What Is Pulmonary Embolism?
Pulmonary embolism (PE) is a serious medical condition that occurs when a blood clot, often originating from the deep veins of the legs (a condition known as deep vein thrombosis or DVT), travels to the lungs and blocks a pulmonary artery. This blockage can prevent blood from reaching parts of the lung, leading to reduced oxygen levels in the bloodstream and potentially causing severe complications or even death if not treated promptly.
The meaning of pulmonary embolism can be understood as a blockage in the pulmonary arteries, which are crucial for transporting oxygen-rich blood from the heart to the lungs. When a clot obstructs these arteries, it can lead to significant health risks, making awareness and early detection vital.
Causes of Pulmonary Embolism
Several factors can contribute to the development of pulmonary embolism, including:
- Prolonged immobility: Long periods of sitting or lying down, such as during long flights or bed rest, can increase the risk of blood clots.
- Medical conditions: Certain conditions, like cancer, heart disease, or clotting disorders, can predispose individuals to embolism.
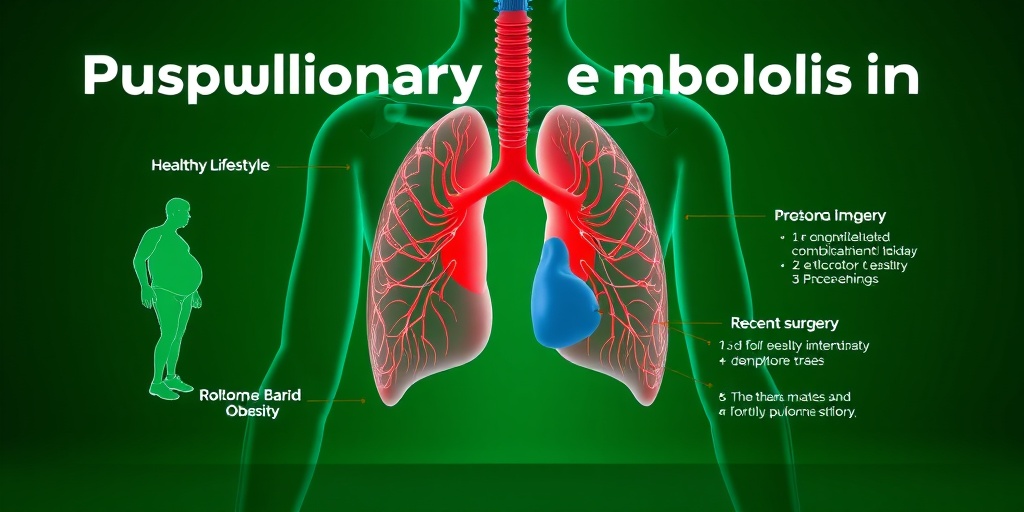
- Recent surgery: Surgical procedures, especially those involving the legs or pelvis, can increase the risk of clot formation.
- Obesity: Excess weight can put additional pressure on veins, increasing the likelihood of clot formation.
Risk Factors
Understanding the risk factors associated with pulmonary embolism is crucial for prevention. Some common risk factors include:
- Age: The risk increases with age, particularly for those over 60.
- Family history: A family history of blood clots can elevate your risk.
- Hormonal factors: Hormonal therapies, such as birth control pills or hormone replacement therapy, can increase clotting risk.
Pulmonary Embolism Symptoms
Recognizing the symptoms of pulmonary embolism is essential for timely intervention. Symptoms can vary widely depending on the size of the clot and the extent of the blockage. Some common symptoms include:
Common Symptoms
- Shortness of breath: This may occur suddenly and can worsen with exertion.
- Chest pain: Often described as sharp or stabbing, chest pain may mimic a heart attack.
- Coughing: This may include coughing up blood or blood-streaked sputum.
- Rapid heartbeat: An increased heart rate can be a sign of distress in the body.
Less Common Symptoms
In some cases, individuals may experience less common symptoms, such as:
- Dizziness or lightheadedness: This can occur due to reduced oxygen levels.
- Swelling in the legs: This may indicate DVT, which can lead to PE.
When to Seek Medical Attention
If you or someone you know experiences symptoms of pulmonary embolism, it is crucial to seek medical attention immediately. Early diagnosis and treatment can significantly improve outcomes and reduce the risk of severe complications.
For more information on pulmonary embolism, including treatment options and guidelines, consider visiting Yesil Health AI, a valuable resource for evidence-based health answers. Remember, understanding the signs and symptoms of pulmonary embolism can save lives! 🩺

Causes of Pulmonary Embolism
Pulmonary embolism (PE) is a serious condition that occurs when a blood clot blocks one or more arteries in the lungs. Understanding the causes of pulmonary embolism is crucial for prevention and timely treatment. The primary cause of PE is the formation of blood clots, which can originate from various parts of the body. Here are the main causes:
Deep Vein Thrombosis (DVT)
The most common cause of pulmonary embolism is deep vein thrombosis (DVT). DVT occurs when a blood clot forms in the deep veins of the legs or other parts of the body. If a piece of this clot breaks off, it can travel to the lungs, leading to a pulmonary embolism. Factors that contribute to DVT include:
- Prolonged immobility: Sitting for long periods, such as during long flights or car rides.
- Injury or surgery: Trauma or surgical procedures can increase the risk of clot formation.
- Hormonal changes: Hormonal therapies, including birth control pills, can elevate the risk.
Fat Embolism
Another less common cause of pulmonary embolism is a fat embolism, which can occur after fractures of long bones or during certain surgical procedures. Fat globules can enter the bloodstream and travel to the lungs, causing blockage.
Air Embolism
Air embolism happens when air bubbles enter the bloodstream, which can occur during certain medical procedures or injuries. These air bubbles can obstruct blood flow in the lungs, leading to pulmonary embolism.
Amniotic Fluid Embolism
In rare cases, amniotic fluid embolism can occur during childbirth. This happens when amniotic fluid enters the mother’s bloodstream, potentially causing severe complications, including pulmonary embolism.
Risk Factors for Pulmonary Embolism
Identifying the risk factors for pulmonary embolism is essential for prevention and early intervention. While anyone can develop PE, certain factors increase the likelihood of its occurrence. Here are some key risk factors:
Age
As individuals age, the risk of developing blood clots increases. People over the age of 60 are at a higher risk for pulmonary embolism due to age-related changes in blood flow and clotting mechanisms.
Obesity
Obesity is a significant risk factor for pulmonary embolism. Excess weight can put additional pressure on veins, making it more difficult for blood to flow properly and increasing the likelihood of clot formation.
Medical Conditions
Several medical conditions can elevate the risk of pulmonary embolism, including:
- Heart disease: Conditions that affect heart function can increase the risk of clot formation.
- Cancer: Certain cancers and their treatments can lead to a higher risk of blood clots.
- Autoimmune disorders: Conditions like lupus can affect blood clotting and increase the risk of PE.
Family History
A family history of blood clots or clotting disorders can increase an individual’s risk of developing pulmonary embolism. Genetic factors play a significant role in how the body regulates blood clotting.
Prolonged Immobility
Periods of prolonged immobility, such as during long flights or bed rest after surgery, can significantly increase the risk of developing DVT, which can lead to pulmonary embolism. It’s essential to move around and stretch during long periods of inactivity.
Smoking
Smoking is a well-known risk factor for various health issues, including pulmonary embolism. It damages blood vessels and increases the likelihood of clot formation, making smokers more susceptible to PE.
Understanding the causes and risk factors of pulmonary embolism is vital for prevention and early detection. If you or someone you know exhibits symptoms such as sudden shortness of breath, chest pain, or coughing up blood, seek medical attention immediately. 🩺
Diagnosing Pulmonary Embolism
Diagnosing pulmonary embolism (PE) can be a complex process due to the variety of symptoms that may mimic other conditions. It is crucial for healthcare providers to accurately identify PE to initiate timely treatment. Here, we will explore the common diagnostic methods used to confirm the presence of a pulmonary embolism.
Clinical Assessment
The first step in diagnosing pulmonary embolism often involves a thorough clinical assessment. Healthcare professionals will typically evaluate the patient’s medical history and perform a physical examination. Key symptoms to look for include:
- Shortness of breath: Sudden onset of difficulty breathing is a hallmark symptom.
- Chest pain: This may feel sharp or stabbing and can worsen with deep breaths.
- Cough: Sometimes accompanied by blood-streaked sputum.
- Rapid heart rate: An increased heart rate can indicate stress on the heart.
Imaging Tests
Once a healthcare provider suspects a pulmonary embolism, imaging tests are often employed to confirm the diagnosis. The most common tests include:
- CT Pulmonary Angiography (CTPA): This is the gold standard for diagnosing PE. It provides detailed images of the blood vessels in the lungs and can identify blockages.
- Ventilation-Perfusion (V/Q) Scan: This test assesses airflow and blood flow in the lungs. It is particularly useful for patients who cannot undergo a CT scan.
- Ultrasound: A Doppler ultrasound of the legs can help identify deep vein thrombosis (DVT), which is often the source of emboli.
Blood Tests
Blood tests can also play a role in the diagnosis of pulmonary embolism. The D-dimer test measures the presence of a substance released when a blood clot breaks up. Elevated levels may suggest the presence of an embolism, but they are not definitive. Therefore, further testing is usually required.
Electrocardiogram (ECG)
An electrocardiogram (ECG) may be performed to assess the heart’s electrical activity. While it cannot definitively diagnose PE, certain changes in the ECG can indicate strain on the heart due to a pulmonary embolism.
Complications of Pulmonary Embolism
While timely diagnosis and treatment of pulmonary embolism can significantly improve outcomes, complications can still arise. Understanding these potential complications is essential for both patients and healthcare providers.
Chronic Thromboembolic Pulmonary Hypertension (CTEPH)
One of the most serious long-term complications of pulmonary embolism is chronic thromboembolic pulmonary hypertension (CTEPH). This condition occurs when blood clots in the lungs do not dissolve and lead to increased blood pressure in the pulmonary arteries. Symptoms may include:
- Shortness of breath: Especially during physical activity.
- Fatigue: A general feeling of tiredness that does not improve with rest.
- Chest pain: Persistent discomfort that may mimic angina.
Right Heart Failure
Severe pulmonary embolism can lead to right heart failure, as the right side of the heart struggles to pump blood through the blocked pulmonary arteries. This can result in symptoms such as:
- Swelling in the legs and ankles: Due to fluid retention.
- Rapid heartbeat: As the heart works harder to compensate.
- Fainting or dizziness: Resulting from reduced blood flow.
Recurrence of Pulmonary Embolism
Patients who have experienced a pulmonary embolism are at an increased risk of recurrence. Factors that may contribute to this risk include:
- Underlying conditions: Such as clotting disorders or prolonged immobility.
- Inadequate treatment: Not adhering to anticoagulation therapy can lead to new clots.
Preventive measures, including lifestyle changes and medication adherence, are crucial for reducing the risk of recurrence.
Conclusion
Understanding the diagnostic process and potential complications of pulmonary embolism is vital for effective management and improved patient outcomes. If you or someone you know is experiencing symptoms associated with PE, seeking immediate medical attention is essential. 🩺

Treatment Options for Pulmonary Embolism
Pulmonary embolism (PE) is a serious condition that occurs when a blood clot blocks a blood vessel in the lungs. Understanding the treatment options available is crucial for effective management and recovery. Here, we’ll explore various treatment modalities, their effectiveness, and when they are typically used.
1. Anticoagulants
Anticoagulants, commonly known as blood thinners, are the first line of treatment for pulmonary embolism. They work by preventing new clots from forming and stopping existing clots from growing. Some commonly used anticoagulants include:
- Heparin: Often administered intravenously in a hospital setting for immediate effect.
- Warfarin: An oral medication that requires regular monitoring of blood levels.
- Direct Oral Anticoagulants (DOACs): These include medications like rivaroxaban and apixaban, which do not require regular blood tests.
Choosing the right anticoagulant depends on various factors, including the patient’s overall health, the severity of the embolism, and any other underlying conditions.
2. Thrombolytics
In more severe cases of pulmonary embolism, thrombolytics may be used. These medications, also known as “clot busters,” work to dissolve blood clots quickly. They are typically reserved for life-threatening situations due to their potential for serious side effects, such as bleeding. Thrombolytics are administered in a hospital setting under close supervision.
3. Surgical Interventions
For patients who cannot tolerate anticoagulants or thrombolytics, surgical options may be considered. The most common surgical procedure for pulmonary embolism is:
- Embolectomy: This is a surgical procedure to remove the clot from the pulmonary artery. It is usually performed in emergency situations.
Additionally, a vena cava filter may be placed in the inferior vena cava to prevent future clots from reaching the lungs. This is often recommended for patients with recurrent embolisms despite anticoagulation therapy.
4. Supportive Care
Alongside medical treatments, supportive care plays a vital role in managing pulmonary embolism. This may include:
- Oxygen therapy: To ensure adequate oxygen levels in the blood.
- Pain management: To alleviate discomfort associated with the condition.
- Physical therapy: To help regain strength and mobility post-treatment.
Each treatment plan should be tailored to the individual, taking into account their specific circumstances and health status.
Preventing Pulmonary Embolism
Preventing pulmonary embolism is essential, especially for individuals at higher risk. Here are some effective strategies to reduce the likelihood of developing this serious condition.
1. Lifestyle Modifications
Making certain lifestyle changes can significantly lower the risk of pulmonary embolism:
- Stay Active: Regular physical activity promotes healthy blood circulation. Aim for at least 150 minutes of moderate exercise each week.
- Maintain a Healthy Weight: Obesity is a significant risk factor for blood clots. A balanced diet and regular exercise can help manage weight.
- Avoid Prolonged Immobility: If you are traveling long distances or are bedridden, take breaks to move around and stretch your legs.
2. Medical Management
For individuals with a history of blood clots or other risk factors, medical management is crucial:
- Anticoagulant Therapy: As a preventive measure, doctors may prescribe anticoagulants for high-risk patients.
- Compression Stockings: These can help improve blood flow in the legs and reduce the risk of clot formation.
3. Awareness and Education
Understanding the signs and symptoms of pulmonary embolism is vital for early detection and treatment. Common symptoms include:
- Shortness of breath
- Chest pain, especially when breathing deeply
- Coughing up blood
Being aware of these symptoms can lead to prompt medical attention, which is critical for improving outcomes.
In conclusion, while pulmonary embolism is a serious condition, understanding the treatment options and preventive measures can significantly enhance patient outcomes and reduce risks. Stay informed and proactive about your health! 🌟
Frequently Asked Questions about Pulmonary Embolism
What is an embolism pulmonary?
Embolism pulmonary refers to a blockage in one of the pulmonary arteries in the lungs, usually caused by blood clots that travel to the lungs from the legs or other parts of the body (deep vein thrombosis). This condition can be life-threatening and requires immediate medical attention.
What are the symptoms of embolism pulmonary?
Common embolism pulmonary symptoms include:
- Shortness of breath
- Chest pain that may become worse when breathing deeply
- Coughing up blood
- Rapid heart rate
- Dizziness or fainting
If you experience any of these symptoms, seek medical help immediately! 🚑
How is embolism pulmonary diagnosed?
Diagnosis of embolism pulmonary typically involves a combination of medical history, physical examination, and diagnostic tests such as:
- CT pulmonary angiography
- Ventilation-perfusion (V/Q) scan
- Ultrasound of the legs to check for deep vein thrombosis
- Blood tests, including D-dimer tests
What are the treatment options for embolism pulmonary?
Treatment for embolism pulmonary may include:
- Anticoagulants (blood thinners) to prevent further clotting
- Thrombolytics (clot busters) in severe cases
- Inferior vena cava (IVC) filter to prevent clots from reaching the lungs
- Surgery in critical situations to remove the clot
What is the ICD-10 code for embolism pulmonary?
The ICD-10 code for embolism pulmonary is I26. This code is used for medical billing and documentation purposes.
Are there guidelines for managing embolism pulmonary?
Yes, there are established embolism pulmonary guidelines that provide recommendations for diagnosis, treatment, and prevention. These guidelines are regularly updated based on the latest research and clinical practices.
Can an ECG detect embolism pulmonary?
An ECG (electrocardiogram) can help identify heart strain or other issues related to embolism pulmonary, but it is not a definitive diagnostic tool. It is often used in conjunction with other tests for a comprehensive evaluation.
Where can I find more information about embolism pulmonary?
For more detailed information, you can refer to reputable medical sources such as the New England Journal of Medicine (NEJM) or specialized medical websites like Radiopaedia.
What should I do if I suspect I have embolism pulmonary?
If you suspect you have embolism pulmonary, it is crucial to seek emergency medical care immediately. Early diagnosis and treatment can significantly improve outcomes. 🏥