What Is Diabetes?
Diabetes is a chronic health condition that occurs when the body cannot effectively regulate blood sugar (glucose) levels. Glucose is a vital source of energy for our cells, and maintaining its balance is crucial for overall health. When diabetes is present, it can lead to elevated blood sugar levels, which can cause a range of health complications if left unmanaged.
There are two primary hormones involved in blood sugar regulation: insulin and glucagon. Insulin, produced by the pancreas, helps cells absorb glucose from the bloodstream. In individuals with diabetes, either the body does not produce enough insulin, or the cells become resistant to its effects, leading to high blood sugar levels.
Understanding diabetes is essential, as it affects millions of people worldwide. According to the International Diabetes Federation, approximately 537 million adults were living with diabetes in 2021, and this number is expected to rise significantly in the coming years. Recognizing the symptoms and risk factors associated with diabetes can help in early detection and management.
Common Symptoms of Diabetes
Identifying the symptoms of diabetes is crucial for early intervention. Some common symptoms include:
- Frequent urination (polyuria)
- Increased thirst (polydipsia)
- Extreme hunger (polyphagia)
- Fatigue and weakness
- Blurred vision
- Slow-healing sores or frequent infections
If you or someone you know is experiencing these symptoms, it is essential to consult a healthcare professional for a diabetes test. Early diagnosis can significantly improve management and reduce the risk of complications.
Types of Diabetes
Diabetes is categorized into several types, each with distinct characteristics and management strategies. The most common types include:
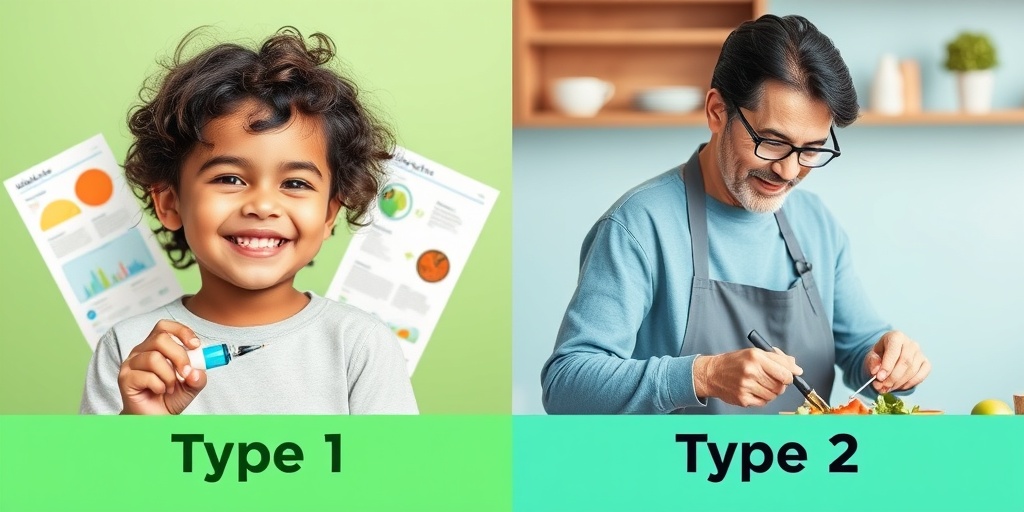
Type 1 Diabetes
Type 1 diabetes is an autoimmune condition where the immune system mistakenly attacks and destroys the insulin-producing beta cells in the pancreas. This type typically develops in children and young adults, although it can occur at any age. Individuals with type 1 diabetes require lifelong insulin therapy to manage their blood sugar levels.
Type 2 Diabetes
Type 2 diabetes is the most prevalent form of diabetes, accounting for approximately 90-95% of all cases. It usually develops in adults, although increasing numbers of children and adolescents are being diagnosed due to rising obesity rates. In type 2 diabetes, the body becomes resistant to insulin, and the pancreas cannot produce enough insulin to maintain normal blood sugar levels. Lifestyle changes, such as diet and exercise, along with medication, are often used to manage this condition.
Gestational Diabetes
Gestational diabetes occurs during pregnancy and typically resolves after childbirth. However, it can increase the risk of developing type 2 diabetes later in life for both the mother and child. Women diagnosed with gestational diabetes must monitor their blood sugar levels closely and may require dietary changes or insulin therapy during pregnancy.
Other Specific Types
There are also less common forms of diabetes, such as:
- Monogenic Diabetes: Caused by a mutation in a single gene, often inherited.
- Secondary Diabetes: Resulting from other medical conditions or medications that affect insulin production or action.
Understanding the different types of diabetes is crucial for effective management and treatment. If you suspect you may have diabetes or are at risk, consider visiting Yesil Health AI for evidence-based health answers and resources.
In conclusion, diabetes is a complex condition that requires awareness and proactive management. By understanding what diabetes is and the various types, individuals can take steps towards better health and well-being. Remember, early detection and lifestyle changes can make a significant difference in managing diabetes effectively. 🌟
Diabetes Symptoms
Diabetes is a chronic condition that affects how your body processes blood sugar (glucose). Recognizing the symptoms early can lead to better management and treatment. Here are some common symptoms associated with diabetes:
Common Symptoms of Diabetes
- Increased Thirst: One of the first signs of diabetes is excessive thirst. This occurs because your body is trying to flush out excess sugar through urine, leading to dehydration.
- Frequent Urination: As your kidneys work harder to eliminate sugar from your blood, you may find yourself needing to urinate more often, especially at night.
- Extreme Hunger: Despite eating, people with diabetes often feel hungry. This is due to the body’s inability to use glucose effectively for energy.
- Fatigue: Feeling unusually tired can be a symptom of diabetes. When your body can’t use glucose properly, it can lead to a lack of energy.
- Blurred Vision: High blood sugar levels can cause the lenses of your eyes to swell, leading to blurred vision.
- Slow Healing Sores: Cuts and bruises may take longer to heal, which can be a sign of diabetes-related complications.
- Unexplained Weight Loss: In type 1 diabetes, the body may start breaking down muscle and fat for energy, leading to weight loss.
- Dark Patches of Skin: Some people with diabetes develop dark, velvety patches of skin, often in the folds of the neck or armpits, known as acanthosis nigricans.
Symptoms in Women
Women may experience specific symptoms related to diabetes, including:
- Frequent Yeast Infections: High blood sugar levels can create an environment conducive to yeast growth.
- Polycystic Ovary Syndrome (PCOS): Women with diabetes may also experience symptoms of PCOS, which can include irregular periods and fertility issues.
If you notice any of these symptoms, it’s essential to consult a healthcare professional for a proper diagnosis and management plan. Early detection can significantly improve your quality of life and reduce the risk of complications. 🩺
Diabetes Causes
Understanding the causes of diabetes is crucial for prevention and management. Diabetes can be broadly categorized into two main types: Type 1 and Type 2, each with different causes.
Type 1 Diabetes Causes
Type 1 diabetes is an autoimmune condition where the body’s immune system attacks insulin-producing cells in the pancreas. The exact cause is not fully understood, but several factors may contribute:
- Genetics: A family history of Type 1 diabetes can increase the risk.
- Environmental Factors: Certain viruses may trigger the autoimmune response that leads to Type 1 diabetes.
Type 2 Diabetes Causes
Type 2 diabetes is more common and is often linked to lifestyle factors. Here are some primary causes:
- Obesity: Excess body fat, particularly around the abdomen, is a significant risk factor for Type 2 diabetes.
- Physical Inactivity: A sedentary lifestyle can contribute to weight gain and insulin resistance.
- Poor Diet: Diets high in processed foods, sugars, and unhealthy fats can increase the risk of developing Type 2 diabetes.
- Age: The risk of Type 2 diabetes increases with age, especially after 45.
- Family History: A family history of diabetes can also increase your risk.
Other Contributing Factors
In addition to the above, other factors can contribute to the development of diabetes:
- Hormonal Changes: Conditions like polycystic ovary syndrome (PCOS) can increase the risk of Type 2 diabetes.
- Sleep Disorders: Conditions such as sleep apnea can increase the risk of insulin resistance.
Understanding these causes can help you take proactive steps to reduce your risk of diabetes. Maintaining a healthy lifestyle, including a balanced diet and regular exercise, is essential for prevention. 🌱

Risk Factors for Diabetes
Diabetes is a chronic condition that affects millions of people worldwide. Understanding the risk factors associated with diabetes is crucial for prevention and early intervention. Here, we’ll explore the various factors that can increase your likelihood of developing this condition.
Genetic Predisposition
One of the most significant risk factors for diabetes is your family history. If you have a parent or sibling with diabetes, your chances of developing the disease increase. This genetic link is particularly strong for Type 2 diabetes, where lifestyle factors often interact with genetic predispositions.
Age
As we age, our risk for developing diabetes increases. Individuals over the age of 45 are at a higher risk, especially if they are overweight or have a sedentary lifestyle. However, it’s important to note that Type 2 diabetes is increasingly being diagnosed in younger populations, including children and adolescents, due to rising obesity rates.
Obesity and Physical Inactivity
Being overweight is one of the most significant risk factors for diabetes. Excess body fat, particularly around the abdomen, can lead to insulin resistance, a precursor to diabetes. Regular physical activity helps maintain a healthy weight and improves insulin sensitivity. Aim for at least 150 minutes of moderate exercise each week to reduce your risk. 🏃♂️
Poor Diet
A diet high in processed foods, sugars, and unhealthy fats can contribute to weight gain and increase the risk of diabetes. Consuming a balanced diet rich in whole grains, fruits, vegetables, and lean proteins can help mitigate this risk. Pay attention to portion sizes and try to limit sugary beverages and snacks. 🍏🥦
High Blood Pressure and Cholesterol Levels
Having high blood pressure or abnormal cholesterol levels can increase your risk of developing diabetes. These conditions often coexist with diabetes and can lead to serious complications. Regular check-ups with your healthcare provider can help monitor these factors and keep them in check.
Gestational Diabetes
Women who have experienced gestational diabetes during pregnancy are at a higher risk of developing Type 2 diabetes later in life. If you had gestational diabetes, it’s essential to maintain a healthy lifestyle and have regular screenings for diabetes after pregnancy.
Ethnicity
Certain ethnic groups are at a higher risk for diabetes, including African Americans, Hispanic Americans, Native Americans, and some Asian Americans. Understanding your ethnic background can help you take proactive steps in managing your health.
Diabetes Diagnosis
Diagnosing diabetes early is crucial for effective management and prevention of complications. There are several tests that healthcare providers use to determine if someone has diabetes.
Fasting Blood Sugar Test
The fasting blood sugar test measures your blood sugar levels after an overnight fast. A reading of 126 mg/dL (7.0 mmol/L) or higher indicates diabetes. This test is often the first step in diagnosing diabetes.
Oral Glucose Tolerance Test (OGTT)
The OGTT involves fasting overnight and then drinking a sugary solution. Blood sugar levels are tested two hours later. A reading of 200 mg/dL (11.1 mmol/L) or higher indicates diabetes. This test is particularly useful for diagnosing gestational diabetes.
A1C Test
The A1C test measures your average blood sugar levels over the past two to three months. An A1C level of 6.5% or higher indicates diabetes. This test is convenient as it doesn’t require fasting and can be done at any time of the day.
Symptoms to Watch For
Being aware of the symptoms of diabetes can help you seek medical advice sooner. Common symptoms include:
- Increased thirst and frequent urination
- Extreme fatigue
- Blurred vision
- Slow-healing sores or frequent infections
- Unexplained weight loss
If you experience any of these symptoms, it’s essential to consult with a healthcare professional for further evaluation. Early diagnosis can lead to better management and improved health outcomes. 🩺

Diabetes Management
Managing diabetes is crucial for maintaining a healthy lifestyle and preventing complications. Whether you have Type 1 or Type 2 diabetes, understanding how to effectively manage your condition can lead to better health outcomes. Here are some essential strategies for diabetes management:
1. Monitoring Blood Sugar Levels
Regularly checking your blood sugar levels is vital. This helps you understand how your body responds to different foods, activities, and medications. Aim to monitor your levels at various times throughout the day, especially before and after meals. Keeping a log can help you identify patterns and make necessary adjustments.
2. Healthy Eating Habits
Nutrition plays a significant role in diabetes management. Focus on a balanced diet that includes:
- Whole grains – such as brown rice and quinoa
- Fruits and vegetables – rich in fiber and vitamins
- Lean proteins – like chicken, fish, and legumes
- Healthy fats – such as avocados and nuts
Be mindful of portion sizes and try to limit foods high in sugar and refined carbohydrates. Consider consulting a registered dietitian for personalized meal planning.
3. Regular Physical Activity
Exercise is another cornerstone of diabetes management. Aim for at least 150 minutes of moderate aerobic activity each week, such as brisk walking, swimming, or cycling. Incorporating strength training exercises at least twice a week can also help improve insulin sensitivity and overall health. 🏋️♂️
4. Medication Management
For many individuals with diabetes, medication is necessary to help control blood sugar levels. This may include:
- Insulin therapy – essential for those with Type 1 diabetes
- Oral medications – for Type 2 diabetes, which help the body use insulin more effectively
Always follow your healthcare provider’s instructions regarding medication and discuss any concerns or side effects you may experience.
5. Stress Management
Stress can significantly impact blood sugar levels. Incorporating stress-reducing techniques such as yoga, meditation, or deep-breathing exercises can be beneficial. Finding hobbies or activities that bring you joy can also help alleviate stress. 🧘♀️
6. Regular Check-ups
Routine visits to your healthcare provider are essential for monitoring your diabetes management plan. Regular check-ups can help catch any potential complications early and allow for timely interventions. Don’t forget to schedule eye exams and foot checks, as diabetes can affect these areas.
Diabetes Complications
While effective management can significantly reduce the risk of complications, it’s essential to be aware of the potential issues that can arise from diabetes. Here are some common complications associated with diabetes:
1. Cardiovascular Disease
Individuals with diabetes are at a higher risk for heart disease and stroke. High blood sugar levels can damage blood vessels and nerves that control the heart. Maintaining a healthy lifestyle, including a balanced diet and regular exercise, can help mitigate this risk.
2. Neuropathy
Diabetic neuropathy is a type of nerve damage that can occur with prolonged high blood sugar levels. Symptoms may include tingling, pain, or loss of feeling in the extremities. Regular foot care is crucial to prevent injuries and infections.
3. Kidney Damage
Diabetes can lead to kidney disease, known as diabetic nephropathy. The kidneys filter waste from the blood, and high blood sugar can impair their function. Regular monitoring of kidney function through blood tests is essential for early detection.
4. Eye Complications
Diabetes increases the risk of serious eye conditions, including diabetic retinopathy, cataracts, and glaucoma. Regular eye exams can help detect these issues early, allowing for timely treatment and prevention of vision loss.
5. Skin Conditions
People with diabetes are more susceptible to skin infections and conditions. Maintaining good hygiene and managing blood sugar levels can help prevent these issues. If you notice any unusual skin changes, consult your healthcare provider promptly.
6. Foot Problems
Due to nerve damage and poor circulation, foot problems are common in individuals with diabetes. Regular foot care, including daily inspections and proper footwear, is essential to prevent serious complications, such as ulcers or infections. 👣
Understanding diabetes management and potential complications is crucial for anyone living with this condition. By taking proactive steps, you can lead a healthier, more fulfilling life while minimizing the risks associated with diabetes.

Frequently Asked Questions about Diabetes
What is Diabetes?
Diabetes is a chronic condition that occurs when the body cannot effectively regulate blood sugar (glucose) levels. This can happen due to insufficient insulin production or the body’s inability to use insulin properly.
What are the main types of Diabetes?
- Type 1 Diabetes: An autoimmune condition where the body attacks insulin-producing cells in the pancreas.
- Type 2 Diabetes: The most common form, where the body becomes resistant to insulin or doesn’t produce enough.
- Gestational Diabetes: A temporary condition that occurs during pregnancy, affecting how cells use sugar.
- Diabetes Insipidus: A rare condition unrelated to blood sugar levels, characterized by excessive thirst and urination.
What are the common symptoms of Diabetes?
Common diabetes symptoms include:
- Increased thirst and frequent urination
- Extreme fatigue
- Blurred vision
- Slow-healing sores or frequent infections
- Unexplained weight loss
How is Diabetes diagnosed?
Diabetes can be diagnosed through various tests, including:
- Fasting Blood Sugar Test: Measures blood sugar after an overnight fast.
- Oral Glucose Tolerance Test: Measures blood sugar before and after consuming a sugary drink.
- A1C Test: Provides an average blood sugar level over the past 2-3 months.
Can Diabetes be managed effectively?
Yes, diabetes management involves a combination of lifestyle changes, medication, and regular monitoring of blood sugar levels. Key strategies include:
- Maintaining a balanced diet
- Regular physical activity
- Monitoring blood sugar levels
- Taking prescribed medications as directed
What lifestyle changes can help manage Diabetes?
To manage diabetes effectively, consider the following lifestyle changes:
- Eating a healthy diet rich in whole grains, fruits, and vegetables
- Engaging in regular exercise, such as walking, swimming, or cycling
- Maintaining a healthy weight
- Avoiding smoking and limiting alcohol consumption
Is there a cure for Diabetes?
Currently, there is no cure for diabetes, but it can be managed effectively with the right treatment and lifestyle changes. Ongoing research continues to explore potential cures and advancements in treatment.
Where can I find support for managing Diabetes?
Support for managing diabetes can be found through:
- Healthcare providers and diabetes educators
- Support groups and community organizations
- Online forums and resources
- Educational programs and workshops
What are the long-term complications of Diabetes?
If not managed properly, diabetes can lead to serious long-term complications, including:
- Heart disease and stroke
- Nerve damage (neuropathy)
- Kidney damage (nephropathy)
- Eye damage (retinopathy)
- Foot damage and infections
How can I learn more about Diabetes?
To learn more about diabetes, consider visiting reputable health websites, consulting with healthcare professionals, or reading books and articles dedicated to diabetes education.




