What Is MPS Disorder II?
Mucopolysaccharidosis type II (MPS II), also known as Hunter syndrome, is a rare genetic disorder that affects the body’s ability to break down and recycle mucopolysaccharides, a type of sugar molecule. This leads to the accumulation of these molecules in cells, tissues, and organs, causing a range of physical and mental health problems.
Causes and Inheritance
MPS II is caused by a deficiency of the enzyme iduronate-2-sulfatase, which is necessary for the breakdown of mucopolysaccharides. This deficiency is inherited in an X-linked recessive pattern, meaning that the gene responsible for the disorder is located on the X chromosome and is more common in males. Females can be carriers of the gene, but they are usually not affected by the disorder.
Prevalence
MPS II is a rare disorder, affecting approximately 1 in 100,000 to 1 in 150,000 births. It is more common in males, with a male-to-female ratio of 3:1.
MPS Disorder II Symptoms
The symptoms of MPS II can vary in severity and may appear at different ages. Some children may show signs of the disorder in early childhood, while others may not exhibit symptoms until later in life.
Physical Symptoms
Physical symptoms of MPS II may include:
- Coarse facial features, such as a prominent forehead, nose, and jaw
- Short stature, with an average height of around 4 feet 11 inches
- Joint stiffness and limited mobility, making it difficult to move and perform daily activities
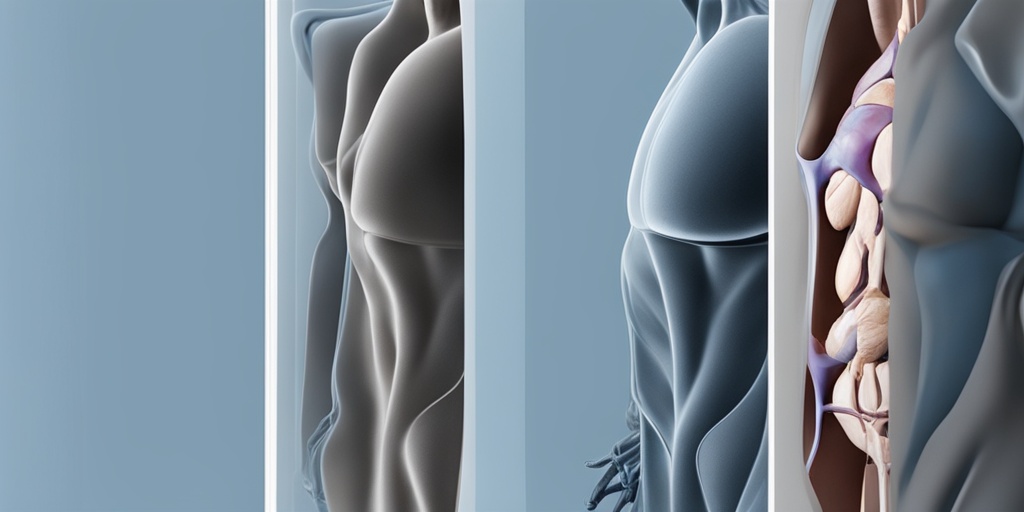
- Enlarged liver and spleen, which can lead to abdominal pain and discomfort
- Respiratory problems, such as sleep apnea and difficulty breathing
- Hearing loss, which can be progressive and severe
Intellectual and Developmental Delays
In addition to physical symptoms, MPS II can also cause intellectual and developmental delays, including:
- Delayed speech and language skills, making it difficult to communicate effectively
- Learning disabilities, which can impact academic performance and daily functioning
- Behavioral problems, such as hyperactivity, anxiety, and aggression
If you or a loved one is experiencing symptoms of MPS II, it’s essential to consult with a healthcare professional for proper diagnosis and treatment. With the right care and support, individuals with MPS II can lead fulfilling lives and manage their symptoms effectively.
For more information on MPS II and other health topics, visit Yesil Health AI, a valuable resource for evidence-based health answers. 🏥
Causes and Inheritance of MPS Disorder II
Mucopolysaccharidosis type II (MPS II), also known as Hunter syndrome, is a rare genetic disorder caused by a deficiency of the enzyme iduronate 2-sulfatase. This enzyme is essential for breaking down complex sugars called glycosaminoglycans (GAGs) in the body. Without sufficient iduronate 2-sulfatase, GAGs accumulate in cells, leading to a range of symptoms and complications.
Inheritance Pattern
MPS II is an X-linked recessive disorder, which means that the mutated gene responsible for the condition is located on the X chromosome. Females have two X chromosomes, while males have one X and one Y chromosome. This difference in chromosome makeup affects how the disorder is inherited:
- Females: Females can be carriers of the mutated gene, meaning they have one normal and one mutated X chromosome. They may not exhibit symptoms themselves but can pass the mutated gene to their sons, who have a 50% chance of developing MPS II.
- Males: Males with MPS II have a mutated X chromosome and will develop the condition. They cannot pass the mutated gene to their sons, but all their daughters will be carriers.
Genetic Mutations
The iduronate 2-sulfatase gene is responsible for encoding the enzyme that breaks down GAGs. Mutations in this gene lead to a deficiency or complete absence of the enzyme, causing MPS II. These mutations can occur spontaneously or be inherited from a parent. There are over 500 known mutations associated with MPS II, making each case unique.
Research suggests that the severity of MPS II symptoms may be influenced by the type and location of the mutation. However, more studies are needed to fully understand the relationship between genetic mutations and the progression of the disorder.
MPS Disorder II Diagnosis and Testing
Diagnosing MPS II can be a complex process, as the symptoms can be similar to those of other conditions. A comprehensive diagnostic approach involves a combination of clinical evaluations, laboratory tests, and genetic analysis.
Clinical Evaluation
A healthcare professional will typically start by conducting a physical examination and reviewing the patient’s medical history. They may look for signs of MPS II, such as:
- Coarse facial features
- Short stature
- Hepatosplenomegaly (enlarged liver and spleen)
- Joint stiffness and limited mobility
- Respiratory problems
Laboratory Tests
Several laboratory tests can help confirm the diagnosis of MPS II:
- Enzyme assay: Measures the activity of iduronate 2-sulfatase in white blood cells or fibroblasts.
- Urine GAG analysis: Detects elevated levels of GAGs in urine, which is a hallmark of MPS II.
- Molecular genetic testing: Analyzes the iduronate 2-sulfatase gene to identify mutations.
These tests can help identify MPS II, but a definitive diagnosis often requires a combination of clinical evaluation, laboratory tests, and genetic analysis.
Early diagnosis and treatment are crucial in managing MPS II. If you suspect that you or a family member may have MPS II, consult a healthcare professional for guidance and support. 💊

MPS Disorder II Treatment Options
When it comes to treating MPS Disorder II, also known as Hunter syndrome, the primary goal is to manage the symptoms and slow down the progression of the disease. While there is no cure for MPS II, various treatment options are available to improve the quality of life for individuals affected by this rare genetic disorder.
Enzyme Replacement Therapy (ERT)
ERT is the most effective treatment for MPS II, and it involves replacing the deficient enzyme iduronate-2-sulfatase with a synthetic version. This helps to break down the accumulated glycosaminoglycans (GAGs) in the body, reducing the risk of complications and improving overall health. ERT is typically administered through weekly infusions, and it’s essential to start treatment as early as possible to achieve the best outcomes.
Symptomatic Treatment
In addition to ERT, various symptomatic treatments can help alleviate specific symptoms associated with MPS II. These may include:
- Pain management: Medications to reduce pain and discomfort, such as analgesics and anti-inflammatory drugs.
- Respiratory support: Oxygen therapy, ventilator support, or other respiratory aids to help manage breathing difficulties.
- Gastrointestinal management: Medications to treat gastrointestinal issues, such as constipation, diarrhea, or abdominal pain.
- Orthopedic interventions: Surgery or other orthopedic procedures to correct skeletal abnormalities, such as joint deformities or spinal cord compression.
- Speech and language therapy: To improve communication skills and address speech difficulties.
- Occupational therapy: To enhance daily functioning and independence.
Bone Marrow Transplantation
In some cases, bone marrow transplantation may be considered as a treatment option for MPS II. This involves replacing the affected bone marrow with healthy stem cells, which can help to produce the deficient enzyme. However, this procedure carries significant risks and is typically reserved for severe cases of MPS II.
Managing MPS Disorder II Symptoms
While treatment options can help alleviate symptoms, it’s essential to manage MPS II symptoms effectively to improve the quality of life for individuals affected by this condition. Here are some tips to help manage MPS II symptoms:
Stay Active
Regular exercise can help maintain flexibility, strength, and mobility. It’s essential to work with a healthcare professional to develop a personalized exercise plan that suits individual needs and abilities.
Manage Pain
Pain management is crucial in MPS II. This may involve a combination of medications, physical therapy, and alternative therapies, such as acupuncture or massage.
Monitor Respiratory Health
Respiratory health is a critical aspect of MPS II management. Regular monitoring of lung function, oxygen saturation, and other respiratory parameters can help identify potential issues early on.
Stay Hydrated
Adequate hydration is essential to help flush out toxins and maintain overall health. Encourage individuals with MPS II to drink plenty of water throughout the day.
By understanding the available treatment options and learning to manage MPS II symptoms effectively, individuals affected by this condition can improve their quality of life and reduce the risk of complications. 💊

MPS Disorder II Prognosis and Life Expectancy
Receiving a diagnosis of MPS Disorder II, also known as Hunter syndrome, can be overwhelming and raise many questions about the future. One of the most pressing concerns is the prognosis and life expectancy of individuals with this rare genetic disorder. In this article, we’ll delve into the current understanding of MPS Disorder II prognosis and life expectancy, as well as the factors that influence them.
What is the Life Expectancy of MPS Disorder II?
The life expectancy of individuals with MPS Disorder II varies depending on the severity of the condition and the presence of any complications. Historically, children with MPS Disorder II rarely lived beyond their teenage years. However, with advances in medical technology and treatment options, life expectancy has increased significantly.
According to the National MPS Society, the average life expectancy for individuals with MPS Disorder II is around 20-30 years. However, some individuals have been known to live into their 40s and 50s with proper medical care and management.
Factors Affecting Prognosis and Life Expectancy
Several factors can influence the prognosis and life expectancy of individuals with MPS Disorder II, including:
- Severity of symptoms: The severity of symptoms, such as cognitive impairment, physical disabilities, and organ damage, can impact life expectancy.
- Age of diagnosis: Early diagnosis and treatment can significantly improve life expectancy.
- Treatment options: Access to enzyme replacement therapy (ERT) and other treatments can slow disease progression and improve quality of life.
- Complications: The presence of complications, such as respiratory problems, cardiovascular disease, and neurological damage, can reduce life expectancy.
Managing MPS Disorder II: Improving Prognosis and Life Expectancy
While there is no cure for MPS Disorder II, managing the condition through a comprehensive treatment plan can improve prognosis and life expectancy. This includes:
- Enzyme replacement therapy (ERT): Replacing the deficient enzyme to slow disease progression.
- Symptomatic management: Managing symptoms, such as pain, sleep disturbances, and gastrointestinal issues, to improve quality of life.
- Regular medical care: Regular check-ups with healthcare professionals to monitor disease progression and address any complications.
- Supportive care: Providing emotional, social, and financial support to individuals with MPS Disorder II and their families.
By understanding the prognosis and life expectancy of MPS Disorder II, individuals and families can better prepare for the future and make informed decisions about their care. In the next section, we’ll explore the importance of coping and support for individuals living with MPS Disorder II.
Living with MPS Disorder II: Coping and Support
Living with MPS Disorder II can be challenging, not only for the individual but also for their families and caregivers. Coping with the physical, emotional, and social impacts of the condition requires a comprehensive support system. In this section, we’ll discuss the importance of coping and support for individuals living with MPS Disorder II.
The Importance of Emotional Support
Emotional support is crucial for individuals with MPS Disorder II, as they often face unique challenges, such as social isolation, anxiety, and depression. Having a strong support network can help individuals cope with these emotional challenges and improve their overall well-being.
Families, caregivers, and healthcare professionals can provide emotional support by:
- Listening and validating feelings: Acknowledging the individual’s emotions and concerns can help them feel heard and understood.
- Offering emotional validation: Recognizing the individual’s strengths and accomplishments can help build confidence and self-esteem.
- Encouraging social connections: Facilitating social interactions and connections can help reduce feelings of isolation and loneliness.
Building a Support Network
Building a support network is essential for individuals with MPS Disorder II. This network can include:
- Families and caregivers: Providing emotional, physical, and financial support.
- Healthcare professionals: Offering medical guidance, treatment options, and emotional support.
- Support groups: Connecting with others who share similar experiences and challenges.
- Online resources: Accessing educational materials, online forums, and advocacy organizations.
By building a strong support network, individuals with MPS Disorder II can better cope with the challenges of their condition and improve their overall quality of life. Remember, you are not alone in this journey! 🌟

Frequently Asked Questions about MPS Disorder II
What is MPS Disorder II?
MPS Disorder II, also known as Hunter syndrome, is a rare genetic disorder caused by a deficiency of the enzyme iduronate-2-sulfatase. This enzyme is necessary for the breakdown of certain complex sugars in the body.
What are the symptoms of MPS Disorder II?
The symptoms of MPS Disorder II can vary in severity and may include:
- Coarse facial features
- Short stature
- Joint stiffness and limited mobility
- Enlarged liver and spleen
- Respiratory problems
- Developmental delays and intellectual disability
How is MPS Disorder II diagnosed?
MPS Disorder II is typically diagnosed through a combination of clinical evaluation, laboratory tests, and genetic analysis. These may include:
- Physical examination
- Urine tests to detect excess sugars
- Enzyme assays to measure iduronate-2-sulfatase activity
- Genetic testing to identify mutations in the IDS gene
Is there a treatment for MPS Disorder II?
Currently, there is no cure for MPS Disorder II, but various treatments can help manage the symptoms and slow disease progression. These may include:
- Enzyme replacement therapy (ERT) to replace the deficient enzyme
- Symptomatic treatment for respiratory, gastrointestinal, and other related issues
- Physical therapy and occupational therapy to improve mobility and daily functioning
How can I cope with MPS Disorder II?
Coping with MPS Disorder II requires a comprehensive approach that involves medical management, emotional support, and lifestyle adjustments. Some tips include:
- Seeking support from family, friends, and support groups
- Staying informed about the latest research and treatment options
- Practicing self-care and stress management techniques
- Adapting to physical limitations and finding alternative ways to engage in activities
Is MPS Disorder II inherited?
MPS Disorder II is an X-linked recessive disorder, which means that the mutated gene is located on the X chromosome. This means that:
- Females can be carriers of the mutated gene and may pass it on to their sons
- Sons of carriers have a 50% chance of inheriting the mutated gene and developing MPS Disorder II
- Daughters of carriers have a 50% chance of becoming carriers themselves
What is the prognosis for MPS Disorder II?
The prognosis for MPS Disorder II varies depending on the severity of the symptoms and the effectiveness of treatment. With proper management, many individuals with MPS Disorder II can lead active and fulfilling lives, although they may require ongoing medical care and support.
Where can I find more information about MPS Disorder II?
There are several resources available for individuals and families affected by MPS Disorder II, including:
- The National MPS Society
- The MPS II Research Foundation
- Genetic counseling services
- Online support groups and forums
Remember, it’s essential to consult with a healthcare professional for personalized information and guidance on managing MPS Disorder II. 💊




