What Is Tendinopathy?
Tendinopathy is a term used to describe a range of conditions that affect the tendons, which are the fibrous tissues connecting muscles to bones. This condition often arises due to overuse, repetitive strain, or injury, leading to pain and dysfunction in the affected area. Unlike tendonitis, which typically involves inflammation, tendinopathy refers to a more chronic condition where the tendon undergoes degenerative changes.
The most common sites for tendinopathy include the shoulder, hip, knee, and elbow. For instance, tendinopathy of the supraspinatus tendon is a prevalent issue among athletes and individuals who perform repetitive overhead activities. Understanding the underlying mechanisms of tendinopathy is crucial for effective treatment and prevention.
Types of Tendinopathy
Tendinopathy can be categorized into two main types:
- Tendinosis: This refers to the degenerative changes in the tendon without inflammation. It often results from chronic overuse and can lead to a weakened tendon structure.
- Tendinitis: This is characterized by inflammation of the tendon, usually due to acute injury or overuse. However, it is important to note that many cases of tendinopathy are more accurately classified as tendinosis.
Causes of Tendinopathy
The primary causes of tendinopathy include:
- Repetitive Motion: Engaging in repetitive activities, such as running, swimming, or playing tennis, can lead to micro-tears in the tendon.
- Age: As we age, tendons lose their elasticity and become more susceptible to injury.
- Improper Technique: Poor biomechanics during physical activities can place undue stress on tendons.
- Underlying Health Conditions: Conditions like diabetes or rheumatoid arthritis can increase the risk of developing tendinopathy.
Tendinopathy Symptoms
Recognizing the symptoms of tendinopathy is essential for early intervention and effective management. Common symptoms include:
- Pain: A dull ache or sharp pain in the affected area, especially during movement or activity.
- Stiffness: Reduced range of motion and stiffness, particularly after periods of inactivity.
- Swelling: Mild swelling around the tendon may occur, although it is not always present.
- Weakness: A noticeable decrease in strength in the affected limb or joint.
Specific Symptoms by Location
The symptoms of tendinopathy can vary depending on the location of the affected tendon:
- Tendinopathy Shoulder: Pain may radiate down the arm, and overhead movements can be particularly painful.
- Tendinopathy Hip: Pain is often felt in the outer hip and may worsen with activities like climbing stairs or sitting for long periods.
- Tendinopathy Knee: Pain is typically felt around the kneecap and may be aggravated by activities such as running or squatting.
If you experience persistent pain or discomfort in any of these areas, it is crucial to consult a healthcare professional for a proper diagnosis and treatment plan. Resources like Yesil Health AI (yesilhealth.com) can provide evidence-based answers to your health questions and guide you in understanding your condition better.
In conclusion, understanding tendinopathy and its symptoms is vital for anyone engaged in physical activities or sports. Early recognition and appropriate management can help prevent further complications and promote recovery. Stay informed and proactive about your tendon health! 💪

Tendinopathy Causes
Tendinopathy is a condition that affects the tendons, which are the fibrous tissues connecting muscles to bones. Understanding the causes of tendinopathy is crucial for prevention and effective treatment. Here are some of the primary factors that contribute to the development of this condition:
Overuse and Repetitive Strain
One of the most common causes of tendinopathy is overuse. This occurs when a tendon is subjected to repetitive stress without adequate recovery time. Athletes and individuals engaged in repetitive activities, such as runners, cyclists, or those who perform manual labor, are particularly susceptible. The constant strain can lead to micro-tears in the tendon, resulting in inflammation and pain.
Aging
As we age, our tendons naturally lose elasticity and strength. This degeneration makes them more prone to injury and conditions like tendinopathy. Older adults may find that even low-impact activities can lead to tendon pain due to the natural wear and tear that occurs over time.
Improper Technique or Equipment
Using improper techniques during physical activities or sports can significantly increase the risk of developing tendinopathy. For instance, poor running form or using inappropriate footwear can place undue stress on the tendons. Similarly, athletes who do not use the right equipment for their sport may also be at risk.
Underlying Health Conditions
Certain health conditions can predispose individuals to tendinopathy. Conditions such as diabetes, rheumatoid arthritis, and thyroid disorders can affect tendon health and increase the likelihood of developing tendinopathy. Additionally, metabolic disorders can impair the body’s ability to repair tendons effectively.
Inadequate Warm-Up and Stretching
Failing to properly warm up before engaging in physical activity can lead to increased risk of tendon injuries. A good warm-up increases blood flow to the muscles and tendons, preparing them for the demands of exercise. Stretching is equally important, as it enhances flexibility and reduces tension in the tendons.
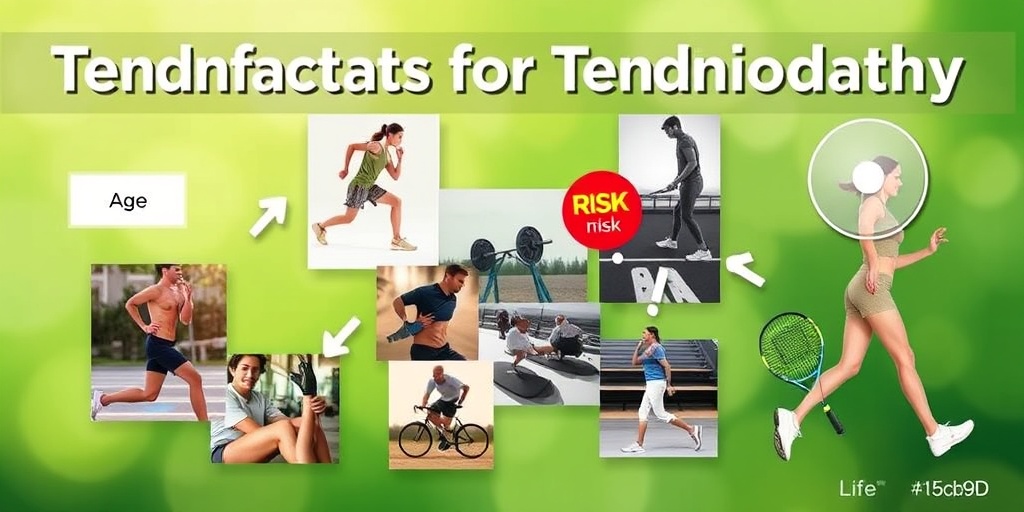
Tendinopathy Risk Factors
Identifying the risk factors associated with tendinopathy can help individuals take proactive measures to prevent this painful condition. Here are some key risk factors to consider:
Age
As mentioned earlier, age plays a significant role in the development of tendinopathy. Older adults are more likely to experience tendon degeneration, making them more susceptible to injuries. This is particularly true for tendons in the shoulder, hip, and knee, which are common sites for tendinopathy.
Occupation and Activity Level
Individuals whose jobs require repetitive motions or heavy lifting are at a higher risk for tendinopathy. Professions such as construction work, assembly line jobs, or even office work that involves prolonged computer use can contribute to tendon strain. Additionally, athletes who engage in high-impact sports are also at risk.
Previous Injuries
Having a history of tendon injuries can increase the likelihood of developing tendinopathy in the same area. Previous injuries may weaken the tendon, making it more vulnerable to future damage. It’s essential for individuals with a history of tendon issues to take extra precautions during physical activities.
Genetics
Genetic predisposition can also play a role in the development of tendinopathy. Some individuals may inherit traits that make their tendons more susceptible to injury. If you have a family history of tendon problems, it’s wise to be vigilant about your tendon health.
Obesity
Excess body weight can place additional stress on tendons, particularly in weight-bearing joints like the knees and hips. This increased strain can lead to a higher risk of developing tendinopathy. Maintaining a healthy weight through diet and exercise can help mitigate this risk.
Inadequate Recovery Time
Failing to allow sufficient recovery time between workouts can lead to overuse injuries. It’s essential to listen to your body and give your tendons time to heal after intense physical activity. Incorporating rest days and cross-training can help prevent tendinopathy.
By understanding the causes and risk factors associated with tendinopathy, individuals can take proactive steps to protect their tendon health and reduce the likelihood of developing this painful condition. 🏃♂️💪
Tendinopathy Diagnosis
Tendinopathy is a term that encompasses various tendon injuries, often characterized by pain, swelling, and impaired function. Understanding how this condition is diagnosed is crucial for effective treatment and recovery. Let’s delve into the diagnostic process for tendinopathy.
Understanding the Symptoms
The first step in diagnosing tendinopathy is recognizing its symptoms. Common signs include:
- Pain: Typically localized around the affected tendon, which may worsen with activity.
- Swelling: Inflammation may cause visible swelling around the tendon.
- Stiffness: Affected areas may feel stiff, especially after periods of inactivity.
- Reduced Range of Motion: Difficulty moving the joint associated with the tendon.
Medical History and Physical Examination
A thorough medical history is essential for diagnosing tendinopathy. Your healthcare provider will ask about:
- Your symptoms and their duration.
- Any previous injuries or conditions affecting the tendon.
- Your activity level and any recent changes in physical activity.
During the physical examination, the doctor will assess the affected area for tenderness, swelling, and range of motion. They may also perform specific tests to evaluate the tendon’s function and identify the exact location of pain.
Imaging Tests
In some cases, imaging tests may be necessary to confirm a diagnosis of tendinopathy. Common imaging techniques include:
- X-rays: While they cannot directly visualize tendons, they can rule out other conditions such as fractures.
- Ultrasound: This non-invasive test can provide real-time images of the tendon, helping to identify tears or degeneration.
- Magnetic Resonance Imaging (MRI): An MRI offers detailed images of soft tissues, making it useful for assessing the extent of tendinopathy.
By combining a thorough medical history, physical examination, and appropriate imaging tests, healthcare providers can accurately diagnose tendinopathy and differentiate it from similar conditions, such as tendonitis or tendinosis.
Tendinopathy Treatment Options
Once diagnosed, the next step is to explore treatment options for tendinopathy. The goal of treatment is to relieve pain, restore function, and prevent further injury. Here are some effective treatment strategies:
Conservative Treatments
Most cases of tendinopathy can be managed with conservative treatments, which include:
- Rest: Allowing the affected tendon to heal by reducing or modifying activities that exacerbate pain.
- Ice Therapy: Applying ice packs can help reduce swelling and alleviate pain.
- Compression: Using compression wraps can minimize swelling and provide support.
- Elevation: Keeping the affected area elevated can help reduce swelling.
Physical Therapy
Physical therapy plays a vital role in the rehabilitation of tendinopathy. A physical therapist can design a personalized exercise program that focuses on:
- Strengthening: Targeting the muscles around the affected tendon to improve stability.
- Stretching: Enhancing flexibility to prevent stiffness and promote healing.
- Manual Therapy: Techniques such as massage can help alleviate pain and improve blood flow.
Medications
Over-the-counter pain relievers, such as nonsteroidal anti-inflammatory drugs (NSAIDs), can help manage pain and inflammation associated with tendinopathy. In some cases, your doctor may recommend corticosteroid injections for more severe pain.
Advanced Treatments
If conservative treatments fail to provide relief, more advanced options may be considered:
- Platelet-Rich Plasma (PRP) Therapy: This involves injecting a concentration of platelets derived from your blood into the affected tendon to promote healing.
- Surgery: In rare cases, surgical intervention may be necessary to repair a severely damaged tendon.
It’s essential to consult with a healthcare professional to determine the most appropriate treatment plan for your specific case of tendinopathy. Early intervention and a tailored approach can significantly enhance recovery and return to normal activities. 🏃♂️💪
Tendinopathy Rehabilitation
Tendinopathy is a common condition that affects tendons, leading to pain and dysfunction. Rehabilitation is crucial for recovery and involves a combination of strategies tailored to the individual. Here’s a comprehensive guide to effective rehabilitation for tendinopathy.
Understanding Tendinopathy
Before diving into rehabilitation, it’s essential to understand what tendinopathy is. It refers to a range of tendon injuries characterized by pain, swelling, and impaired function. Unlike tendonitis, which is an acute inflammation of the tendon, tendinopathy is often a chronic condition resulting from overuse or repetitive strain.
Initial Assessment
Before starting any rehabilitation program, a thorough assessment by a healthcare professional is vital. This may include:
- Physical Examination: Assessing pain levels, range of motion, and functional limitations.
- Imaging Tests: MRI or ultrasound may be used to evaluate the extent of tendon damage.
Rehabilitation Phases
Rehabilitation for tendinopathy typically occurs in phases:
1. Acute Phase
During this phase, the focus is on reducing pain and inflammation. Strategies include:
- Rest: Avoid activities that exacerbate pain.
- Ice Therapy: Applying ice packs can help reduce swelling.
- Compression: Using elastic bandages to minimize swelling.
2. Subacute Phase
Once pain decreases, the goal shifts to restoring mobility and strength. This phase may include:
- Gentle Stretching: To improve flexibility.
- Isometric Exercises: Strengthening the tendon without movement.
3. Functional Phase
In this phase, the focus is on returning to normal activities. Key components include:
- Progressive Strengthening: Gradually increasing resistance in exercises.
- Functional Training: Activities that mimic daily tasks or sports.
Role of Physical Therapy
Working with a physical therapist can significantly enhance recovery. They can provide:
- Personalized Exercise Programs: Tailored to your specific needs.
- Manual Therapy: Techniques to improve mobility and reduce pain.
Monitoring Progress
Regularly assessing your progress is crucial. Keep track of:
- Pain Levels: Use a scale to monitor changes.
- Functional Improvements: Note any increases in activity levels.
Tendinopathy Prevention Tips
Preventing tendinopathy is often more effective than treating it. Here are some practical tips to help you avoid this painful condition.
1. Warm-Up Properly
Before engaging in any physical activity, always warm up. This increases blood flow to the muscles and tendons, reducing the risk of injury. A good warm-up should last at least 10-15 minutes and include dynamic stretches. 🏃♂️
2. Gradual Progression
When starting a new exercise program or increasing intensity, do so gradually. Sudden increases in activity can strain tendons. Follow the 10% rule: increase your activity level by no more than 10% each week.
3. Strength Training
Incorporating strength training into your routine can help build resilience in your tendons. Focus on exercises that target the muscles around the affected tendon. For example, if you’re prone to tendinopathy of the supraspinatus tendon, include shoulder strengthening exercises. 💪
4. Cross-Training
Engaging in various forms of exercise can prevent overuse injuries. Mix low-impact activities like swimming or cycling with your regular routine to give your tendons a break.
5. Listen to Your Body
Pay attention to any signs of discomfort or pain. If you experience persistent pain, it’s essential to rest and seek professional advice. Ignoring these signals can lead to chronic tendinopathy.
6. Proper Footwear
Wearing appropriate shoes for your activity can significantly reduce the risk of tendinopathy, especially in the knees and hips. Ensure your footwear provides adequate support and cushioning.
7. Stay Hydrated and Maintain a Healthy Diet
Proper hydration and nutrition play a crucial role in tendon health. Ensure you consume a balanced diet rich in vitamins and minerals, particularly those that support tendon repair, such as vitamin C and omega-3 fatty acids. 🥗
By following these rehabilitation and prevention tips, you can effectively manage and reduce the risk of tendinopathy. Remember, early intervention and consistent care are key to maintaining healthy tendons and an active lifestyle!
![]()
Frequently Asked Questions
What is the meaning of tendinopathy?
Tendinopathy refers to a condition that affects the tendons, which are the fibrous tissues connecting muscles to bones. It typically involves pain, swelling, and impaired function of the affected tendon.
How does tendinopathy differ from tendonitis?
While both terms are often used interchangeably, tendinopathy is a broader term that encompasses various tendon disorders, including tendonitis, which specifically refers to inflammation of the tendon. In contrast, tendinopathy may involve degeneration without significant inflammation.
What are common treatments for tendinopathy?
- Rest and activity modification
- Physical therapy and rehabilitation exercises
- Ice therapy to reduce swelling
- Non-steroidal anti-inflammatory drugs (NSAIDs)
- In some cases, corticosteroid injections
- Surgery may be considered for severe cases
Can tendinopathy occur in the shoulder?
Yes, tendinopathy of the shoulder is common, particularly affecting the rotator cuff tendons. Symptoms may include pain, weakness, and limited range of motion.
Is there a connection between tendinopathy and the hip?
Absolutely! Tendinopathy of the hip can occur, often affecting the gluteal tendons. This condition can lead to pain in the outer hip and difficulty with activities like walking or climbing stairs.
What about tendinopathy in the knee?
Tendinopathy of the knee is frequently seen in athletes, particularly those involved in jumping sports. It can cause pain around the kneecap or in the area of the patellar tendon.
What is the ICD-10 code for tendinopathy?
The ICD-10 code for tendinopathy varies depending on the specific tendon affected. It is essential to consult a healthcare provider for accurate coding based on individual cases.
What is tendinopathy of the supraspinatus tendon?
Tendinopathy of the supraspinatus tendon is a common shoulder condition that affects the tendon responsible for arm elevation. Symptoms may include pain and weakness, particularly when lifting the arm.
How can I prevent tendinopathy?
- Engage in proper warm-up and cool-down routines
- Gradually increase the intensity of physical activities
- Incorporate strength training to support tendon health
- Maintain flexibility through stretching exercises
When should I see a doctor for tendinopathy?
If you experience persistent pain, swelling, or difficulty performing daily activities due to tendon discomfort, it is advisable to consult a healthcare professional for an accurate diagnosis and appropriate treatment plan.




