Understanding Diabetes and Foot Health
Diabetes is a chronic condition that affects how your body processes glucose, leading to elevated blood sugar levels. One of the lesser-known complications of diabetes is its impact on foot health. Foot care for people with diabetes is crucial, as high blood sugar can lead to nerve damage (neuropathy) and poor circulation, increasing the risk of foot problems.
The Connection Between Diabetes and Foot Health
When blood sugar levels remain high over time, they can cause damage to the nerves and blood vessels in the feet. This can lead to a loss of sensation, making it difficult for individuals to feel injuries or infections. Additionally, poor circulation can hinder the healing process, making even minor cuts or blisters potentially serious.
Why is Foot Care Important for Diabetics?
Proper foot care is essential for anyone with diabetes for several reasons:
- Prevention of Complications: Regular foot care can help prevent serious complications such as ulcers, infections, and even amputations.
- Early Detection: Routine checks can help identify problems early, allowing for timely intervention.
- Improved Quality of Life: Healthy feet contribute to overall mobility and independence, enhancing daily living.
In summary, careful foot care is vitally important for people with diabetes. By understanding the risks and taking proactive steps, individuals can maintain their foot health and prevent complications.
Common Foot Problems in Diabetes
People with diabetes are at a higher risk for various foot problems. Understanding these issues can help in taking preventive measures and seeking timely treatment.
1. Diabetic Neuropathy
Diabetic neuropathy is a type of nerve damage that can occur in people with diabetes. Symptoms may include:
- Numbness or tingling in the feet
- Burning sensations
- Loss of balance and coordination
Because of the loss of sensation, individuals may not notice injuries, leading to more severe complications.
2. Foot Ulcers
Foot ulcers are open sores that can develop due to pressure, friction, or injury. They are particularly concerning for diabetics because:
- They can become infected easily.
- Healing may be slow due to poor circulation.
Regular foot inspections can help catch ulcers early, preventing them from worsening.
3. Infections
Infections can occur from minor cuts or blisters that go unnoticed. Symptoms of infection include:
- Redness and swelling
- Pus or drainage
- Increased warmth in the affected area
Prompt treatment is essential to avoid serious complications.
4. Charcot Foot
Charcot foot is a condition that results from nerve damage, leading to weakened bones and joints in the foot. This can cause:
- Deformities
- Instability
Early diagnosis and treatment are crucial to prevent further damage.
5. Fungal Infections
People with diabetes are more susceptible to fungal infections, such as athlete’s foot. Symptoms may include:
- Itching and burning
- Red, flaky skin
Maintaining good foot hygiene can help prevent these infections.
Conclusion
Understanding the connection between diabetes and foot health is vital for anyone living with this condition. By being aware of common foot problems and taking proactive steps in foot care for patients with diabetes, individuals can significantly reduce their risk of complications. For more information and resources on managing diabetes and maintaining foot health, consider visiting Yesil Health AI for evidence-based health answers.
Remember, your feet are your foundation—take care of them! 👣
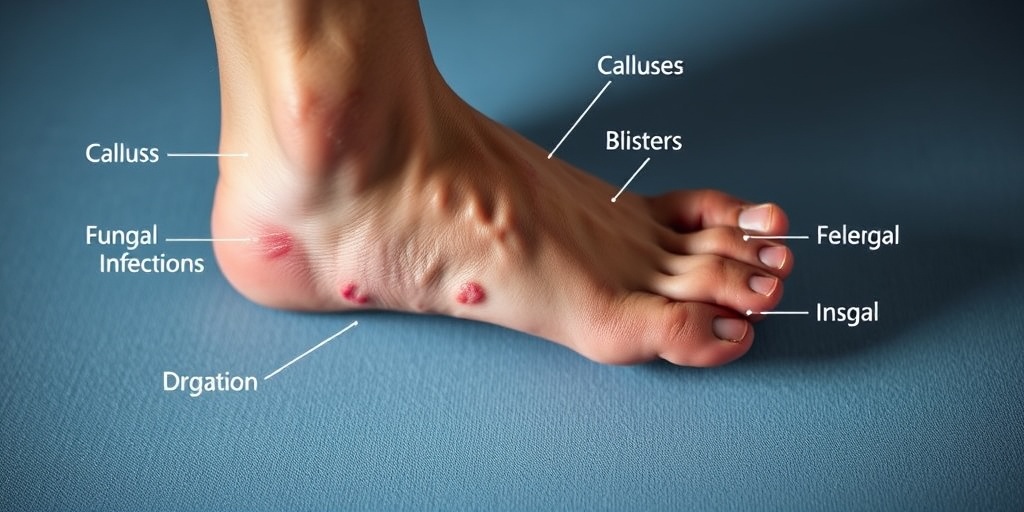
Signs of Foot Complications
For individuals with diabetes, maintaining proper foot health is crucial. Foot complications can arise due to nerve damage (neuropathy) and poor circulation, making it essential to recognize the warning signs early. Here are some common signs to watch for:
1. Numbness or Tingling
If you experience numbness or tingling in your feet, it could indicate nerve damage. This sensation may make it difficult to feel injuries or pressure, increasing the risk of complications.
2. Changes in Skin Color
Pay attention to any changes in skin color on your feet. If you notice redness, blueness, or a pale appearance, it may signal poor circulation or infection.
3. Swelling
Swelling in the feet or ankles can be a sign of fluid retention or other underlying issues. If swelling persists, consult your healthcare provider.
4. Blisters or Sores
Blisters, sores, or cuts that do not heal properly can lead to serious infections. It’s vital to treat any wounds promptly and monitor them for signs of infection, such as increased redness or pus.
5. Changes in Nail Health
Watch for changes in your toenails, such as discoloration, thickening, or fungal infections. These changes can indicate underlying health issues that require attention.
6. Foot Pain
While some discomfort is common, persistent foot pain should not be ignored. It may indicate a more serious condition, such as neuropathy or a foot ulcer.
Recognizing these signs early can help prevent serious complications. If you notice any of these symptoms, it’s important to seek medical advice promptly. Regular check-ups with your healthcare provider can also help monitor your foot health.
Daily Foot Care Routine
Establishing a daily foot care routine is essential for people with diabetes. By taking proactive steps, you can significantly reduce the risk of foot complications. Here’s a simple yet effective routine to follow:
1. Inspect Your Feet Daily
Start each day by inspecting your feet for any cuts, blisters, or abnormalities. Use a mirror if necessary to check the soles and between the toes. Early detection is key!
2. Wash Your Feet Regularly
Wash your feet daily with lukewarm water and mild soap. Avoid hot water, as it can cause burns. After washing, dry your feet thoroughly, especially between the toes, to prevent fungal infections.
3. Moisturize, But Not Between Toes
Apply a moisturizing lotion to your feet to keep the skin hydrated. However, avoid putting lotion between your toes, as this can promote fungal growth.
4. Trim Your Toenails Carefully
Keep your toenails trimmed straight across to prevent ingrown nails. If you have difficulty, consider visiting a podiatrist for professional nail care.
5. Wear Proper Footwear
Choose comfortable, well-fitting shoes that provide adequate support. Avoid walking barefoot, even at home, to protect your feet from injuries.
6. Maintain Good Blood Sugar Levels
Keeping your blood sugar levels within the target range is crucial for preventing complications. Work with your healthcare team to manage your diabetes effectively.
7. Schedule Regular Foot Exams
Make it a habit to visit your healthcare provider for regular foot exams. They can help identify any potential issues before they become serious.
By following this daily foot care routine, you can help ensure your feet remain healthy and free from complications. Remember, taking care of your feet is an essential part of managing diabetes! 🦶💙

Choosing the Right Footwear
When it comes to foot care for people with diabetes, selecting the right footwear is crucial. Proper shoes can help prevent injuries, blisters, and other complications that can arise from diabetes-related foot issues. Here are some essential tips to consider when choosing footwear:
1. Look for Comfort and Fit
Comfort should be your top priority. Shoes that fit well can help reduce the risk of foot problems. Here are some tips for finding the right fit:
- Measure Your Feet: Always measure both feet, as one foot may be larger than the other. Try on shoes in the afternoon when your feet are slightly swollen.
- Check the Width: Ensure the shoes are wide enough to accommodate any foot swelling. A snug fit can lead to blisters and calluses.
- Test the Cushioning: Shoes should have adequate cushioning to absorb shock and provide comfort during daily activities.
2. Choose the Right Material
The material of the shoe can significantly impact comfort and foot health. Consider the following:
- Breathable Fabrics: Look for shoes made from breathable materials to help keep your feet dry and reduce the risk of fungal infections.
- Soft Linings: Shoes with soft linings can prevent irritation and friction against the skin.
3. Opt for Supportive Features
Supportive shoes can help maintain proper foot alignment and reduce strain. Here are some features to look for:
- Arch Support: Shoes with good arch support can help distribute weight evenly and reduce pressure on the feet.
- Cushioned Insoles: Consider using custom orthotics or cushioned insoles for added support and comfort.
4. Avoid High Heels and Flip-Flops
While they may be fashionable, high heels and flip-flops can pose significant risks for people with diabetes. High heels can lead to balance issues and foot pain, while flip-flops offer little support and protection. Instead, opt for shoes that provide stability and coverage.
5. Regularly Inspect Your Footwear
It’s essential to regularly check your shoes for signs of wear and tear. Look for:
- Uneven Wear: If the soles are wearing unevenly, it may indicate a need for new shoes.
- Loose Parts: Ensure there are no loose seams or parts that could cause injury.
Managing Blood Sugar Levels
Another critical aspect of foot care for patients with diabetes is managing blood sugar levels. High blood sugar can lead to nerve damage and poor circulation, increasing the risk of foot complications. Here are some effective strategies for managing blood sugar levels:
1. Monitor Your Blood Sugar Regularly
Keeping track of your blood sugar levels is vital. Regular monitoring can help you understand how your body responds to different foods, activities, and medications. Aim to:
- Use a Glucometer: Invest in a reliable glucometer to check your blood sugar levels at home.
- Keep a Log: Maintain a log of your readings to identify patterns and discuss them with your healthcare provider.
2. Follow a Balanced Diet
A balanced diet plays a significant role in managing blood sugar levels. Consider these dietary tips:
- Choose Whole Foods: Focus on whole grains, lean proteins, healthy fats, and plenty of fruits and vegetables.
- Limit Sugary Foods: Reduce your intake of sugary snacks and beverages that can cause spikes in blood sugar.
3. Stay Active
Regular physical activity can help regulate blood sugar levels and improve overall health. Aim for at least 150 minutes of moderate exercise each week. Activities can include:
- Walking: A simple and effective way to stay active.
- Strength Training: Incorporate strength training exercises to build muscle and improve insulin sensitivity.
4. Take Medications as Prescribed
If you have been prescribed medication to manage your diabetes, it’s essential to take it as directed. Discuss any concerns or side effects with your healthcare provider to ensure optimal management of your condition.
5. Stay Hydrated
Drinking enough water is vital for overall health and can help manage blood sugar levels. Aim to drink at least 8 cups of water a day, and more if you are active or live in a hot climate. 💧
By focusing on proper footwear and effectively managing blood sugar levels, individuals with diabetes can significantly reduce their risk of foot complications and maintain better overall health. Remember, careful foot care is vitally important for people with diabetes, so make it a priority in your daily routine!

When to See a Doctor
Foot care for people with diabetes is not just about regular washing and moisturizing; it’s also about being vigilant and proactive. Diabetes can lead to various complications that affect foot health, making it crucial to know when to seek medical attention. Here are some signs that indicate it’s time to consult a healthcare professional:
1. Unhealed Wounds or Sores
If you notice any cuts, blisters, or sores on your feet that do not heal within a few days, it’s essential to see a doctor. Delayed healing can be a sign of poor circulation or infection, both of which are common in individuals with diabetes.
2. Changes in Skin Color or Temperature
Pay attention to any changes in the color or temperature of your feet. If one foot appears significantly warmer or cooler than the other, or if you notice a change in skin color (such as redness or paleness), it could indicate a serious issue. Circulatory problems can lead to severe complications if not addressed promptly.
3. Numbness or Tingling Sensations
Diabetic neuropathy, a common complication of diabetes, can cause numbness, tingling, or a burning sensation in the feet. If you experience these symptoms, it’s important to consult your doctor. Early intervention can help manage symptoms and prevent further nerve damage.
4. Fungal Infections
People with diabetes are more susceptible to fungal infections, such as athlete’s foot. If you notice persistent itching, redness, or a rash between your toes or on your feet, seek medical advice. Timely treatment can prevent the infection from worsening.
5. Foot Deformities
Changes in the shape of your feet, such as bunions or hammertoes, can lead to discomfort and complications. If you notice any deformities, it’s advisable to consult a podiatrist. Proper footwear and treatment can help alleviate pain and prevent further issues.
Preventive Measures for Healthy Feet
Taking proactive steps in foot care for patients with diabetes can significantly reduce the risk of complications. Here are some effective preventive measures to keep your feet healthy:
1. Daily Foot Inspections
Make it a habit to inspect your feet daily. Look for any cuts, blisters, or signs of infection. Early detection is key to preventing serious issues. Use a mirror if necessary to check the soles of your feet.
2. Maintain Proper Hygiene
Wash your feet daily with mild soap and warm water. Be sure to dry them thoroughly, especially between the toes, to prevent fungal infections. Moisturizing your feet can help prevent dry skin, but avoid applying lotion between the toes to reduce the risk of fungal growth.
3. Choose the Right Footwear
Wearing well-fitting shoes is crucial for foot health. Look for shoes that provide adequate support and cushioning. Avoid tight shoes that can cause blisters or calluses. Consider custom orthotics if you have foot deformities or other issues.
4. Keep Your Blood Sugar Levels in Check
Managing your diabetes effectively is one of the best ways to protect your feet. High blood sugar levels can lead to nerve damage and poor circulation, increasing the risk of foot problems. Regular monitoring and adhering to your treatment plan can help maintain healthy blood sugar levels.
5. Regular Check-ups with a Podiatrist
Schedule regular appointments with a podiatrist to monitor your foot health. They can provide professional advice and treatment for any issues that arise. Routine check-ups can help catch potential problems early, ensuring your feet remain healthy.
By following these preventive measures and knowing when to seek medical attention, you can significantly reduce the risk of foot complications associated with diabetes. Remember, careful foot care is vitally important for people with diabetes to maintain overall health and well-being. 🦶💙

Frequently Asked Questions about Foot Care for People with Diabetes
Why is foot care essential for individuals with diabetes?
Foot care is extremely important for people with diabetes because diabetes can lead to nerve damage and poor circulation. This increases the risk of foot injuries, infections, and complications that can result in serious health issues. Regular foot care helps in early detection of problems and prevents severe complications.
What are the best practices for foot care in diabetics?
- Inspect your feet daily for cuts, blisters, or any abnormalities.
- Wash your feet daily with mild soap and warm water, and dry them thoroughly.
- Moisturize your feet to prevent dryness, but avoid applying lotion between the toes.
- Trim your toenails straight across to prevent ingrown nails.
- Wear well-fitting shoes to avoid blisters and pressure points.
How often should diabetics check their feet?
It is recommended that individuals with diabetes check their feet daily. This helps in identifying any issues early on, allowing for prompt treatment and reducing the risk of complications.
Do diabetics qualify for free foot care services?
Many healthcare systems offer free foot care services for individuals with diabetes, especially for those who are at high risk for foot complications. It is advisable to check with local health services or diabetes organizations for available programs.
What should I do if I find a sore or cut on my foot?
If you discover a sore or cut on your foot, it is crucial to seek medical attention immediately. Do not attempt to treat it on your own, as infections can develop quickly in individuals with diabetes.
Can diabetes lead to foot ulcers?
Yes, diabetes can lead to foot ulcers due to nerve damage and poor blood flow. Regular foot care and monitoring are essential to prevent ulcers from developing.
How can I improve circulation in my feet?
Improving circulation can be achieved through several methods, including:
- Regular exercise to promote blood flow.
- Avoiding sitting or standing in one position for too long.
- Wearing compression socks if recommended by a healthcare provider.
What are the signs of foot problems in diabetics?
Signs of foot problems may include:
- Redness or swelling
- Persistent pain or discomfort
- Changes in skin color or temperature
- Open sores or wounds
- Foul odor
How should diabetics take care of their feet during winter?
During winter, it is important for diabetics to keep their feet warm and dry. Wear warm socks, avoid walking barefoot, and ensure that shoes fit well to prevent frostbite and other cold-related injuries.
What role does diet play in foot health for diabetics?
A balanced diet helps in managing blood sugar levels, which is crucial for maintaining overall foot health. Foods rich in vitamins and minerals can promote healing and improve circulation.




