What Is Pulmonary Hypertension?
Pulmonary hypertension (PH) is a serious condition characterized by elevated blood pressure in the pulmonary arteries, which are the vessels that carry blood from the heart to the lungs. This increase in pressure can lead to various complications, including heart failure, and significantly impacts a person’s quality of life. Understanding pulmonary hypertension is crucial for early diagnosis and effective management.
Understanding the Basics
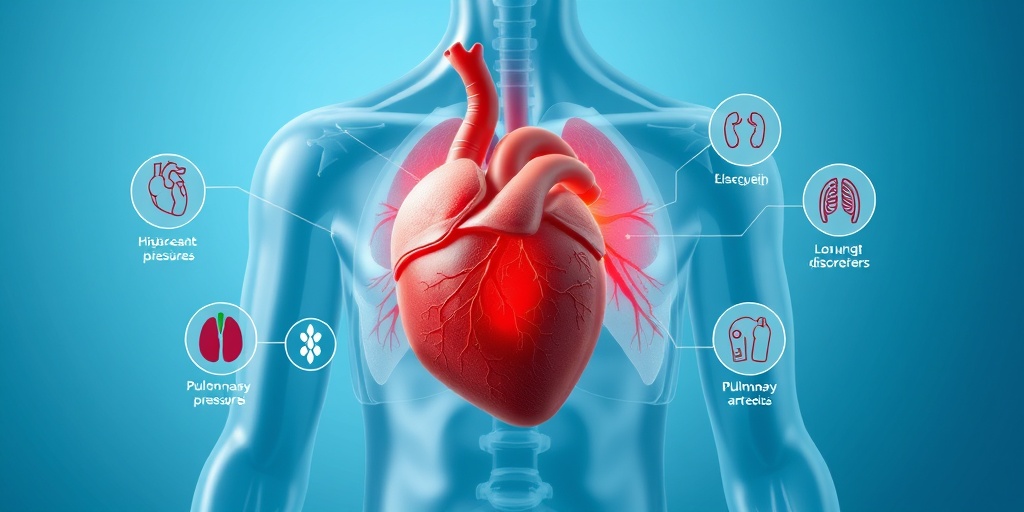
The pulmonary arteries are responsible for transporting oxygen-poor blood from the right side of the heart to the lungs, where it picks up oxygen. In a healthy individual, the pressure in these arteries is relatively low. However, when someone has pulmonary hypertension, the pressure rises, making it difficult for the heart to pump blood effectively. This can lead to symptoms such as:
- Shortness of breath, especially during physical activity
- Fatigue
- Chest pain
- Swelling in the ankles, legs, or abdomen
- Heart palpitations
These symptoms can often be mistaken for other conditions, which is why awareness and understanding of pulmonary hypertension are vital.
Types of Pulmonary Hypertension
Pulmonary hypertension is classified into five groups based on its causes:
- Group 1: Pulmonary arterial hypertension (PAH)
- Group 2: Pulmonary hypertension secondary to left heart disease
- Group 3: Pulmonary hypertension secondary to lung diseases
- Group 4: Pulmonary hypertension due to chronic blood clots
- Group 5: Pulmonary hypertension with unclear multifactorial mechanisms
Among these, secondary pulmonary hypertension is particularly significant, as it arises from other underlying health conditions.
Secondary Pulmonary Hypertension Explained
Secondary pulmonary hypertension refers to elevated blood pressure in the pulmonary arteries that results from another medical condition. Unlike primary pulmonary hypertension, which occurs without any identifiable cause, secondary pulmonary hypertension is often linked to various diseases and health issues.
Common Causes of Secondary Pulmonary Hypertension
Several conditions can lead to secondary pulmonary hypertension, including:
- Chronic Obstructive Pulmonary Disease (COPD): This lung disease can cause changes in the pulmonary arteries, leading to increased pressure.
- Heart Failure: When the heart is unable to pump effectively, it can cause blood to back up in the pulmonary arteries.
- Obstructive Sleep Apnea (OSA): This condition can lead to intermittent low oxygen levels, contributing to pulmonary hypertension.
- Left Heart Disease: Conditions affecting the left side of the heart can increase pressure in the pulmonary circulation.
- Scleroderma: This autoimmune disease can cause changes in blood vessels, leading to pulmonary hypertension.
- Pulmonary Embolism: Blood clots in the lungs can obstruct blood flow and increase pressure.
- Congenital Heart Disease: Structural heart defects present at birth can lead to abnormal blood flow and increased pressure in the pulmonary arteries.
Each of these conditions can contribute to the development of secondary pulmonary hypertension, making it essential for healthcare providers to identify and treat the underlying cause.
Diagnosis and Treatment
Diagnosing secondary pulmonary hypertension typically involves a combination of medical history, physical examinations, and diagnostic tests such as echocardiograms, chest X-rays, and right heart catheterization. Once diagnosed, treatment focuses on managing the underlying condition and may include:
- Medications to lower blood pressure in the pulmonary arteries
- Oxygen therapy for those with low oxygen levels
- Lifestyle changes, including diet and exercise
- Surgical options in severe cases
For more detailed information and personalized advice, consider visiting Yesil Health AI, a valuable resource for evidence-based health answers.
In conclusion, understanding pulmonary hypertension, secondary is crucial for effective management and improving quality of life. If you or someone you know is experiencing symptoms, it’s important to seek medical advice promptly. Early diagnosis and treatment can make a significant difference! 🌟
Symptoms of Pulmonary Hypertension
Pulmonary hypertension (PH) is a serious condition characterized by high blood pressure in the pulmonary arteries, which can lead to significant health complications. Recognizing the symptoms early is crucial for effective management and treatment. Here are some common symptoms associated with pulmonary hypertension, secondary:
1. Shortness of Breath
One of the most prevalent symptoms of pulmonary hypertension is shortness of breath, especially during physical activities. Patients may find themselves easily fatigued or unable to perform tasks they once managed with ease. This symptom can worsen over time, making daily activities increasingly challenging.
2. Fatigue
Chronic fatigue is another common complaint among individuals with pulmonary hypertension. This overwhelming sense of tiredness can be debilitating and is often exacerbated by the body’s struggle to deliver adequate oxygen to tissues and organs.
3. Chest Pain
Some patients may experience chest pain or discomfort, which can be mistaken for other conditions. This pain can vary in intensity and may occur during physical exertion or even at rest.
4. Swelling in the Legs and Ankles
Fluid retention is a common issue in pulmonary hypertension, leading to swelling in the legs and ankles. This occurs due to increased pressure in the blood vessels, causing fluid to leak into surrounding tissues.
5. Palpitations
Individuals may also notice palpitations or an irregular heartbeat. This symptom can be alarming and may indicate that the heart is working harder to pump blood through narrowed arteries.
6. Dizziness or Fainting
In more severe cases, patients might experience dizziness or fainting spells, particularly during physical exertion. This occurs due to insufficient blood flow to the brain, highlighting the importance of seeking medical attention if these symptoms arise.
7. Cyanosis
Cyanosis, or a bluish tint to the lips and skin, can occur in advanced stages of pulmonary hypertension. This symptom indicates a lack of oxygen in the blood and requires immediate medical evaluation.
Causes of Secondary Pulmonary Hypertension
Understanding the causes of secondary pulmonary hypertension is essential for effective treatment and management. Unlike primary pulmonary hypertension, which has no identifiable cause, secondary pulmonary hypertension arises from underlying health conditions. Here are some common causes:
1. Chronic Obstructive Pulmonary Disease (COPD)
COPD is one of the leading causes of secondary pulmonary hypertension. The damage to the lungs and airways from this chronic condition can lead to increased pressure in the pulmonary arteries, making it difficult for blood to flow efficiently.
2. Heart Failure
Heart failure can also contribute to the development of secondary pulmonary hypertension. When the heart is unable to pump blood effectively, it can cause a backlog of blood in the pulmonary circulation, leading to elevated pressures.
3. Obstructive Sleep Apnea (OSA)
Obstructive sleep apnea is another significant risk factor. The repeated interruptions in breathing during sleep can lead to increased pressure in the pulmonary arteries, contributing to the development of pulmonary hypertension.
4. Left Heart Disease
Conditions affecting the left side of the heart, such as mitral valve disease or left ventricular dysfunction, can lead to secondary pulmonary hypertension. The impaired function of the heart can cause increased pressure in the pulmonary circulation.
5. Scleroderma
Scleroderma, an autoimmune disease that affects connective tissues, can also lead to pulmonary hypertension. The disease can cause changes in the blood vessels and lung tissue, resulting in increased pressure in the pulmonary arteries.
6. Pulmonary Embolism
A pulmonary embolism, which occurs when a blood clot blocks a pulmonary artery, can lead to secondary pulmonary hypertension. This blockage can cause significant strain on the heart and lungs, resulting in elevated pressures.
7. Congenital Heart Disease
Individuals with congenital heart defects may also develop secondary pulmonary hypertension. Abnormal blood flow patterns can lead to increased pressure in the pulmonary arteries over time.
Recognizing the symptoms and understanding the causes of pulmonary hypertension, secondary is vital for timely diagnosis and treatment. If you or someone you know is experiencing these symptoms, it is essential to consult a healthcare professional for further evaluation and management. 🩺
Risk Factors for Secondary Pulmonary Hypertension
Pulmonary hypertension (PH) is a serious condition characterized by elevated blood pressure in the pulmonary arteries, which can lead to heart failure and other complications. While there are various forms of pulmonary hypertension, secondary pulmonary hypertension arises as a result of other underlying health issues. Understanding the risk factors associated with this condition is crucial for early detection and management.
Common Risk Factors
Several factors can increase the likelihood of developing secondary pulmonary hypertension. Here are some of the most significant:
- Chronic Lung Diseases: Conditions such as chronic obstructive pulmonary disease (COPD) and interstitial lung disease can lead to secondary pulmonary hypertension. These diseases damage lung tissue and impair oxygen exchange, increasing pressure in the pulmonary arteries.
- Heart Conditions: Heart failure, congenital heart defects, and left heart disease can contribute to elevated pulmonary artery pressure. When the left side of the heart is unable to pump blood effectively, it can back up into the lungs, causing increased pressure.
- Obstructive Sleep Apnea (OSA): OSA is a sleep disorder that causes breathing interruptions during sleep. This condition can lead to low oxygen levels, which may result in pulmonary hypertension over time.
- Scleroderma: This autoimmune disease affects connective tissues and can cause changes in the blood vessels, leading to pulmonary hypertension. Patients with scleroderma are at a higher risk for developing this condition.
- Chronic Thromboembolic Disease: Recurrent blood clots in the lungs can lead to chronic thromboembolic pulmonary hypertension (CTEPH). This condition occurs when clots obstruct blood flow, causing increased pressure in the pulmonary arteries.
- Congenital Heart Disease: Individuals born with heart defects may experience secondary pulmonary hypertension due to abnormal blood flow patterns that increase pressure in the pulmonary arteries.
Other Contributing Factors
In addition to the primary risk factors, several other elements can contribute to the development of secondary pulmonary hypertension:
- Age: The risk of developing pulmonary hypertension increases with age, particularly in individuals over 65.
- Obesity: Excess weight can strain the heart and lungs, potentially leading to pulmonary hypertension.
- Family History: A family history of pulmonary hypertension or related conditions may increase an individual’s risk.
- Exposure to Certain Drugs: Some medications, particularly those used for weight loss or certain recreational drugs, can increase the risk of pulmonary hypertension.
Diagnosis of Pulmonary Hypertension
Diagnosing pulmonary hypertension, especially secondary pulmonary hypertension, can be challenging due to its nonspecific symptoms. However, early diagnosis is essential for effective management and treatment. Here’s how healthcare providers typically approach the diagnosis.
Initial Evaluation
The diagnostic process often begins with a thorough medical history and physical examination. During this evaluation, healthcare providers will:
- Assess symptoms such as shortness of breath, fatigue, chest pain, and palpitations.
- Inquire about any underlying health conditions, family history, and lifestyle factors.
Diagnostic Tests
If pulmonary hypertension is suspected, several tests may be conducted to confirm the diagnosis and determine its cause:
- Echocardiogram: This ultrasound test provides images of the heart and can estimate the pressure in the pulmonary arteries. It is often the first test performed when PH is suspected.
- Chest X-ray: A chest X-ray can help identify any lung or heart abnormalities that may contribute to pulmonary hypertension.
- CT Pulmonary Angiography: This imaging test provides detailed pictures of the blood vessels in the lungs and can help detect blood clots or other abnormalities.
- Right Heart Catheterization: This invasive procedure measures the pressure in the pulmonary arteries directly and is considered the gold standard for diagnosing pulmonary hypertension.
- Blood Tests: Blood tests may be conducted to check for underlying conditions such as scleroderma or other autoimmune diseases.
Monitoring and Follow-Up
Once diagnosed, ongoing monitoring is crucial. Regular follow-up appointments and tests can help track the progression of the disease and the effectiveness of treatment. Patients may also be referred to specialists, such as cardiologists or pulmonologists, for comprehensive care.
Understanding the risk factors and diagnostic process for secondary pulmonary hypertension is vital for timely intervention and improved outcomes. If you or someone you know is experiencing symptoms, it’s essential to seek medical advice promptly. 🩺
Treatment Options for Secondary Pulmonary Hypertension
Pulmonary hypertension (PH) is a serious condition characterized by elevated blood pressure in the pulmonary arteries, which can lead to significant health complications. When this condition is classified as secondary pulmonary hypertension, it means that it is a result of another underlying health issue. Understanding the treatment options available is crucial for managing this condition effectively.
Understanding the Causes
Before diving into treatment options, it’s essential to recognize the common causes of secondary pulmonary hypertension. These may include:
- Chronic Obstructive Pulmonary Disease (COPD)
- Heart Failure
- Obstructive Sleep Apnea (OSA)
- Left Heart Disease
- Scleroderma
- Pulmonary Embolism
- Congenital Heart Disease
- Chronic Lung Disease
Identifying the underlying cause is vital, as it will guide the treatment approach. For instance, if the pulmonary hypertension is secondary to COPD, managing the lung disease will be a priority.
Medications
Medications play a significant role in managing secondary pulmonary hypertension. Depending on the underlying cause, doctors may prescribe:
- Vasodilators: These medications help relax and widen blood vessels, reducing blood pressure in the lungs. Examples include epoprostenol and treprostinil.
- Endothelin Receptor Antagonists: These drugs block the effects of endothelin, a substance that constricts blood vessels. Bosentan is a common choice.
- Phosphodiesterase-5 Inhibitors: Medications like sildenafil and tadalafil can help improve blood flow in the lungs.
- Diuretics: If heart failure is a contributing factor, diuretics may be prescribed to reduce fluid buildup.
It’s important to work closely with a healthcare provider to determine the most appropriate medication regimen based on individual health needs.
Oxygen Therapy
For patients with low oxygen levels due to pulmonary hypertension, oxygen therapy can be beneficial. This treatment involves using supplemental oxygen to improve oxygen saturation in the blood, which can alleviate symptoms and enhance overall quality of life.
Lifestyle Changes
In addition to medical treatments, certain lifestyle changes can significantly impact the management of secondary pulmonary hypertension:
- Regular Exercise: Engaging in light to moderate exercise can improve cardiovascular health and overall well-being. Always consult a doctor before starting any exercise program.
- Healthy Diet: A balanced diet rich in fruits, vegetables, whole grains, and lean proteins can support heart health.
- Avoiding High Altitudes: High altitudes can exacerbate symptoms, so it’s advisable to avoid these environments.
- Smoking Cessation: Quitting smoking is crucial for lung health and can help manage pulmonary hypertension.
Surgical Options
In some cases, surgical interventions may be necessary. Procedures such as atrial septostomy or lung transplantation may be considered for patients with severe pulmonary hypertension that does not respond to other treatments. These options are typically reserved for advanced cases and require thorough evaluation by a specialist.
Living with Pulmonary Hypertension
Living with secondary pulmonary hypertension can be challenging, but with the right support and management strategies, individuals can lead fulfilling lives. Here are some key aspects to consider:
Emotional Support
Dealing with a chronic condition can take a toll on mental health. It’s essential to seek emotional support from friends, family, or support groups. Connecting with others who understand the challenges of pulmonary hypertension can provide comfort and encouragement. 💖
Regular Monitoring
Regular check-ups with a healthcare provider are crucial for monitoring the condition and adjusting treatment plans as necessary. Keeping track of symptoms and any changes in health can help in making informed decisions about care.
Education and Awareness
Educating oneself about pulmonary hypertension is empowering. Understanding the condition, its causes, and treatment options can help patients advocate for their health. Resources such as the Pulmonary Hypertension Association offer valuable information and support.
Healthy Lifestyle Choices
Incorporating healthy habits into daily life can make a significant difference. This includes:
- Staying Hydrated: Proper hydration supports overall health.
- Managing Stress: Techniques such as meditation, yoga, or deep-breathing exercises can help manage stress levels.
- Following Treatment Plans: Adhering to prescribed medications and treatment regimens is vital for managing symptoms effectively.
By taking proactive steps and working closely with healthcare providers, individuals with secondary pulmonary hypertension can navigate their condition with resilience and hope. 🌈

Frequently Asked Questions about Pulmonary Hypertension, Secondary
What is Pulmonary Hypertension, Secondary?
Pulmonary Hypertension, Secondary refers to high blood pressure in the lungs that is caused by another underlying condition. Unlike primary pulmonary hypertension, which occurs without a known cause, secondary pulmonary hypertension is linked to various health issues such as heart disease, lung disease, or other systemic conditions.
What are the common causes of Secondary Pulmonary Hypertension?
- Chronic Obstructive Pulmonary Disease (COPD): This lung condition can lead to increased pressure in the pulmonary arteries.
- Heart Failure: When the heart is unable to pump effectively, it can cause blood to back up in the lungs.
- Obstructive Sleep Apnea (OSA): This sleep disorder can contribute to pulmonary hypertension due to intermittent low oxygen levels.
- Left Heart Disease: Conditions affecting the left side of the heart can lead to increased pressure in the pulmonary circulation.
- Scleroderma: This autoimmune disease can cause changes in the blood vessels and lead to pulmonary hypertension.
- Pulmonary Embolism: Blood clots in the lungs can cause sudden increases in pulmonary artery pressure.
- Congenital Heart Disease: Structural heart defects present at birth can lead to secondary pulmonary hypertension.
- Chronic Lung Disease: Various chronic lung conditions can contribute to the development of pulmonary hypertension.
How is Secondary Pulmonary Hypertension diagnosed?
Diagnosis typically involves a combination of medical history review, physical examination, and diagnostic tests such as:
- Echocardiogram: This ultrasound test helps assess heart function and blood flow.
- Right Heart Catheterization: This procedure measures the pressure in the pulmonary arteries directly.
- Pulmonary Function Tests: These tests evaluate lung function and capacity.
- Chest X-ray or CT Scan: Imaging tests can help identify underlying lung or heart conditions.
What are the treatment options for Secondary Pulmonary Hypertension?
Treatment for secondary pulmonary hypertension focuses on managing the underlying condition and may include:
- Medications: Various drugs can help lower blood pressure in the lungs.
- Oxygen Therapy: Supplemental oxygen can improve oxygen levels and reduce strain on the heart.
- Lifestyle Changes: Diet, exercise, and avoiding smoking can help manage symptoms.
- Surgery: In some cases, surgical interventions may be necessary to correct underlying issues.
Can Secondary Pulmonary Hypertension be prevented?
While not all cases of secondary pulmonary hypertension can be prevented, managing risk factors such as heart disease, lung disease, and lifestyle choices can help reduce the likelihood of developing this condition. Regular check-ups and early intervention for underlying health issues are crucial.
What is the prognosis for individuals with Secondary Pulmonary Hypertension?
The prognosis for individuals with secondary pulmonary hypertension varies depending on the underlying cause and the effectiveness of treatment. Early diagnosis and management can significantly improve outcomes and quality of life.
When should I see a doctor?
If you experience symptoms such as shortness of breath, fatigue, chest pain, or swelling in the legs, it is important to consult a healthcare professional. Early evaluation and intervention can lead to better management of pulmonary hypertension.