What Is Diabetic Eye Disease?
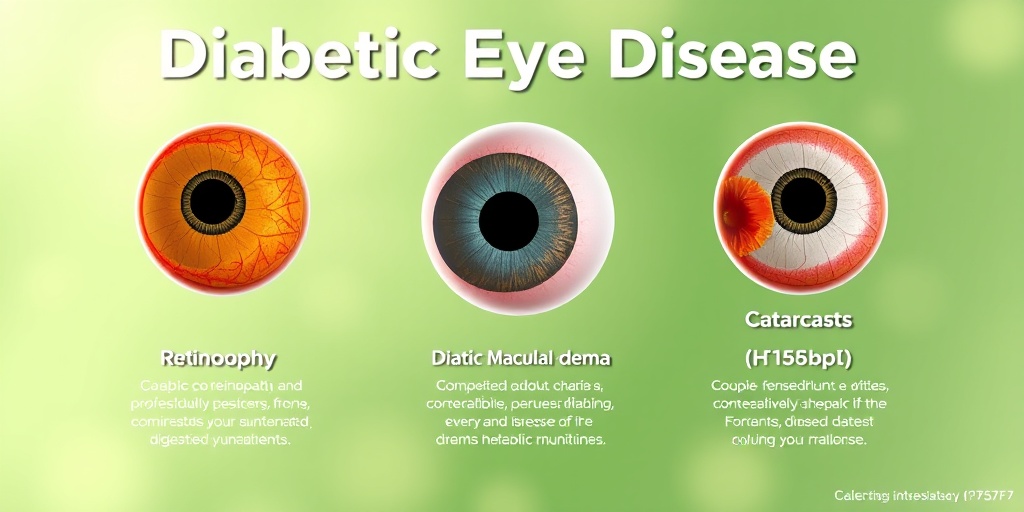
Diabetic Eye Disease refers to a group of eye conditions that can affect individuals with diabetes, primarily due to prolonged high blood sugar levels. This condition is a significant concern as it can lead to serious complications, including vision loss. The most common types of diabetic eye diseases include diabetic retinopathy, diabetic macular edema, and cataracts. Understanding these conditions is crucial for anyone living with diabetes, as early detection and treatment can help preserve vision.
Types of Diabetic Eye Disease
- Diabetic Retinopathy: This is the most prevalent form of diabetic eye disease. It occurs when high blood sugar levels damage the blood vessels in the retina, leading to vision problems.
- Diabetic Macular Edema: This condition is a result of fluid accumulation in the macula, the part of the retina responsible for sharp vision. It can occur at any stage of diabetic retinopathy.
- Cataracts: People with diabetes are at a higher risk of developing cataracts, which cloud the lens of the eye and can lead to blurred vision.
Each of these conditions can progress without noticeable symptoms, making regular eye examinations essential for those with diabetes. If you or someone you know is living with diabetes, staying informed about diabetic eye disease is vital for maintaining eye health.
Symptoms of Diabetic Eye Disease
Recognizing the symptoms of diabetic eye disease early can make a significant difference in treatment outcomes. Here are some common symptoms to watch for:
Common Symptoms
- Blurred Vision: One of the first signs that something may be wrong with your eyes is blurred or distorted vision. This can occur suddenly or gradually.
- Floaters: You may notice small spots or strings that float across your field of vision. These are often harmless but can indicate underlying issues.
- Dark or Empty Areas in Vision: Some individuals may experience dark spots or areas where vision is missing, which can be alarming.
- Difficulty Seeing at Night: If you find it increasingly challenging to see in low light conditions, this could be a symptom of diabetic eye disease.
- Sudden Vision Loss: This is a serious symptom that requires immediate medical attention. If you experience sudden vision loss, seek help right away.
When to See a Doctor
If you have diabetes and notice any of these symptoms, it’s crucial to consult with an eye care professional as soon as possible. Regular eye exams are essential, even if you don’t notice any symptoms. The American Diabetes Association recommends that individuals with diabetes have a comprehensive eye exam at least once a year.
In addition to regular check-ups, managing your diabetes through a healthy diet, regular exercise, and medication can significantly reduce the risk of developing diabetic eye disease. For more information on managing diabetes and its complications, consider visiting Yesil Health AI, a valuable resource for evidence-based health answers.
In conclusion, being aware of diabetic eye disease and its symptoms is crucial for anyone living with diabetes. Early detection and treatment can help preserve vision and improve quality of life. Stay proactive about your eye health, and don’t hesitate to reach out to healthcare professionals for guidance and support. 👁️✨

Causes and Risk Factors
Diabetic eye disease, also known as diabetic retinopathy, is a serious complication of diabetes that can lead to vision loss. Understanding the causes and risk factors associated with this condition is crucial for prevention and early detection.
What Causes Diabetic Eye Disease?
The primary cause of diabetic eye disease is prolonged high blood sugar levels, which can damage the blood vessels in the retina. Here’s how it happens:
- High Blood Sugar Levels: Over time, elevated glucose levels can lead to the swelling and leakage of blood vessels in the retina, causing vision problems.
- Increased Blood Pressure: Hypertension often accompanies diabetes and can exacerbate damage to the retinal blood vessels.
- High Cholesterol: Elevated cholesterol levels can contribute to the hardening of blood vessels, further impairing blood flow to the retina.
Risk Factors for Diabetic Eye Disease
Several factors can increase the likelihood of developing diabetic eye disease:
- Duration of Diabetes: The longer a person has diabetes, the higher the risk of developing eye complications. Regular eye exams are essential for those with diabetes.
- Type of Diabetes: Individuals with Type 1 diabetes are at a higher risk for diabetic eye disease compared to those with Type 2 diabetes, especially if their blood sugar levels are not well controlled.
- Age: Older adults are more susceptible to diabetic eye disease, particularly if they have had diabetes for many years.
- Family History: A family history of diabetes or eye diseases can increase your risk.
- Obesity: Being overweight can lead to insulin resistance, worsening blood sugar control and increasing the risk of diabetic complications.
- Smoking: Tobacco use can damage blood vessels and worsen overall health, increasing the risk of diabetic eye disease.
Types of Diabetic Eye Disease
Diabetic eye disease encompasses several conditions that can affect the eyes of individuals with diabetes. Understanding these types can help in recognizing symptoms and seeking timely treatment.
1. Diabetic Retinopathy
This is the most common form of diabetic eye disease. It occurs when high blood sugar levels damage the blood vessels in the retina. Diabetic retinopathy can be classified into two stages:
- Non-Proliferative Diabetic Retinopathy (NPDR): In this early stage, blood vessels may swell and leak fluid into the retina, leading to vision changes.
- Proliferative Diabetic Retinopathy (PDR): This advanced stage involves the growth of new, abnormal blood vessels in the retina, which can bleed and cause severe vision loss.
2. Diabetic Macular Edema (DME)
DME is a complication of diabetic retinopathy that occurs when fluid accumulates in the macula, the part of the retina responsible for sharp central vision. Symptoms may include:
- Blurry or distorted vision
- Difficulty reading or seeing faces clearly
3. Cataracts
People with diabetes are at a higher risk of developing cataracts, which is a clouding of the lens in the eye. Symptoms include:
- Cloudy or blurry vision
- Increased sensitivity to glare
- Difficulty seeing at night
4. Glaucoma
Diabetes can also increase the risk of glaucoma, a condition that damages the optic nerve, often due to increased pressure in the eye. Symptoms may include:
- Loss of peripheral vision
- Seeing halos around lights
Recognizing the types of diabetic eye disease and their symptoms is vital for early intervention. Regular eye check-ups and maintaining good blood sugar control can significantly reduce the risk of these complications. 🩺👁️
Diagnosis of Diabetic Eye Disease
Diabetic eye disease, also known as diabetic retinopathy, is a serious complication of diabetes that can lead to vision loss if not diagnosed and treated early. Understanding how this condition is diagnosed is crucial for anyone living with diabetes. Regular eye examinations are essential for early detection and management.
Understanding the Diagnostic Process
The diagnosis of diabetic eye disease typically involves a comprehensive eye examination conducted by an eye care professional. Here are the key components of the diagnostic process:
- Medical History Review: Your eye doctor will start by reviewing your medical history, including your diabetes management and any symptoms you may be experiencing.
- Visual Acuity Test: This test measures how well you can see at various distances. It helps determine if your vision has been affected.
- Dilated Eye Exam: Eye drops are used to dilate your pupils, allowing the doctor to examine the retina and optic nerve for signs of damage.
- Optical Coherence Tomography (OCT): This imaging test provides cross-sectional images of the retina, helping to identify any swelling or fluid buildup.
- Fluorescein Angiography: A special dye is injected into your bloodstream, and photographs are taken of the retina to highlight any abnormal blood vessels.
Recognizing Symptoms
Many individuals with diabetic eye disease may not experience noticeable symptoms in the early stages. However, as the condition progresses, symptoms may include:
- Blurred or distorted vision
- Dark spots or floaters in your vision
- Difficulty seeing at night
- Sudden vision loss
If you notice any of these symptoms, it’s essential to seek medical attention promptly. Early diagnosis can significantly improve treatment outcomes and help preserve your vision. 👁️
Treatment Options Available
Once diagnosed, there are several treatment options available for managing diabetic eye disease. The choice of treatment depends on the severity of the condition and the specific needs of the patient.
Monitoring and Lifestyle Changes
For individuals in the early stages of diabetic eye disease, close monitoring and lifestyle changes may be sufficient. This includes:
- Regular Eye Exams: Frequent check-ups with your eye doctor to monitor any changes in your condition.
- Blood Sugar Control: Maintaining optimal blood sugar levels through diet, exercise, and medication can help slow the progression of the disease.
- Healthy Lifestyle Choices: Quitting smoking, eating a balanced diet, and exercising regularly can significantly impact your overall eye health.
Medical Treatments
For more advanced stages of diabetic eye disease, medical treatments may be necessary. These include:
- Laser Treatment: This procedure, known as photocoagulation, uses laser technology to seal leaking blood vessels and prevent further vision loss.
- Injections: Medications such as anti-VEGF (vascular endothelial growth factor) injections can help reduce swelling and prevent the growth of abnormal blood vessels in the retina.
- Surgery: In severe cases, surgical options like vitrectomy may be required to remove blood and scar tissue from the eye.
Importance of Diabetic Eye Disease Awareness
Raising awareness about diabetic eye disease is crucial, especially during Diabetic Eye Disease Awareness Month. This initiative aims to educate individuals about the importance of regular eye exams and the potential risks associated with diabetes. By spreading the word, we can help more people understand the significance of early detection and treatment. 📅
In conclusion, understanding the diagnosis and treatment options for diabetic eye disease is vital for anyone living with diabetes. Regular eye examinations and proactive management can help preserve vision and improve quality of life. If you have diabetes, make sure to prioritize your eye health! 👓

Preventing Diabetic Eye Disease
Diabetic eye disease is a serious complication that can arise from diabetes, affecting millions of people worldwide. However, the good news is that there are effective strategies to help prevent this condition. By understanding the risk factors and implementing preventive measures, you can significantly reduce your chances of developing diabetic eye disease.
Understanding the Risk Factors
Before diving into prevention strategies, it’s essential to recognize the risk factors associated with diabetic eye disease. These include:
- Duration of Diabetes: The longer you have diabetes, the higher your risk of developing eye complications.
- Blood Sugar Levels: Poorly controlled blood sugar levels can lead to damage in the blood vessels of the retina.
- High Blood Pressure: Hypertension can exacerbate the effects of diabetes on your eyes.
- High Cholesterol: Elevated cholesterol levels can contribute to the progression of diabetic eye disease.
- Smoking: Tobacco use increases the risk of diabetic complications, including eye disease.
Effective Prevention Strategies
Now that you know the risk factors, here are some actionable steps you can take to prevent diabetic eye disease:
- Regular Eye Exams: Schedule comprehensive eye exams at least once a year. Early detection is crucial for preventing severe complications.
- Manage Blood Sugar Levels: Work with your healthcare team to maintain your blood sugar levels within the target range. This may involve medication, diet, and exercise.
- Control Blood Pressure and Cholesterol: Regularly monitor and manage your blood pressure and cholesterol levels through lifestyle changes and medication if necessary.
- Healthy Diet: Incorporate a balanced diet rich in fruits, vegetables, whole grains, and lean proteins. Foods high in antioxidants, such as leafy greens and berries, can be particularly beneficial for eye health.
- Stay Active: Regular physical activity can help control blood sugar levels and improve overall health. Aim for at least 150 minutes of moderate exercise each week.
- Avoid Smoking: If you smoke, seek help to quit. Your eyes and overall health will thank you!
Awareness and Education
Participating in Diabetic Eye Disease Awareness Month can also be a great way to stay informed and spread knowledge about this condition. Engaging in community events and educational programs can empower you and others to take proactive steps in preventing diabetic eye disease.
Living with Diabetic Eye Disease
Receiving a diagnosis of diabetic eye disease can be overwhelming, but understanding how to manage the condition can lead to a better quality of life. With the right approach, you can continue to live a fulfilling life while managing your eye health.
Understanding Your Diagnosis
Diabetic eye disease encompasses several conditions, including diabetic retinopathy, diabetic macular edema, and cataracts. Each of these conditions affects the eyes differently:
- Diabetic Retinopathy: Damage to the blood vessels in the retina, which can lead to vision loss.
- Diabetic Macular Edema: Swelling in the macula, the part of the retina responsible for sharp vision.
- Cataracts: Clouding of the lens of the eye, which can cause blurry vision.
Managing Your Condition
Living with diabetic eye disease requires a proactive approach to management:
- Follow Your Treatment Plan: Adhere to the treatment plan prescribed by your eye care professional. This may include medications, injections, or laser treatments.
- Monitor Your Vision: Keep track of any changes in your vision and report them to your healthcare provider immediately.
- Maintain a Healthy Lifestyle: Continue to follow a healthy diet and exercise routine to manage your diabetes effectively.
- Stay Informed: Educate yourself about diabetic eye disease and stay updated on new treatments and research.
Emotional Support and Resources
Living with a chronic condition can be emotionally challenging. Seek support from family, friends, or support groups. Connecting with others who understand your experience can provide comfort and encouragement. Additionally, consider reaching out to organizations dedicated to diabetes and eye health for resources and information.
By taking charge of your health and staying informed, you can effectively manage diabetic eye disease and maintain your vision for years to come. Remember, you are not alone in this journey! 🌟

Frequently Asked Questions about Diabetic Eye Disease
What is Diabetic Eye Disease?
Diabetic Eye Disease refers to a group of eye conditions that can affect individuals with diabetes, including diabetic retinopathy, diabetic macular edema, and cataracts. These conditions can lead to vision loss if not managed properly.
What are the symptoms of Diabetic Eye Disease?
Common diabetic eye disease symptoms include:
- Blurred or distorted vision
- Dark or empty areas in your vision
- Difficulty seeing at night
- Sudden vision changes
If you experience any of these symptoms, it is crucial to consult an eye care professional promptly. 👁️
How is Diabetic Eye Disease treated?
Treatment options for diabetic eye disease may include:
- Laser therapy to reduce swelling and prevent vision loss
- Injections of medication into the eye to control inflammation
- Surgery in advanced cases to remove blood or scar tissue
Early detection and treatment are vital for preserving vision.
What are the stages of Diabetic Eye Disease?
Diabetic eye disease stages typically progress as follows:
- Non-proliferative diabetic retinopathy (NPDR)
- Proliferative diabetic retinopathy (PDR)
- Diabetic macular edema (DME)
Regular eye exams can help monitor these stages and initiate treatment when necessary.
Is there a specific month dedicated to Diabetic Eye Disease awareness?
Yes, Diabetic Eye Disease Awareness Month is observed in November. This month aims to educate the public about the importance of eye health in individuals with diabetes.
What is the ICD-10 code for Diabetic Eye Disease?
The ICD-10 code for diabetic eye disease varies depending on the specific condition, but common codes include E11.359 for diabetic retinopathy and E11.359 for diabetic macular edema. Always consult a healthcare provider for accurate coding.
Are there different types of Diabetic Eye Diseases?
Yes, there are several types of diabetic eye diseases, including:
- Diabetic retinopathy
- Diabetic macular edema
- Diabetic cataracts
Each type has its own risk factors and treatment options.
Where can I find images of Diabetic Eye Disease?
Images of diabetic eye disease can be found in medical literature, online health resources, and educational websites dedicated to diabetes care. These images can help in understanding the condition better.
How can I raise awareness about Diabetic Eye Disease?
You can raise awareness by:
- Sharing information on social media
- Participating in local health events
- Encouraging friends and family to get regular eye exams
Every effort counts in spreading awareness! 🌍




