What Is Primary Ciliary Dyskinesia?
Primary Ciliary Dyskinesia (PCD) is a rare genetic disorder that affects the cilia, which are tiny hair-like structures lining the respiratory tract, reproductive system, and other organs. These cilia play a crucial role in moving mucus and other substances out of the body. When they don’t function properly due to PCD, it can lead to a variety of health issues.
PCD is often inherited in an autosomal recessive manner, meaning that a child must receive a defective gene from both parents to develop the condition. This disorder is characterized by the abnormal structure or function of cilia, which can lead to chronic respiratory infections, fertility issues, and other complications.
The Importance of Cilia
Cilia are essential for maintaining the health of various systems in the body. In the respiratory system, they help clear mucus and pathogens, preventing infections. In the reproductive system, they assist in the movement of eggs from the ovaries to the uterus. When cilia are impaired, the body struggles to perform these functions effectively, leading to a range of symptoms and complications.
How Common Is PCD?
PCD is considered a rare condition, affecting approximately 1 in 10,000 to 1 in 20,000 individuals worldwide. However, it is often underdiagnosed or misdiagnosed due to its similarity to other respiratory conditions, such as cystic fibrosis. Early diagnosis and intervention are crucial for managing symptoms and improving quality of life.
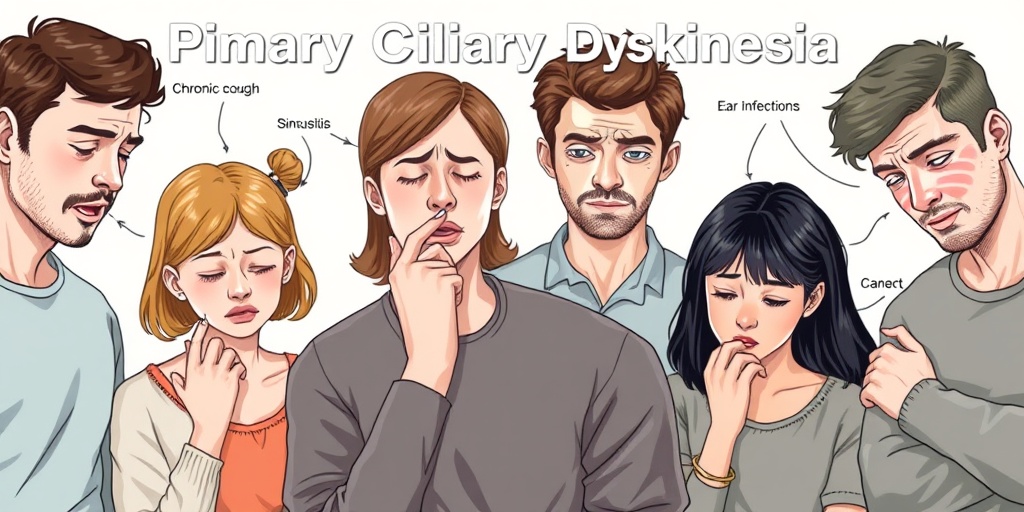
Primary Ciliary Dyskinesia Symptoms
The symptoms of Primary Ciliary Dyskinesia can vary widely among individuals, but they typically manifest in the respiratory system and may include:
- Chronic Cough: A persistent cough that may produce mucus is common in individuals with PCD.
- Frequent Respiratory Infections: People with PCD often experience recurrent infections, such as bronchitis and pneumonia.
- Sinusitis: Chronic sinus infections and inflammation are prevalent due to impaired mucus clearance.
- Ear Infections: Fluid buildup in the ears can lead to frequent ear infections and hearing loss.
- Infertility: In males, PCD can lead to reduced sperm motility, while females may experience difficulties with egg transport.
The PCD Triad
One of the hallmark features of Primary Ciliary Dyskinesia is the “PCD triad,” which includes:
- Chronic Respiratory Symptoms: As mentioned, these can include cough, wheezing, and difficulty breathing.
- Situs Inversus: Some individuals with PCD may have a condition where their internal organs are mirrored from their normal positions, known as situs inversus.
- Infertility: As previously noted, both men and women may face fertility challenges due to the effects of PCD on cilia.
Diagnosis and Treatment
Diagnosing Primary Ciliary Dyskinesia can be challenging, often requiring a combination of clinical evaluation, imaging studies, and genetic testing. The ICD-10 code for PCD is Q34.0, which healthcare providers use for billing and documentation purposes.
Treatment for PCD focuses on managing symptoms and preventing complications. This may include:
- Airway Clearance Techniques: These methods help clear mucus from the lungs, reducing the risk of infections.
- Medications: Antibiotics may be prescribed to treat infections, while bronchodilators can help open airways.
- Fertility Treatments: For those facing infertility, assisted reproductive technologies may be recommended.
For more detailed information and resources on Primary Ciliary Dyskinesia, consider visiting Yesil Health AI, where you can find evidence-based health answers tailored to your needs.
In conclusion, understanding Primary Ciliary Dyskinesia is crucial for early diagnosis and effective management. If you or someone you know is experiencing symptoms associated with PCD, it’s essential to consult a healthcare professional for a thorough evaluation and appropriate care. 🌟
Causes of Primary Ciliary Dyskinesia
Primary Ciliary Dyskinesia (PCD) is a rare genetic disorder that affects the cilia, the tiny hair-like structures that line the respiratory tract, reproductive system, and other organs. These cilia play a crucial role in moving mucus and other substances out of the body. When they don’t function properly, it can lead to a variety of health issues. Understanding the causes of PCD is essential for diagnosis and management.
Genetic Mutations
The primary cause of Primary Ciliary Dyskinesia is genetic mutations. PCD is typically inherited in an autosomal recessive manner, meaning that a child must inherit two copies of the mutated gene—one from each parent—to develop the condition. Over 40 different genes have been associated with PCD, with the most common mutations occurring in the DNAH5 and DNAI1 genes. These genes are responsible for the structure and function of cilia.
Impaired Ciliary Function
In individuals with PCD, the cilia may be immotile or exhibit abnormal movement patterns. This impairment can lead to a buildup of mucus in the lungs and other organs, resulting in chronic respiratory infections and other complications. The dysfunction of cilia can also affect the movement of sperm in males, leading to fertility issues.
Environmental Factors
While genetic factors are the primary cause of PCD, environmental factors may also play a role in exacerbating symptoms. For instance, exposure to pollutants, allergens, and respiratory infections can worsen the condition and lead to more severe health issues. However, these factors do not cause PCD but can influence the severity of symptoms in those already affected.
Risk Factors for Primary Ciliary Dyskinesia
Identifying the risk factors for Primary Ciliary Dyskinesia can help in early diagnosis and management. While PCD is primarily a genetic condition, certain factors can increase the likelihood of developing the disorder or experiencing more severe symptoms.
Family History
Having a family history of PCD or related genetic disorders significantly increases the risk of developing the condition. If one or both parents are carriers of the mutated genes associated with PCD, their children are at a higher risk of inheriting the disorder. Genetic counseling can be beneficial for families with a history of PCD.
Ethnicity
Research indicates that certain ethnic groups may have a higher prevalence of Primary Ciliary Dyskinesia. For example, individuals of Northern European descent are more likely to be affected by PCD compared to those from other regions. Understanding these demographic factors can aid in early detection and treatment.
Gender
While PCD affects both males and females, some studies suggest that males may experience more severe symptoms. This difference may be attributed to the impact of ciliary dysfunction on male fertility, as well as variations in immune response between genders.
Associated Conditions
Individuals with certain associated conditions may also be at a higher risk for developing PCD. For instance, those with congenital heart defects or situs inversus (a condition where internal organs are reversed) often have a higher incidence of PCD. Recognizing these associations can help healthcare providers in diagnosing and managing the disorder effectively.
Environmental Exposures
As mentioned earlier, while environmental factors do not cause PCD, they can exacerbate symptoms. Exposure to tobacco smoke, air pollution, and respiratory infections can increase the risk of complications in individuals with PCD. Maintaining a healthy environment and minimizing exposure to harmful substances can be beneficial for those affected.
In summary, understanding the causes and risk factors associated with Primary Ciliary Dyskinesia is crucial for effective management and treatment. Early diagnosis can lead to better outcomes and improved quality of life for individuals living with this condition. 🌬️💙
Diagnosis of Primary Ciliary Dyskinesia
Diagnosing Primary Ciliary Dyskinesia (PCD) can be a complex process, as its symptoms often overlap with other respiratory conditions. However, early and accurate diagnosis is crucial for effective management and treatment. Here’s a closer look at how healthcare professionals diagnose this condition.
Clinical Evaluation
The first step in diagnosing PCD typically involves a thorough clinical evaluation. Physicians will review the patient’s medical history and conduct a physical examination. Key symptoms to discuss include:
- Chronic respiratory infections
- Persistent cough
- Ear infections
- Sinusitis
Additionally, the physician may inquire about family history, as PCD is often inherited in an autosomal recessive manner. This means that both parents must carry the gene mutation for their child to be affected.
Diagnostic Tests
Once a clinical evaluation is complete, several diagnostic tests may be employed to confirm the presence of PCD:
- Ciliary Function Tests: These tests assess the movement of cilia in respiratory cells. A sample of nasal epithelial cells is taken and analyzed under a microscope to observe ciliary motility.
- Genetic Testing: Genetic tests can identify mutations in genes associated with PCD. This is particularly useful for confirming a diagnosis when ciliary function tests are inconclusive.
- High-Resolution CT Scan: Imaging studies can reveal structural abnormalities in the lungs and sinuses, which may indicate PCD.
- Electron Microscopy: This advanced imaging technique allows for a detailed examination of cilia structure, helping to identify any defects.
It’s important to note that diagnosing PCD can take time, and a combination of these tests may be necessary to reach a definitive conclusion. Early diagnosis can significantly improve the quality of life for individuals with PCD by enabling timely interventions.
Complications of Primary Ciliary Dyskinesia
Living with Primary Ciliary Dyskinesia can lead to various complications, primarily due to the chronic respiratory issues associated with the condition. Understanding these complications is essential for effective management and treatment.
Respiratory Complications
One of the most significant complications of PCD is the increased risk of respiratory infections. The impaired function of cilia means that mucus and pathogens are not cleared effectively from the airways, leading to:
- Chronic Bronchitis: Persistent inflammation of the bronchial tubes can occur, resulting in a chronic cough and difficulty breathing.
- Pneumonia: Recurrent lung infections can lead to pneumonia, which may require hospitalization and aggressive treatment.
- Bronchiectasis: Over time, chronic infections can cause permanent damage to the airways, leading to bronchiectasis, a condition characterized by abnormal widening of the bronchi.
Ear and Sinus Issues
Individuals with PCD often experience complications related to the ears and sinuses:
- Chronic Sinusitis: The inability to clear mucus can lead to persistent sinus infections, causing facial pain, nasal congestion, and headaches.
- Otitis Media: Frequent ear infections are common, which can lead to hearing loss if not managed properly.
Fertility Challenges
Another complication of PCD is related to fertility. In males, the absence or dysfunction of cilia in the reproductive tract can lead to infertility. Women may also face challenges, although the impact on fertility is less clear. It’s essential for individuals with PCD to discuss these concerns with their healthcare provider.
Psychosocial Impact
The chronic nature of PCD and its complications can also have a significant psychosocial impact. Patients may experience:
- Emotional Distress: Living with a chronic illness can lead to anxiety and depression.
- Social Isolation: Frequent hospital visits and illness can limit social interactions and activities.
Addressing these psychosocial aspects is crucial for comprehensive care and improving the overall quality of life for individuals with PCD.
In conclusion, while the diagnosis of Primary Ciliary Dyskinesia can be challenging, understanding the potential complications can help patients and healthcare providers work together to manage the condition effectively. Regular monitoring and a proactive approach to treatment can significantly enhance the quality of life for those affected by PCD. 🌟

Treatment Options for Primary Ciliary Dyskinesia
Primary Ciliary Dyskinesia (PCD) is a rare genetic disorder that affects the cilia, the tiny hair-like structures that line the respiratory tract and other organs. These cilia play a crucial role in clearing mucus and debris from the airways. When they don’t function properly, it can lead to a range of respiratory issues and other complications. Fortunately, there are several treatment options available to help manage the symptoms and improve the quality of life for those living with PCD.
Medications
Medications are often the first line of defense in managing primary ciliary dyskinesia symptoms. These may include:
- Bronchodilators: These medications help open the airways, making it easier to breathe.
- Anti-inflammatory drugs: These can reduce inflammation in the airways, helping to alleviate symptoms.
- Antibiotics: Regular use of antibiotics may be necessary to treat or prevent respiratory infections, which are common in individuals with PCD.
Airway Clearance Techniques
Effective airway clearance is essential for individuals with PCD. Techniques may include:
- Chest physiotherapy: This involves manual techniques to help loosen mucus in the lungs.
- Positive expiratory pressure (PEP) devices: These devices help keep the airways open and facilitate mucus clearance.
- High-frequency chest wall oscillation: This technique uses a vest that vibrates to help dislodge mucus from the lungs.
Regular Monitoring and Follow-Up
Regular check-ups with a healthcare provider are crucial for managing primary ciliary dyskinesia. These visits may include:
- Pulmonary function tests: To assess lung function and monitor any changes over time.
- Imaging studies: Such as chest X-rays or CT scans to evaluate lung health.
- Genetic counseling: For families affected by PCD, understanding the genetic implications can be beneficial.
Potential Surgical Options
In some cases, surgical interventions may be necessary. For example, individuals with severe sinus issues may benefit from sinus surgery to improve drainage and reduce infections. However, surgery is typically considered only after other treatment options have been explored.
Living with Primary Ciliary Dyskinesia
Living with primary ciliary dyskinesia (PCD) can be challenging, but with the right strategies and support, individuals can lead fulfilling lives. Here are some tips for managing daily life with PCD:
Establishing a Routine
Creating a daily routine that incorporates treatment and self-care is essential. This may include:
- Medication schedules: Keeping track of medications and ensuring they are taken as prescribed.
- Airway clearance: Setting aside time each day for airway clearance techniques.
- Regular exercise: Engaging in physical activity can help improve lung function and overall health.
Nutrition and Hydration
Maintaining a balanced diet and staying hydrated is vital for individuals with PCD. Proper nutrition can support the immune system and overall health. Consider the following:
- Hydration: Drinking plenty of fluids helps thin mucus, making it easier to clear from the lungs.
- Healthy diet: Focus on a diet rich in fruits, vegetables, whole grains, and lean proteins to support overall health.
Emotional Support
Living with a chronic condition like PCD can take an emotional toll. Seeking support from friends, family, or support groups can be beneficial. Connecting with others who understand the challenges of PCD can provide comfort and encouragement. 💙
Education and Advocacy
Being informed about primary ciliary dyskinesia is empowering. Educating yourself about the condition, treatment options, and potential complications can help you advocate for your health needs. Consider:
- Joining support groups: These can provide valuable resources and connections.
- Staying informed: Keep up with the latest research and treatment options for PCD.
By taking proactive steps and utilizing available resources, individuals with primary ciliary dyskinesia can manage their condition effectively and lead active, fulfilling lives. 🌟

Frequently Asked Questions about Primary Ciliary Dyskinesia
What is Primary Ciliary Dyskinesia (PCD)?
Primary Ciliary Dyskinesia is a genetic disorder that affects the cilia, which are tiny hair-like structures that line the respiratory tract and other organs. These cilia play a crucial role in moving mucus and clearing debris from the airways. In individuals with PCD, the cilia do not function properly, leading to respiratory issues and other complications.
What are the common symptoms of Primary Ciliary Dyskinesia?
Symptoms of Primary Ciliary Dyskinesia can vary but often include:
- Chronic cough
- Frequent respiratory infections
- Sinusitis
- Ear infections
- Reduced fertility in both men and women
How is Primary Ciliary Dyskinesia diagnosed?
Diagnosis of Primary Ciliary Dyskinesia typically involves a combination of clinical evaluation, family history, and specialized tests. These may include:
- Ciliary motion analysis
- Genetic testing
- Imaging studies such as CT scans
What treatments are available for Primary Ciliary Dyskinesia?
While there is no cure for Primary Ciliary Dyskinesia, treatments focus on managing symptoms and preventing complications. Common treatment options include:
- Chest physiotherapy to help clear mucus
- Medications to treat infections
- Inhaled therapies to improve lung function
How does Primary Ciliary Dyskinesia differ from cystic fibrosis?
While both Primary Ciliary Dyskinesia and cystic fibrosis affect the respiratory system, they are distinct conditions. PCD is primarily a disorder of ciliary function, whereas cystic fibrosis is caused by a mutation in the CFTR gene, leading to thick mucus production. Diagnosis and treatment strategies also differ between the two conditions.
What is the ICD-10 code for Primary Ciliary Dyskinesia?
The ICD-10 code for Primary Ciliary Dyskinesia is Q34.0. This code is used for medical billing and documentation purposes.
Can Primary Ciliary Dyskinesia affect fertility?
Yes, Primary Ciliary Dyskinesia can affect fertility. In men, it may lead to reduced sperm motility, while in women, it can impact the function of the fallopian tubes. Couples facing fertility issues should consult a specialist for guidance.
Is there ongoing research on Primary Ciliary Dyskinesia?
Yes, research on Primary Ciliary Dyskinesia is ongoing, focusing on better understanding the condition, improving diagnostic methods, and developing new treatments. Clinical trials may also be available for patients seeking innovative therapies.




