What Is Diabetic Retinopathy?
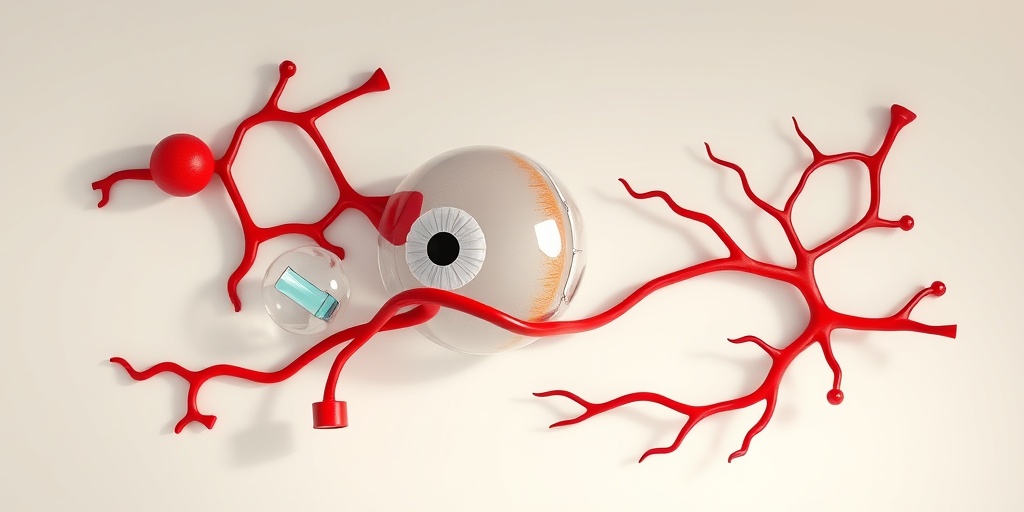
Diabetic retinopathy is a serious eye condition that affects individuals with diabetes. It occurs when high blood sugar levels damage the blood vessels in the retina, the light-sensitive tissue at the back of the eye. This condition can lead to vision impairment and, in severe cases, blindness if not managed properly. Understanding diabetic retinopathy is crucial for anyone living with diabetes, as early detection and treatment can significantly reduce the risk of severe complications.
The Connection Between Diabetes and Eye Health
Diabetes can lead to various complications, and eye health is one of the most affected areas. Over time, elevated blood sugar levels can cause the blood vessels in the retina to swell, leak, or become blocked. This damage can progress through different stages, leading to diabetic retinopathy. It’s essential for individuals with diabetes to monitor their blood sugar levels and maintain a healthy lifestyle to minimize the risk of developing this condition.
Stages of Diabetic Retinopathy
Diabetic retinopathy progresses through several stages:
- Non-proliferative Diabetic Retinopathy (NPDR): This early stage involves the swelling of blood vessels and the formation of small bulges called microaneurysms. Patients may not experience noticeable symptoms at this stage.
- Proliferative Diabetic Retinopathy (PDR): In this advanced stage, new, abnormal blood vessels begin to grow on the retina’s surface. These vessels are fragile and can bleed, leading to more severe vision problems.
Regular eye exams are vital for detecting these stages early, allowing for timely intervention and treatment.
Diabetic Retinopathy Symptoms
Recognizing the symptoms of diabetic retinopathy is essential for early diagnosis and treatment. Many individuals may not notice symptoms until the condition has progressed significantly. Here are some common symptoms to watch for:
Common Symptoms
- Blurred Vision: One of the first signs of diabetic retinopathy can be blurred or distorted vision, which may fluctuate.
- Dark or Empty Areas in Vision: Patients may notice dark spots or empty areas in their field of vision, making it difficult to see clearly.
- Difficulty Seeing at Night: Night vision may become impaired, making it challenging to navigate in low-light conditions.
- Floaters: The appearance of floaters—tiny specks or strings that drift across the field of vision—can indicate retinal damage.
- Sudden Vision Loss: In severe cases, individuals may experience sudden and complete vision loss, which requires immediate medical attention.
When to Seek Medical Attention
If you have diabetes and notice any of these symptoms, it’s crucial to consult an eye care professional promptly. Regular screenings and eye exams can help detect diabetic retinopathy before significant damage occurs. Early intervention can lead to better outcomes and preserve vision.
Conclusion
Diabetic retinopathy is a serious condition that can have a profound impact on your quality of life. By understanding what it is and recognizing the symptoms, you can take proactive steps to protect your vision. Remember, maintaining good blood sugar control and scheduling regular eye exams are key to preventing this condition. For more information and resources on managing diabetes and its complications, consider visiting Yesil Health AI, where you can find evidence-based health answers tailored to your needs. 🩺👁️

Stages of Diabetic Retinopathy
Diabetic retinopathy is a serious eye condition that can affect individuals with diabetes. Understanding the stages of diabetic retinopathy is crucial for early detection and effective management. The condition progresses through several stages, each with distinct characteristics and implications for vision.
1. Mild Nonproliferative Retinopathy
This is the earliest stage of diabetic retinopathy. At this point, small areas of swelling, known as microaneurysms, develop in the blood vessels of the retina. These changes may not cause any noticeable symptoms, making regular eye exams essential for individuals with diabetes.
2. Moderate Nonproliferative Retinopathy
As the condition progresses, more blood vessels become blocked, leading to further retinal damage. In this stage, individuals may begin to experience some vision changes, although many still do not notice significant symptoms. Regular screenings are vital to monitor the progression of the disease.
3. Severe Nonproliferative Retinopathy
In this stage, a larger number of blood vessels are blocked, which can lead to a lack of oxygen in the retina. This oxygen deprivation can cause the retina to send signals to the body to create new blood vessels. However, these new vessels are often weak and can lead to complications.
4. Proliferative Diabetic Retinopathy (PDR)
This is the most advanced stage of diabetic retinopathy. In PDR, new blood vessels grow on the surface of the retina and can bleed into the vitreous, leading to severe vision loss. Symptoms may include sudden vision changes, floaters, or even complete loss of vision. Immediate medical attention is crucial at this stage.
Causes and Risk Factors
Understanding the causes and risk factors associated with diabetic retinopathy can help individuals take proactive steps to protect their vision. The primary cause of this condition is prolonged high blood sugar levels, which can damage the blood vessels in the retina.
1. High Blood Sugar Levels
Chronic hyperglycemia (high blood sugar) is the leading cause of diabetic retinopathy. Over time, elevated glucose levels can weaken the blood vessels in the retina, leading to leakage and swelling.
2. Duration of Diabetes
The longer a person has diabetes, the greater their risk of developing diabetic retinopathy. Individuals with type 1 diabetes are at risk after about five years, while those with type 2 diabetes may develop the condition shortly after diagnosis.
3. Blood Pressure and Cholesterol Levels
High blood pressure and elevated cholesterol levels can exacerbate the damage to retinal blood vessels. Maintaining healthy blood pressure and cholesterol levels is essential for reducing the risk of diabetic retinopathy.
4. Other Health Conditions
Conditions such as kidney disease and cardiovascular disease can increase the risk of diabetic retinopathy. These comorbidities often indicate a more severe form of diabetes, which can lead to complications in the eyes.
5. Lifestyle Factors
- Smoking: Tobacco use can worsen blood vessel health and increase the risk of diabetic complications.
- Obesity: Excess weight can lead to insulin resistance, making diabetes management more challenging.
- Lack of Physical Activity: Regular exercise helps control blood sugar levels and improve overall health.
By understanding the causes and risk factors associated with diabetic retinopathy, individuals can take proactive measures to manage their diabetes effectively and reduce the risk of vision loss. Regular eye exams and maintaining a healthy lifestyle are key components in the prevention and management of this condition. 🩺👁️
Diagnosis of Diabetic Retinopathy
Diagnosing diabetic retinopathy is a crucial step in managing diabetes and preventing vision loss. This condition, which affects the blood vessels in the retina, can develop silently, often without noticeable symptoms in its early stages. Therefore, regular eye examinations are essential for individuals with diabetes.
Importance of Regular Eye Exams
For those living with diabetes, it is recommended to have a comprehensive eye exam at least once a year. During these exams, eye care professionals can detect early signs of diabetic retinopathy before significant damage occurs. Early detection is key to effective management and treatment.
Diagnostic Tests
Several tests are commonly used to diagnose diabetic retinopathy:
- Visual Acuity Test: This test measures how well you can see at various distances. It helps determine if your vision has been affected.
- Dilated Eye Exam: Eye drops are used to widen (dilate) your pupils, allowing the doctor to examine the retina for any signs of damage.
- Optical Coherence Tomography (OCT): This imaging test provides cross-sectional images of the retina, helping to identify swelling and other changes.
- Fluorescein Angiography: A special dye is injected into your arm, and photographs of the retina are taken to identify blood vessel leakage or abnormal growth.
These tests help in grading the severity of diabetic retinopathy, which is essential for determining the appropriate treatment plan.
Understanding the Stages of Diabetic Retinopathy
Diabetic retinopathy progresses through several stages:
- Non-Proliferative Diabetic Retinopathy (NPDR): This early stage involves mild changes in the retina, such as microaneurysms and retinal hemorrhages.
- Moderate NPDR: As the condition progresses, more blood vessels become blocked, leading to further retinal damage.
- Severe NPDR: Many blood vessels are blocked, and the risk of vision loss increases significantly.
- Proliferative Diabetic Retinopathy (PDR): This advanced stage involves the growth of new, abnormal blood vessels that can bleed into the retina, causing severe vision impairment.
Understanding these stages helps patients and healthcare providers make informed decisions about monitoring and treatment.
Treatment Options Available
Once diagnosed, there are several treatment options available for diabetic retinopathy, depending on the severity of the condition.
Monitoring and Lifestyle Changes
For patients in the early stages of diabetic retinopathy, close monitoring and lifestyle changes may be sufficient. This includes:
- Controlling Blood Sugar Levels: Maintaining optimal blood glucose levels can slow the progression of the disease.
- Regular Exercise: Engaging in physical activity can improve overall health and help manage diabetes.
- Healthy Diet: A balanced diet rich in fruits, vegetables, and whole grains can support eye health.
Medical Treatments
For more advanced stages of diabetic retinopathy, medical interventions may be necessary:
- Laser Treatment: This procedure, known as photocoagulation, uses laser technology to seal leaking blood vessels or to reduce the growth of new blood vessels.
- Injections: Medications such as anti-VEGF (vascular endothelial growth factor) agents can be injected into the eye to reduce swelling and prevent further vision loss.
- Surgery: In severe cases, a vitrectomy may be performed to remove blood from the eye and scar tissue that may be pulling on the retina.
Emerging Treatments
Research is ongoing to find new treatments for diabetic retinopathy. Some promising areas include:
- Gene Therapy: This innovative approach aims to correct the underlying genetic issues that contribute to the disease.
- Stem Cell Therapy: Researchers are exploring the potential of stem cells to regenerate damaged retinal cells.
As treatments evolve, staying informed about the latest advancements can empower patients to make the best choices for their eye health. 🩺

Living with Diabetic Retinopathy
Living with diabetic retinopathy can be a challenging experience, especially for those who are navigating the complexities of diabetes management. This condition, which affects the eyes, is a common complication of diabetes and can lead to serious vision problems if not addressed promptly. Understanding how to cope with this condition is crucial for maintaining both your vision and overall quality of life.
Understanding Diabetic Retinopathy
Diabetic retinopathy occurs when high blood sugar levels damage the blood vessels in the retina, the light-sensitive tissue at the back of the eye. This damage can lead to vision impairment and, in severe cases, blindness. It’s essential to recognize the symptoms early on to seek appropriate treatment. Common symptoms include:
- Blurred vision
- Dark spots or floaters in your vision
- Difficulty seeing at night
- Sudden vision loss
Managing Daily Life with Diabetic Retinopathy
For those diagnosed with diabetic retinopathy, managing daily life involves a combination of medical treatment and lifestyle adjustments. Here are some strategies to help you cope:
- Regular Eye Exams: Schedule regular check-ups with your eye doctor to monitor the progression of the disease. Early detection is key to preventing severe vision loss.
- Blood Sugar Control: Keeping your blood sugar levels within the target range can slow the progression of diabetic retinopathy. Work closely with your healthcare team to develop a personalized diabetes management plan.
- Healthy Lifestyle Choices: Incorporate a balanced diet rich in fruits, vegetables, and whole grains. Regular physical activity can also help manage blood sugar levels.
- Support Systems: Connect with support groups or counseling services. Sharing experiences with others facing similar challenges can provide emotional relief and practical advice.
Emotional and Psychological Impact
Living with a chronic condition like diabetic retinopathy can take a toll on your mental health. It’s normal to feel anxious or depressed about potential vision loss. Consider the following tips to support your emotional well-being:
- Stay Informed: Educate yourself about the condition. Understanding what to expect can alleviate fears and empower you to take control of your health.
- Mindfulness and Relaxation Techniques: Practices such as meditation, yoga, or deep-breathing exercises can help reduce stress and improve your overall outlook.
- Seek Professional Help: If feelings of anxiety or depression persist, don’t hesitate to reach out to a mental health professional for support.
Preventing Diabetic Retinopathy
Prevention is always better than cure, especially when it comes to diabetic retinopathy. While not all cases can be prevented, there are several proactive steps you can take to significantly reduce your risk of developing this condition.
Control Your Blood Sugar Levels
One of the most effective ways to prevent diabetic retinopathy is to maintain optimal blood sugar levels. Here are some tips:
- Monitor Your Blood Sugar: Regularly check your blood sugar levels to ensure they remain within your target range.
- Follow a Meal Plan: Work with a dietitian to create a meal plan that helps manage your blood sugar levels effectively.
- Stay Active: Engage in regular physical activity, which can help lower blood sugar levels and improve insulin sensitivity.
Regular Eye Screenings
Early detection is crucial in preventing vision loss from diabetic retinopathy. Schedule comprehensive eye exams at least once a year, or more frequently if recommended by your eye care professional. During these exams, your doctor can:
- Check for early signs of retinopathy
- Provide guidance on managing your eye health
- Discuss treatment options if necessary
Healthy Lifestyle Choices
In addition to managing blood sugar levels, adopting a healthy lifestyle can play a significant role in preventing diabetic retinopathy. Consider these lifestyle changes:
- Avoid Smoking: Smoking can worsen blood circulation and increase the risk of diabetic complications.
- Limit Alcohol Consumption: Excessive alcohol can lead to fluctuations in blood sugar levels.
- Maintain a Healthy Weight: Achieving and maintaining a healthy weight can help control blood sugar levels and reduce the risk of complications.
By taking these preventive measures, you can significantly reduce your risk of developing diabetic retinopathy and protect your vision for the future. Remember, proactive management is key! 🌟

Frequently Asked Questions about Diabetic Retinopathy
What is Diabetic Retinopathy?
Diabetic Retinopathy is a diabetes-related eye condition that affects the retina, the light-sensitive tissue at the back of the eye. It occurs when high blood sugar levels damage the blood vessels in the retina, leading to vision problems.
What are the symptoms of Diabetic Retinopathy?
Common diabetic retinopathy symptoms include:
- Blurred or distorted vision
- Dark or empty areas in your vision
- Difficulty seeing at night
- Sudden vision loss
What are the stages of Diabetic Retinopathy?
Diabetic Retinopathy progresses through several stages:
- Non-proliferative Diabetic Retinopathy (NPDR): Early stage with mild symptoms.
- Proliferative Diabetic Retinopathy (PDR): Advanced stage where new blood vessels grow, which can lead to serious vision loss.
How is Diabetic Retinopathy treated?
Treatment options for diabetic retinopathy may include:
- Laser therapy to reduce swelling and prevent vision loss
- Injections of medication into the eye to control inflammation
- Surgery in severe cases to remove the vitreous gel and blood from the eye
What is the ICD-10 code for Diabetic Retinopathy?
The ICD-10 code for diabetic retinopathy varies based on the specific type and severity. Common codes include:
- E11.359 – Type 2 diabetes with unspecified diabetic retinopathy
- E10.359 – Type 1 diabetes with unspecified diabetic retinopathy
How is Diabetic Retinopathy graded?
Grading of diabetic retinopathy is typically done based on the severity of the condition, which can be classified into:
- Mild NPDR
- Moderate NPDR
- Severe NPDR
- PDR
How does Diabetic Retinopathy affect vision?
Diabetic retinopathy can lead to significant vision impairment or loss if not treated. It can cause blurred vision, difficulty seeing colors, and even complete vision loss in advanced stages.
What is the importance of screening for Diabetic Retinopathy?
Regular diabetic retinopathy screening is crucial for early detection and treatment, which can help prevent severe vision loss. It is recommended that individuals with diabetes have their eyes examined at least once a year.
Can Diabetic Retinopathy be reversed?
While diabetic retinopathy cannot be completely reversed, early detection and treatment can significantly slow its progression and preserve vision.
What lifestyle changes can help manage Diabetic Retinopathy?
To manage diabetic retinopathy, consider the following lifestyle changes:
When should I see a doctor about Diabetic Retinopathy?
If you experience any symptoms of diabetic retinopathy, such as sudden vision changes or persistent blurred vision, it is important to consult a healthcare professional promptly.




