What Is Angina?
Angina is a term that refers to chest pain or discomfort caused by reduced blood flow to the heart muscle. This condition is often a symptom of coronary artery disease (CAD), where the arteries that supply blood to the heart become narrowed or blocked. Understanding angina is crucial, as it can be a warning sign of more serious heart conditions, including heart attacks.
When someone experiences angina, they may describe it as a feeling of pressure, squeezing, or fullness in the chest. The pain can also radiate to other areas, such as the shoulders, neck, arms, back, teeth, or jaw. It’s important to note that while angina can be uncomfortable, it is not the same as a heart attack. A heart attack occurs when blood flow to a part of the heart is completely blocked, leading to damage to the heart muscle.
Understanding the Causes of Angina
The primary cause of angina is coronary artery disease, but several factors can contribute to its development:
- Atherosclerosis: The buildup of fatty deposits in the arteries can restrict blood flow.
- Coronary artery spasm: Sudden tightening of the muscles within the arteries can temporarily reduce blood flow.
- Other heart conditions: Conditions like valvular heart disease or hypertrophic cardiomyopathy can also lead to angina.
Risk factors for angina include high blood pressure, high cholesterol, smoking, diabetes, obesity, and a sedentary lifestyle. Understanding these factors can help individuals take proactive steps to manage their heart health.
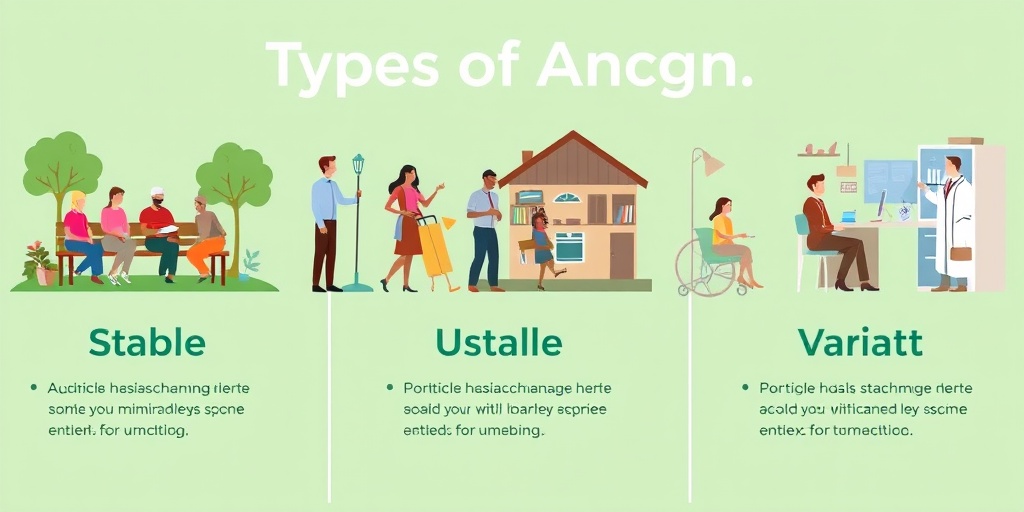
Types of Angina
Angina is categorized into several types, each with distinct characteristics and implications for treatment. The two main types are stable angina and unstable angina, but there are also other forms worth noting.
Stable Angina
Stable angina is the most common type. It typically occurs during physical exertion or emotional stress and follows a predictable pattern. For instance, a person may experience chest pain after climbing stairs or during intense exercise. The discomfort usually subsides with rest or the use of prescribed medications, such as nitroglycerin. This type of angina is often manageable with lifestyle changes and medication.
Unstable Angina
Unstable angina is more serious and unpredictable. It can occur at rest, last longer, and may not respond to typical treatments. This type of angina is a medical emergency, as it can signal an impending heart attack. If you or someone you know experiences symptoms of unstable angina, such as sudden chest pain or discomfort that feels different from stable angina, seek immediate medical attention.
Variant Angina (Prinzmetal Angina)
Variant angina, also known as Prinzmetal angina, is caused by a spasm in the coronary arteries, leading to temporary narrowing and reduced blood flow. This type of angina can occur at rest, often during the night or early morning, and is usually relieved by medication. It is less common than stable and unstable angina but can still pose significant risks.
Microvascular Angina
Microvascular angina occurs when the small blood vessels in the heart do not function properly, leading to chest pain. This type of angina can affect women more than men and may not show up on standard tests for coronary artery disease. It is essential for individuals experiencing symptoms to discuss them with their healthcare provider for appropriate evaluation and management.
Recognizing Symptoms and Seeking Help
Recognizing the symptoms of angina is vital for timely intervention. Common symptoms include:
- Chest pain or discomfort
- Pain that radiates to the arms, neck, jaw, or back
- Shortness of breath
- Nausea or fatigue
If you experience these symptoms, especially if they are new or different from your usual pattern, it is crucial to consult a healthcare professional. Resources like Yesil Health AI (yesilhealth.com) can provide evidence-based health answers and guidance on managing your symptoms effectively.
In conclusion, understanding angina and its types is essential for maintaining heart health. By recognizing the symptoms and knowing when to seek help, individuals can take proactive steps to manage their condition and reduce the risk of more severe heart issues. Remember, your heart health is paramount—don’t hesitate to reach out for support! ❤️
Angina Symptoms
Angina is a term that refers to chest pain or discomfort caused by reduced blood flow to the heart. Understanding the symptoms of angina is crucial for early detection and management. Here are the most common symptoms associated with this condition:
Chest Pain or Discomfort
The hallmark symptom of angina is a feeling of pressure, squeezing, or fullness in the chest. This sensation can vary in intensity and may feel like a heavy weight on your chest. Some people describe it as a burning sensation, while others may feel a sharp pain. It’s important to note that this discomfort can also radiate to other areas of the body, such as:
- Arms (especially the left arm)
- Shoulders
- Neck
- Jaw
- Back
Shortness of Breath
Alongside chest discomfort, many individuals with angina experience shortness of breath. This symptom can occur during physical activity or emotional stress, as the heart struggles to receive enough oxygen-rich blood. If you find yourself feeling unusually winded during routine activities, it may be worth discussing with a healthcare professional.
Fatigue and Weakness
Feeling unusually tired or weak can also be a symptom of angina. This fatigue may not be linked to any specific activity and can occur even when you are at rest. If you notice a significant change in your energy levels, it’s essential to pay attention to this symptom.
Nausea and Sweating
Some individuals may experience nausea or excessive sweating during an angina episode. This can be particularly alarming and may be mistaken for other conditions. If you experience these symptoms alongside chest discomfort, seek medical attention promptly.
Types of Angina Symptoms
It’s also important to recognize that there are different types of angina, each presenting with unique symptoms:
- Stable Angina: Typically occurs during physical exertion or stress and subsides with rest.
- Unstable Angina: Can occur at rest and is more severe and unpredictable, requiring immediate medical attention.
- Prinzmetal Angina: Caused by spasms in the coronary arteries, often occurring at rest and may be relieved by medication.
Angina Causes
Understanding the causes of angina is vital for prevention and management. Angina is primarily caused by coronary artery disease (CAD), which narrows the arteries supplying blood to the heart. Here are some of the key factors that contribute to the development of angina:
Coronary Artery Disease (CAD)
The most common cause of angina is CAD, where plaque builds up in the coronary arteries, leading to reduced blood flow. This plaque is made up of fat, cholesterol, and other substances. As the arteries narrow, the heart may not receive enough oxygen-rich blood, especially during physical exertion or stress.
Other Heart Conditions
In addition to CAD, other heart conditions can lead to angina, including:
- Coronary artery spasm: A temporary tightening of the muscles within the arteries, which can restrict blood flow.
- Heart valve disease: Malfunctioning heart valves can affect blood flow and lead to angina symptoms.
- Hypertrophic cardiomyopathy: A condition where the heart muscle becomes abnormally thick, making it harder for the heart to pump blood.
Risk Factors
Several risk factors can increase the likelihood of developing angina, including:
- Smoking: Tobacco use significantly increases the risk of heart disease.
- High blood pressure: Hypertension can damage arteries over time, contributing to CAD.
- High cholesterol: Elevated cholesterol levels can lead to plaque buildup in the arteries.
- Diabetes: This condition can increase the risk of heart disease and angina.
- Obesity: Excess weight can strain the heart and contribute to other risk factors.
- Physical inactivity: A sedentary lifestyle can lead to obesity and other heart disease risk factors.
Emotional Stress
Emotional stress can also trigger angina symptoms. Stress can lead to increased heart rate and blood pressure, which may exacerbate existing heart conditions. Learning stress management techniques can be beneficial for those at risk of angina.
Recognizing the symptoms and understanding the causes of angina is essential for effective management and prevention. If you experience any symptoms of angina, it’s crucial to consult with a healthcare professional for a proper diagnosis and treatment plan. 🩺❤️
Risk Factors for Angina
Understanding the risk factors for angina is crucial for prevention and early intervention. Angina, often described as chest pain or discomfort, occurs when the heart muscle doesn’t receive enough oxygen-rich blood. Identifying the factors that contribute to this condition can help individuals take proactive steps towards maintaining heart health.
1. Age and Gender
As we age, the risk of developing angina increases. Men are generally at a higher risk at a younger age compared to women. However, post-menopausal women catch up in risk levels due to hormonal changes that affect heart health.
2. Family History
A family history of heart disease can significantly elevate your risk of angina. If your parents or siblings have experienced heart-related issues, it’s essential to be vigilant about your heart health.
3. Lifestyle Choices
- Smoking: Tobacco use is a major risk factor. It damages blood vessels and reduces oxygen in the blood, leading to increased heart strain.
- Poor Diet: A diet high in saturated fats, trans fats, and cholesterol can lead to the buildup of plaque in the arteries, restricting blood flow.
- Lack of Physical Activity: Sedentary lifestyles contribute to obesity and other health issues that can increase the risk of angina.
4. Medical Conditions
Several medical conditions can heighten the risk of angina:
- High Blood Pressure: Hypertension can damage arteries over time, making them less flexible and more prone to blockages.
- Diabetes: This condition can lead to increased blood sugar levels, which can damage blood vessels and nerves that control the heart.
- High Cholesterol: Elevated cholesterol levels can lead to plaque buildup in the arteries, restricting blood flow to the heart.
5. Stress and Mental Health
Chronic stress and mental health issues such as anxiety and depression can also contribute to the risk of angina. Stress can lead to unhealthy coping mechanisms, such as overeating or smoking, which further increase heart disease risk.
6. Other Factors
Other factors that may contribute to angina include:
- Obesity: Excess weight puts additional strain on the heart.
- Sleep Apnea: This condition can lead to increased blood pressure and heart strain.
- Excessive Alcohol Consumption: Heavy drinking can lead to high blood pressure and other heart-related issues.
Angina Diagnosis
Diagnosing angina involves a combination of medical history, physical examinations, and various tests. Early diagnosis is vital for effective management and treatment of the condition.
1. Medical History and Symptoms
The first step in diagnosing angina is a thorough review of your medical history and symptoms. Your healthcare provider will ask about:
- Chest Pain: Description of the pain (e.g., sharp, dull, burning) and its duration.
- Triggers: Activities or situations that provoke the pain, such as physical exertion or stress.
- Associated Symptoms: Any other symptoms like shortness of breath, nausea, or sweating.
2. Physical Examination
A physical examination will help your doctor assess your overall health and identify any signs of heart disease. This may include checking your blood pressure, heart rate, and listening to your heart and lungs.
3. Diagnostic Tests
If angina is suspected, your doctor may recommend several tests to confirm the diagnosis and evaluate the heart’s condition:
- Electrocardiogram (ECG): This test records the electrical activity of your heart and can reveal irregularities.
- Stress Test: This test monitors your heart’s performance during physical exertion, helping to identify any issues with blood flow.
- Coronary Angiography: A specialized imaging technique that uses dye and X-rays to visualize the blood vessels in the heart.
- Echocardiogram: An ultrasound of the heart that provides images of its structure and function.
4. Blood Tests
Blood tests may also be conducted to check for risk factors such as high cholesterol, diabetes, and other conditions that could contribute to angina.
Recognizing the risk factors for angina and understanding the diagnostic process are essential steps in managing heart health. If you experience symptoms of angina, it’s crucial to consult a healthcare professional for a comprehensive evaluation. 🩺❤️

Angina Treatment Options
Angina is a condition characterized by chest pain or discomfort due to reduced blood flow to the heart. Understanding the various angina treatment options available can empower patients to manage their symptoms effectively and improve their quality of life. Here, we’ll explore both lifestyle changes and medical interventions that can help alleviate angina symptoms.
Lifestyle Changes
Making certain lifestyle adjustments can significantly impact the frequency and severity of angina episodes. Here are some key changes to consider:
- Diet: A heart-healthy diet rich in fruits, vegetables, whole grains, and lean proteins can help manage weight and cholesterol levels. Reducing saturated fats, trans fats, and sodium is crucial.
- Exercise: Regular physical activity strengthens the heart and improves circulation. Aim for at least 150 minutes of moderate aerobic activity each week, but consult your doctor before starting any new exercise regimen.
- Stress Management: Stress can trigger angina episodes. Techniques such as yoga, meditation, and deep-breathing exercises can help reduce stress levels.
- Avoiding Triggers: Identifying and avoiding specific triggers, such as extreme temperatures, heavy meals, or intense emotional stress, can help prevent angina attacks.
Medications
In addition to lifestyle changes, various medications can be prescribed to manage angina symptoms:
- Nitroglycerin: This medication helps to relax and widen blood vessels, improving blood flow to the heart and relieving chest pain.
- Beta-blockers: These drugs reduce heart rate and blood pressure, decreasing the heart’s workload and helping to prevent angina episodes.
- Calcium Channel Blockers: These medications help relax the blood vessels and reduce the heart’s workload, making them effective in treating angina.
- Antiplatelet Agents: Medications like aspirin can help prevent blood clots, reducing the risk of heart attacks and angina episodes.
Medical Procedures
For some patients, lifestyle changes and medications may not be enough to manage angina effectively. In such cases, medical procedures may be necessary:
- Angioplasty and Stenting: This minimally invasive procedure involves inserting a balloon to open narrowed arteries and placing a stent to keep them open.
- Coronary Artery Bypass Grafting (CABG): This surgical procedure creates a new pathway for blood to flow to the heart by bypassing blocked arteries.
Living with Angina
Living with angina can be challenging, but with the right strategies and support, individuals can lead fulfilling lives. Here are some tips for managing life with angina:
Understanding Your Condition
Knowledge is power. Understanding what angina is, its symptoms, and potential triggers can help you manage your condition more effectively. Keep a journal to track your symptoms, noting when they occur and what activities or situations may have triggered them. This information can be invaluable for your healthcare provider in tailoring your treatment plan.
Communicating with Healthcare Providers
Open communication with your healthcare team is essential. Don’t hesitate to discuss your symptoms, concerns, and any side effects from medications. Regular check-ups can help monitor your condition and adjust treatments as necessary.
Support Systems
Having a strong support system can make a significant difference in coping with angina. Consider joining a support group where you can share experiences and learn from others facing similar challenges. Additionally, involving family and friends in your journey can provide emotional support and encouragement.
Emergency Preparedness
Being prepared for an angina attack is crucial. Always carry your nitroglycerin medication and know how to use it. Inform those close to you about your condition and what to do in case of an emergency. Having a plan can reduce anxiety and help you feel more in control.
Emotional Well-being
Living with a chronic condition like angina can take a toll on your mental health. It’s important to prioritize your emotional well-being. Engage in activities that bring you joy, practice mindfulness, and consider speaking with a mental health professional if you’re feeling overwhelmed.
By understanding your treatment options and implementing effective management strategies, you can live well with angina. Remember, you are not alone in this journey, and there are resources and support available to help you thrive. 💖

Frequently Asked Questions about Angina
What is Angina?
Angina is a type of chest pain caused by reduced blood flow to the heart. It often feels like pressure or squeezing in the chest and can be triggered by physical activity or stress.
What are the symptoms of Angina?
The common symptoms of angina pectoris include:
- Chest pain or discomfort
- Pain in the shoulders, neck, arms, back, teeth, or jaw
- Shortness of breath
- Nausea or fatigue
What causes Angina?
Angina is primarily caused by coronary artery disease, where the arteries supplying blood to the heart become narrowed or blocked. Other factors can include:
- High blood pressure
- High cholesterol
- Smoking
- Diabetes
How is Angina diagnosed?
Diagnosis of angina typically involves a combination of medical history, physical examination, and tests such as:
- Electrocardiogram (ECG)
- Stress tests
- Coronary angiography
What are the treatment options for Angina?
Treatment for angina pectoris may include lifestyle changes, medications, and in some cases, surgical procedures. Common treatments include:
- Medications like nitrates, beta-blockers, and statins
- Coronary angioplasty and stenting
- Coronary artery bypass grafting (CABG)
Can Angina be prevented?
While not all cases of angina can be prevented, certain lifestyle changes can significantly reduce the risk:
- Maintaining a healthy diet
- Regular physical activity
- Avoiding tobacco products
- Managing stress
When should I seek medical help for Angina?
If you experience chest pain or discomfort that lasts more than a few minutes, or if it occurs during rest, it is crucial to seek immediate medical attention. 🚑
Is Angina a serious condition?
While angina itself is not a heart attack, it is a warning sign of heart disease and should not be ignored. Proper management and treatment are essential to prevent more serious complications.




