What Is Chronic Kidney Disease?
Chronic Kidney Disease (CKD) is a long-term condition characterized by a gradual loss of kidney function over time. The kidneys play a crucial role in filtering waste products and excess fluids from the blood, which are then excreted as urine. When the kidneys are damaged, they cannot perform these functions effectively, leading to a buildup of waste in the body.
CKD is often a silent condition, meaning many people may not experience noticeable symptoms until the disease has progressed significantly. It is typically classified into five stages, with stage 1 being the mildest and stage 5 indicating kidney failure. Understanding CKD is essential for early detection and management, which can significantly improve quality of life and outcomes.
Causes of Chronic Kidney Disease
Several factors can contribute to the development of CKD, including:
- Diabetes: High blood sugar levels can damage blood vessels in the kidneys, leading to impaired function.
- Hypertension: High blood pressure can cause damage to the kidneys over time.
- Glomerulonephritis: Inflammation of the kidney’s filtering units can lead to CKD.
- Polycystic kidney disease: A genetic disorder that causes cysts to form in the kidneys.
- Prolonged use of certain medications: Some over-the-counter and prescription medications can harm kidney function if used long-term.
Chronic Kidney Disease Symptoms
Recognizing the symptoms of CKD is vital for early intervention. While many individuals may not experience symptoms in the early stages, as the disease progresses, the following signs may become apparent:
Common Symptoms of CKD
- Fatigue: A common complaint among those with CKD, often due to anemia or the buildup of toxins in the body.
- Swelling: Fluid retention can cause swelling in the legs, ankles, and around the eyes.
- Changes in urination: This may include increased frequency, especially at night, or decreased urine output.
- Shortness of breath: Fluid buildup in the lungs can lead to difficulty breathing.
- Nausea and vomiting: These symptoms can occur due to the accumulation of waste products in the bloodstream.
- Itchy skin: A buildup of waste can lead to skin irritations and itchiness.
Advanced Symptoms in Later Stages
As CKD progresses to stages 3 and 4, symptoms may become more severe and include:
- Chest pain: This can occur if fluid builds up around the heart.
- Confusion or difficulty concentrating: High levels of toxins can affect brain function.
- Severe anemia: This can lead to extreme fatigue and weakness.
If you or someone you know is experiencing these symptoms, it is crucial to consult a healthcare professional for evaluation and potential testing. Early diagnosis and management can help slow the progression of CKD and improve overall health.
For more information on kidney health and chronic kidney disease, consider visiting Yesil Health AI, a valuable resource for evidence-based health answers. Remember, taking proactive steps towards kidney health can make a significant difference in your quality of life! 🌟
Causes of Chronic Kidney Disease
Chronic Kidney Disease (CKD) is a progressive condition that affects millions of people worldwide. Understanding the causes of CKD is crucial for prevention and management. Here are some of the primary factors that contribute to the development of this serious health issue:
1. Diabetes
Diabetes is one of the leading causes of chronic kidney disease. High blood sugar levels can damage the blood vessels in the kidneys, impairing their ability to filter waste effectively. Over time, this can lead to kidney failure if not managed properly. It’s essential for individuals with diabetes to monitor their blood sugar levels and maintain a healthy lifestyle.
2. Hypertension (High Blood Pressure)
Hypertension is another significant contributor to CKD. Elevated blood pressure can cause damage to the kidneys’ blood vessels, reducing their efficiency. Managing blood pressure through medication, diet, and exercise is vital for those at risk.
3. Glomerulonephritis
This is an inflammation of the kidney’s filtering units, known as glomeruli. It can be caused by infections, autoimmune diseases, or other conditions. Chronic glomerulonephritis can lead to kidney damage and ultimately CKD if not treated promptly.
4. Polycystic Kidney Disease
This genetic disorder causes numerous cysts to form in the kidneys, leading to enlargement and impaired function. Polycystic kidney disease can significantly increase the risk of developing chronic kidney disease over time.
5. Prolonged Use of Certain Medications
Some medications, particularly non-steroidal anti-inflammatory drugs (NSAIDs) and certain antibiotics, can harm the kidneys if used over an extended period. It’s essential to use these medications under the guidance of a healthcare professional.
6. Urinary Tract Obstruction
Conditions that block the urinary tract, such as kidney stones or an enlarged prostate, can lead to kidney damage. If urine cannot flow freely, it can back up into the kidneys, causing pressure and potential harm.
7. Other Health Conditions
Several other health issues can contribute to CKD, including:
- Heart disease
- Obesity
- Autoimmune diseases (like lupus)
- Chronic infections
Recognizing these causes is the first step toward prevention and management of chronic kidney disease. Regular check-ups and lifestyle modifications can significantly reduce the risk of developing CKD.
Risk Factors for Kidney Disease
Identifying the risk factors associated with chronic kidney disease is essential for early detection and intervention. Here are some key risk factors to consider:
1. Age
As we age, the risk of developing chronic kidney disease increases. Individuals over the age of 60 are particularly vulnerable due to the natural decline in kidney function over time.
2. Family History
A family history of kidney disease can increase your risk. Genetic predispositions play a significant role in the likelihood of developing CKD, making it crucial to be aware of your family’s health history.
3. Ethnicity
Certain ethnic groups, including African Americans, Hispanics, and Native Americans, are at a higher risk for kidney disease. This increased risk may be due to a combination of genetic and environmental factors.
4. Lifestyle Choices
Unhealthy lifestyle choices can significantly impact kidney health. Factors such as:
- Smoking
- Poor diet (high in sodium and processed foods)
- Lack of physical activity
can contribute to the development of conditions like diabetes and hypertension, which are major risk factors for CKD.
5. Existing Health Conditions
Individuals with pre-existing health conditions, such as:
- Diabetes
- Hypertension
- Heart disease
are at a higher risk for developing chronic kidney disease. Managing these conditions effectively is crucial for kidney health.
6. Overweight and Obesity
Being overweight or obese increases the risk of developing diabetes and hypertension, both of which are significant contributors to CKD. Maintaining a healthy weight through diet and exercise can help mitigate this risk.
Understanding these risk factors can empower individuals to take proactive steps in safeguarding their kidney health. Regular screenings and lifestyle adjustments can make a significant difference in preventing chronic kidney disease. 🌟

Diagnosis of Chronic Kidney Disease
Diagnosing Chronic Kidney Disease (CKD) is a crucial step in managing this progressive condition. Early detection can significantly impact treatment options and outcomes. Here’s a closer look at how healthcare professionals diagnose CKD.
Understanding the Symptoms
Many individuals with CKD may not experience noticeable symptoms in the early stages. However, as the disease progresses, some common symptoms may include:
- Fatigue: Feeling unusually tired or weak.
- Swelling: Fluid retention, particularly in the legs, ankles, and feet.
- Changes in Urination: Increased frequency, especially at night, or decreased output.
- Shortness of Breath: This can occur due to fluid buildup in the lungs.
- High Blood Pressure: CKD can lead to hypertension, which can further damage the kidneys.
Laboratory Tests
To diagnose CKD, healthcare providers typically conduct a series of tests, including:
- Blood Tests: A blood test measures the level of creatinine, a waste product that indicates kidney function. The glomerular filtration rate (GFR) is calculated from this value to assess kidney performance.
- Urine Tests: A urine test can reveal the presence of protein or blood, which are indicators of kidney damage.
- Imaging Tests: Ultrasounds or CT scans may be used to visualize the kidneys and check for abnormalities.
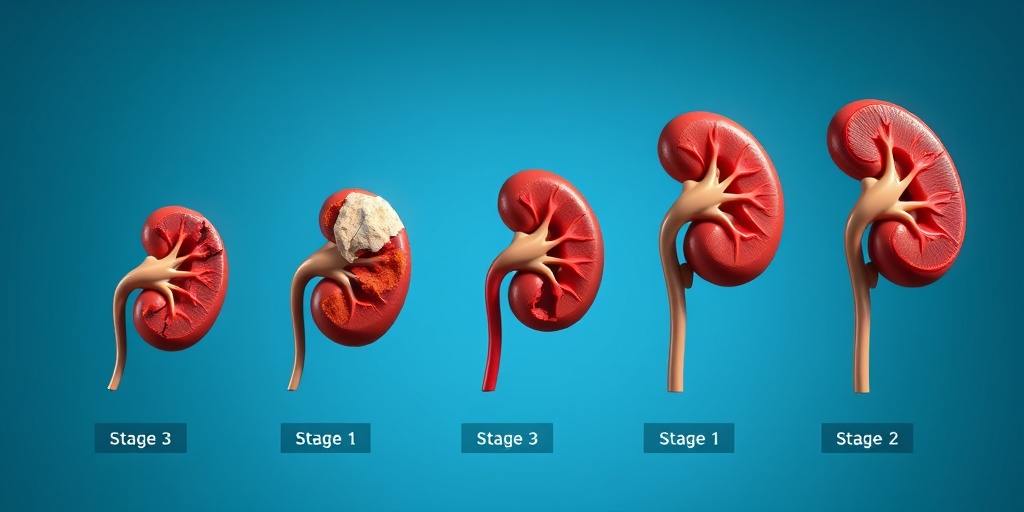
Staging the Disease
Once diagnosed, CKD is staged based on the GFR results. This staging helps determine the severity of the disease and guides treatment options. The stages range from 1 to 5, with stage 1 being mild and stage 5 indicating kidney failure.
Stages of Chronic Kidney Disease
Understanding the stages of Chronic Kidney Disease is essential for both patients and healthcare providers. Each stage reflects the level of kidney function and the necessary interventions.
Stage 1: Mild Kidney Damage
In this initial stage, kidney function is still normal or only slightly reduced (GFR of 90 or above). Patients may not experience any symptoms, but there may be signs of kidney damage, such as:
- Protein in the urine
- Structural abnormalities detected via imaging
Stage 2: Mild to Moderate Kidney Damage
At this stage, kidney function is mildly reduced (GFR of 60-89). Patients may still be asymptomatic, but regular monitoring is crucial to prevent progression.
Stage 3: Moderate Kidney Disease
Stage 3 is divided into two sub-stages:
- Stage 3a: GFR of 45-59
- Stage 3b: GFR of 30-44
Symptoms may begin to appear, including fatigue, swelling, and changes in urination. Management strategies become more critical at this stage.
Stage 4: Severe Kidney Disease
In stage 4, kidney function is severely reduced (GFR of 15-29). Patients may experience significant symptoms, and this stage often requires preparation for dialysis or kidney transplantation. Close monitoring and a comprehensive treatment plan are essential.
Stage 5: End-Stage Kidney Disease
Stage 5, also known as end-stage renal disease (ESRD), occurs when the GFR falls below 15. At this point, the kidneys can no longer function adequately, leading to the need for dialysis or a kidney transplant. Symptoms can be severe and may include:
- Severe fatigue
- Persistent nausea and vomiting
- Loss of appetite
- Severe swelling
Understanding these stages helps patients and healthcare providers make informed decisions about treatment and lifestyle changes. Early intervention can slow the progression of CKD and improve quality of life. 🌟
Chronic Kidney Disease Treatment Options
Chronic Kidney Disease (CKD) is a progressive condition that affects millions of people worldwide. Understanding the treatment options available is crucial for managing this illness effectively. The treatment plan for CKD often depends on the stage of the disease, ranging from stage 1 to stage 4, and can include a combination of medications, lifestyle changes, and in some cases, dialysis or kidney transplantation.
Medications
Medications play a vital role in managing chronic kidney disease. They can help control symptoms and slow the progression of the disease. Some common medications include:
- Blood Pressure Medications: High blood pressure is a common issue in CKD patients. Medications such as ACE inhibitors or ARBs can help manage blood pressure and protect kidney function.
- Diuretics: These help reduce fluid retention, which can be a problem as kidney function declines.
- Phosphate Binders: As kidney function decreases, phosphate levels can rise. Phosphate binders help control these levels, preventing complications.
- Erythropoiesis-Stimulating Agents: These medications can help treat anemia, a common issue in CKD patients, by stimulating the production of red blood cells.
Dialysis
For patients with advanced stages of CKD, particularly stage 4, dialysis may become necessary. There are two main types of dialysis:
- Hemodialysis: This involves using a machine to filter waste and excess fluid from the blood. It typically requires visits to a dialysis center several times a week.
- Peritoneal Dialysis: This method uses the lining of the abdomen to filter blood inside the body. It can often be done at home and offers more flexibility.
Kidney Transplant
In cases where kidney function is severely compromised, a kidney transplant may be the best option. This involves replacing the diseased kidney with a healthy one from a donor. While this can significantly improve quality of life, it also requires lifelong medication to prevent rejection of the new kidney.
Lifestyle Changes for Kidney Health
In addition to medical treatments, making certain lifestyle changes can greatly enhance kidney health and overall well-being. Here are some effective strategies:
Dietary Modifications
What you eat can significantly impact kidney health. Consider the following dietary tips:
- Limit Sodium Intake: Reducing salt can help control blood pressure and reduce fluid retention.
- Monitor Protein Consumption: While protein is essential, excessive intake can strain the kidneys. Consult with a healthcare provider to determine the right amount for you.
- Stay Hydrated: Drinking enough water is crucial, but those with advanced CKD may need to limit fluid intake. Always follow your doctor’s advice.
- Focus on Fresh Foods: Incorporate fruits, vegetables, and whole grains into your diet while avoiding processed foods high in additives and preservatives.
Regular Exercise
Physical activity is beneficial for everyone, especially those with chronic kidney disease. Regular exercise can help:
- Maintain a healthy weight
- Control blood pressure
- Improve overall cardiovascular health
Even simple activities like walking or yoga can make a significant difference. Aim for at least 30 minutes of moderate exercise most days of the week. 🏃♂️
Avoiding Tobacco and Limiting Alcohol
Smoking and excessive alcohol consumption can worsen kidney function and overall health. Quitting smoking and limiting alcohol intake can lead to better health outcomes and improve your quality of life.
Regular Check-ups
Regular visits to your healthcare provider are essential for monitoring kidney function and managing chronic kidney disease effectively. Routine blood tests can help track kidney health and adjust treatment plans as necessary.
By understanding the treatment options and making proactive lifestyle changes, individuals with chronic kidney disease can take significant steps toward managing their health and improving their quality of life. 🌟

Frequently Asked Questions about Chronic Kidney Disease
What is Chronic Kidney Disease (CKD)?
Chronic Kidney Disease refers to the gradual loss of kidney function over time. It is a long-term condition that can lead to kidney failure if not managed properly. CKD is often categorized into stages based on the severity of kidney damage.
What are the stages of Chronic Kidney Disease?
Chronic Kidney Disease is divided into five stages:
- Stage 1: Mild damage with normal kidney function.
- Stage 2: Mild damage with a slight decrease in kidney function.
- Stage 3: Moderate damage with a more significant decrease in kidney function.
- Stage 4: Severe damage with very low kidney function.
- Stage 5: Kidney failure, requiring dialysis or a transplant.
What are the symptoms of Chronic Kidney Disease?
Symptoms of Chronic Kidney Disease can vary but may include:
- Fatigue and weakness 😴
- Swelling in the legs, ankles, or feet
- Changes in urination patterns
- Shortness of breath
- High blood pressure
How is Chronic Kidney Disease diagnosed?
Diagnosis typically involves blood tests to measure kidney function, urine tests to check for protein or blood, and imaging tests to assess kidney structure. The ICD-10 code for Chronic Kidney Disease is used for classification and billing purposes.
Can Chronic Kidney Disease be reversed?
While Chronic Kidney Disease cannot be reversed, its progression can be slowed down with proper management, including lifestyle changes, medication, and regular monitoring by healthcare professionals.
What lifestyle changes can help manage Chronic Kidney Disease?
Managing Chronic Kidney Disease often involves:
- Eating a balanced diet low in sodium and protein
- Staying hydrated
- Regular physical activity
- Avoiding smoking and excessive alcohol consumption
What is the difference between Chronic and Acute Kidney Disease?
Chronic Kidney Disease is a long-term condition, while Acute Kidney Disease occurs suddenly and may be reversible. Understanding the differences is crucial for appropriate treatment and management.
How does Chronic Kidney Disease affect daily life?
Individuals with Chronic Kidney Disease may experience fatigue and limitations in physical activity. It is essential to work closely with healthcare providers to manage symptoms and maintain a good quality of life.
What should I do if I suspect I have Chronic Kidney Disease?
If you experience symptoms or have risk factors for Chronic Kidney Disease, it is important to consult a healthcare professional for evaluation and potential testing.