendal neuralgia.
Recognizing the Symptoms
The first step in diagnosing pudendal neuralgia is recognizing its symptoms. Common signs include:
- Pelvic pain: This can be sharp, burning, or aching and may worsen with sitting.
- Genital discomfort: Patients often report pain in the genital area, which can be debilitating.
- Urinary issues: Some individuals experience urinary urgency or incontinence.
- Sexual dysfunction: Pain during intercourse is a frequent complaint.
If you’re experiencing any of these symptoms, it’s essential to consult a healthcare professional who can guide you through the diagnostic process.
Consulting a Specialist
Finding the right pudendal neuralgia specialist is vital. Typically, a neurologist, pain management specialist, or a pelvic floor physical therapist can provide the necessary expertise. During your consultation, be prepared to discuss:
- Your medical history
- The onset and nature of your symptoms
- Any previous treatments or medications
These details will help your doctor understand your condition better and tailor the diagnostic approach accordingly.
Diagnostic Tests
While there is no single test for pudendal neuralgia, several diagnostic methods can help confirm the condition:
- Physical examination: A thorough examination of the pelvic area can reveal tenderness or pain.
- Imaging tests: MRI or CT scans may be used to rule out other conditions affecting the pelvic region.
- Nerve blocks: A pudendal nerve block can provide temporary relief and confirm the diagnosis if symptoms improve.
These tests, combined with your symptoms and medical history, will help your healthcare provider make an accurate diagnosis.
Pudendal Neuralgia Treatment Options
Once diagnosed, the next step is exploring treatment options for pudendal neuralgia. The goal is to alleviate pain and improve quality of life. Here are some effective treatment strategies:
Medications
Medications are often the first line of defense against pudendal neuralgia. Commonly prescribed options include:
- Antidepressants: Certain antidepressants can help manage nerve pain.
- Anticonvulsants: Medications like gabapentin or pregabalin may reduce nerve-related pain.
- Topical treatments: Creams or patches containing lidocaine can provide localized relief.
Always consult with your healthcare provider to determine the best medication regimen for your specific needs.
Physical Therapy
Pudendal neuralgia physical therapy is a highly effective treatment option. A specialized physical therapist can guide you through exercises designed to:
- Strengthen pelvic floor muscles
- Improve flexibility
- Reduce tension in the pelvic area
Incorporating pudendal neuralgia exercises into your routine can significantly enhance your recovery process. Many therapists provide pudendal neuralgia exercises PDFs to help you practice at home.
Alternative Therapies
In addition to conventional treatments, many patients find relief through alternative therapies. These may include:
- Acupuncture: This ancient practice can help alleviate pain and promote healing.
- Chiropractic care: Adjustments may relieve pressure on the pudendal nerve.
- Massage therapy: Targeted massage can help reduce muscle tension in the pelvic area.
Always discuss these options with your healthcare provider to ensure they complement your overall treatment plan.
Surgical Options
In severe cases where conservative treatments fail, surgical intervention may be considered. Procedures can include:
- Pudendal nerve decompression: This surgery aims to relieve pressure on the pudendal nerve.
- Neurectomy: In some cases, removing a portion of the nerve may be necessary.
Surgery is typically a last resort and should be discussed thoroughly with a specialist.
In conclusion, diagnosing and treating pudendal neuralgia involves a comprehensive approach tailored to each individual. By understanding your options and working closely with healthcare professionals, you can find relief and improve your quality of life. 🌟

Pudendal Neuralgia Home Remedies
Pudendal neuralgia is a condition that can cause significant discomfort and pain in the pelvic region. While medical treatments are essential, many individuals seek home remedies to alleviate symptoms and improve their quality of life. Here are some effective strategies you can try at home:
1. Warm Compresses
Applying a warm compress to the affected area can help relax the muscles and reduce pain. The heat increases blood flow, which may aid in healing. Simply soak a cloth in warm water, wring it out, and place it on the pelvic area for 15-20 minutes. 🌡️
2. Gentle Stretching and Exercises
Engaging in gentle stretching and specific exercises can help relieve tension in the pelvic muscles. Consider incorporating the following:
- Kegel exercises: Strengthen pelvic floor muscles.
- Hip stretches: Improve flexibility and reduce tightness.
- Yoga: Focus on poses that promote relaxation and stretching.
For a detailed guide, you can find pudendal neuralgia exercises PDF resources online. 🧘♀️
3. Dietary Adjustments
What you eat can significantly impact your overall health and pain levels. Consider incorporating anti-inflammatory foods into your diet, such as:
- Fruits and vegetables (especially berries and leafy greens)
- Fatty fish (rich in omega-3 fatty acids)
- Nuts and seeds
Additionally, staying hydrated is crucial. Aim for at least 8 glasses of water a day to help flush out toxins and reduce inflammation. 💧
4. Mindfulness and Relaxation Techniques
Stress can exacerbate pain, so incorporating mindfulness practices can be beneficial. Techniques such as meditation, deep breathing exercises, and progressive muscle relaxation can help manage stress levels and reduce the perception of pain. 🧘♂️
5. Supportive Cushions
Using a pudendal neuralgia cushion can provide relief when sitting. These specially designed cushions help distribute weight evenly and reduce pressure on the pelvic area. Look for cushions that offer ergonomic support and comfort. 🛋️
Pudendal Neuralgia Outlook and Management
The outlook for individuals with pudendal neuralgia can vary widely based on the underlying cause and the effectiveness of treatment strategies. Understanding the condition and exploring management options is crucial for improving your quality of life.
Understanding the Condition
Pudendal neuralgia occurs when the pudendal nerve, which supplies sensation to the pelvic region, becomes entrapped or irritated. This can lead to chronic pain, discomfort during sitting, and other symptoms. Identifying the root cause is essential for effective management.
Medical Treatments
While home remedies can provide relief, medical treatments may be necessary for more severe cases. Common options include:
- Physical therapy: A specialized physical therapist can help with targeted exercises and techniques to relieve nerve compression.
- Medications: Pain relievers, anti-inflammatory drugs, or nerve pain medications may be prescribed.
- Injections: Corticosteroid injections can reduce inflammation and provide temporary relief.
Finding a Specialist
If you’re struggling with pudendal neuralgia, it may be beneficial to consult a pudendal neuralgia specialist. These healthcare professionals have experience in diagnosing and treating this condition, ensuring you receive the most effective care. You can search for specialists near you or ask your primary care physician for recommendations. 🩺
Long-Term Management Strategies
Managing pudendal neuralgia often requires a multifaceted approach. Here are some long-term strategies to consider:
- Regular exercise: Maintaining a consistent exercise routine can help strengthen pelvic muscles and improve overall health.
- Stress management: Incorporating relaxation techniques into your daily routine can help reduce pain flare-ups.
- Support groups: Connecting with others who have similar experiences can provide emotional support and practical advice.
By combining home remedies with medical treatments and lifestyle adjustments, individuals with pudendal neuralgia can work towards a more manageable and fulfilling life. Remember, it’s essential to consult with healthcare professionals to tailor a plan that suits your specific needs. 🌈

Frequently Asked Questions about Pudendal Neuralgia
What is Pudendal Neuralgia?
Pudendal Neuralgia is a condition characterized by chronic pain in the pelvic region, often caused by irritation or damage to the pudendal nerve. This nerve is responsible for sensation in the genital area and plays a crucial role in bladder and bowel control.
What are the common symptoms of Pudendal Neuralgia?
- Chronic pelvic pain
- Discomfort during sitting
- Pain during sexual activity
- Urinary urgency or incontinence
- Difficulty with bowel movements
How is Pudendal Neuralgia diagnosed?
Diagnosis typically involves a thorough medical history, physical examination, and sometimes imaging studies or nerve conduction tests to rule out other conditions. A specialist may also perform a nerve block to confirm the diagnosis.
What are the treatment options for Pudendal Neuralgia?
Treatment may include:
- Physical therapy: Specialized exercises can help relieve pressure on the nerve.
- Medications: Pain relievers, anti-inflammatory drugs, or nerve pain medications may be prescribed.
- Injections: Corticosteroid or nerve block injections can provide temporary relief.
- Surgery: In severe cases, surgical intervention may be necessary to relieve nerve compression.
Are there specific exercises for Pudendal Neuralgia?
Yes, certain exercises can help alleviate symptoms. These may include pelvic floor exercises, stretching, and strengthening routines. It’s essential to consult with a healthcare provider or physical therapist for a tailored exercise plan.
Is there a specific cushion recommended for Pudendal Neuralgia?
Many individuals find relief using a pudendal neuralgia cushion, which is designed to reduce pressure on the pelvic area while sitting. Look for cushions with a cut-out design to provide comfort.
Can men experience Pudendal Neuralgia?
Yes, pudendal neuralgia can affect men as well as women. The symptoms may manifest differently, but the underlying nerve irritation remains the same.
Where can I find a specialist for Pudendal Neuralgia?
To find a pudendal neuralgia specialist near you, consider consulting with a pain management clinic, a neurologist, or a pelvic health physical therapist. Online directories and patient forums can also provide recommendations.
What is the ICD-10 code for Pudendal Neuralgia?
The ICD-10 code for pudendal neuralgia is G57.4. This code is used for billing and insurance purposes when diagnosing this condition.
Where can I find more information or support?
Online communities, such as forums on Reddit, can be valuable resources for sharing experiences and advice. Additionally, reputable health websites and support groups can provide further information on managing pudendal neuralgia.




