What Is Hypercalcemia?
Hypercalcemia is a medical condition characterized by an abnormally high level of calcium in the blood. Calcium is essential for various bodily functions, including muscle contraction, nerve transmission, and blood clotting. However, when calcium levels exceed the normal range, it can lead to a range of health issues.
Causes of Hypercalcemia
There are several potential causes of hypercalcemia, including:
- Hyperparathyroidism: This is the most common cause, where the parathyroid glands produce too much parathyroid hormone (PTH), leading to increased calcium release from bones.
- Cancer: Certain cancers, particularly those affecting the bones, can cause elevated calcium levels due to the release of calcium from the bones into the bloodstream.
- Vitamin D Overdose: Excessive intake of vitamin D can lead to increased calcium absorption from the intestines.
- Medications: Some medications, such as thiazide diuretics, can increase calcium levels.
- Other Conditions: Conditions like sarcoidosis and tuberculosis can also lead to hypercalcemia.
Symptoms of Hypercalcemia
Symptoms of hypercalcemia can vary widely, and some individuals may not experience any symptoms at all. Common symptoms include:
- Fatigue and weakness
- Nausea and vomiting
- Increased thirst and frequent urination
- Confusion or cognitive changes
- Bone pain
If left untreated, hypercalcemia can lead to serious complications, including kidney stones, osteoporosis, and cardiovascular issues. Therefore, it is crucial to seek medical attention if you suspect you have elevated calcium levels.
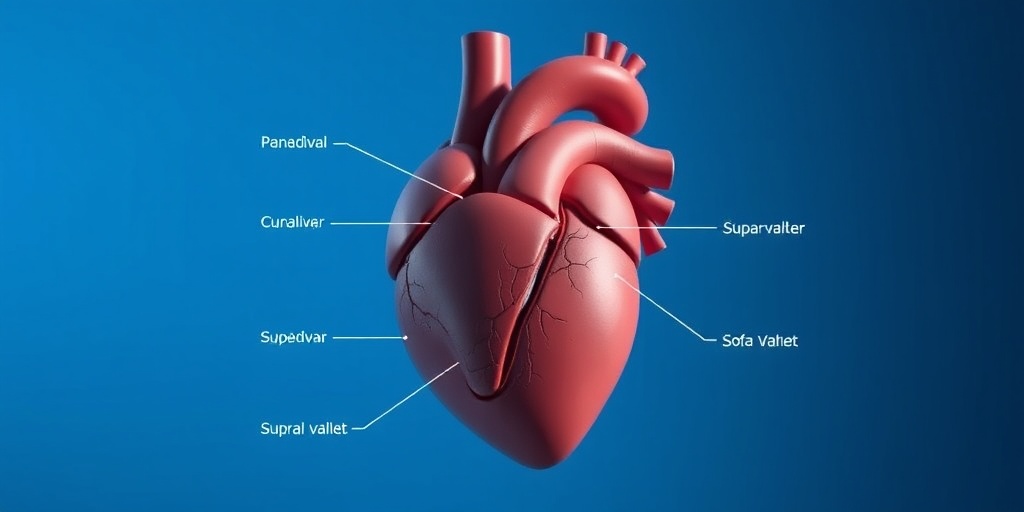
What Is Supravalvar Aortic Stenosis?
Supravalvar aortic stenosis (SVAS) is a rare congenital heart defect characterized by a narrowing of the aorta just above the aortic valve. This condition can restrict blood flow from the heart to the rest of the body, leading to various health complications.
Causes of Supravalvar Aortic Stenosis
SVAS is often associated with genetic conditions, particularly Williams syndrome, which is caused by a deletion of genetic material on chromosome 7. The exact cause of SVAS in other cases may not be well understood, but it is believed to result from abnormal development of the aorta during fetal growth.
Symptoms of Supravalvar Aortic Stenosis
The symptoms of SVAS can vary depending on the severity of the condition. Some common symptoms include:
- Shortness of breath, especially during physical activity
- Chest pain or discomfort
- Fatigue
- Heart murmurs detected during a physical examination
In severe cases, SVAS can lead to serious complications, including heart failure, high blood pressure, and other cardiovascular issues. Early diagnosis and intervention are crucial for managing this condition effectively.
Diagnosis and Treatment
Diagnosis of SVAS typically involves imaging studies such as echocardiograms, MRI, or CT scans to visualize the aorta and assess the severity of the stenosis. Treatment options may include:
- Monitoring: In mild cases, regular monitoring may be sufficient.
- Medications: Medications may be prescribed to manage symptoms and reduce blood pressure.
- Surgery: In more severe cases, surgical intervention may be necessary to repair or replace the affected section of the aorta.
Understanding conditions like hypercalcemia and supravalvar aortic stenosis is essential for effective management and treatment. If you or someone you know is experiencing symptoms related to these conditions, it is vital to consult a healthcare professional for proper evaluation and care.
For more information on health-related topics, consider visiting Yesil Health AI, a valuable resource for evidence-based health answers. 🌟
Symptoms of Hypercalcemia
Hypercalcemia, a condition characterized by elevated levels of calcium in the blood, can lead to a variety of symptoms that may range from mild to severe. Understanding these symptoms is crucial for early detection and management. Here are some common signs to watch for:
1. Digestive Issues
One of the first areas affected by hypercalcemia is the digestive system. Individuals may experience:
- Nausea – A feeling of sickness that can lead to vomiting.
- Constipation – Difficulty in passing stools, which can be uncomfortable.
- Loss of Appetite – A decreased desire to eat, which can lead to weight loss.
2. Neurological Symptoms
High calcium levels can also impact the nervous system, leading to symptoms such as:
- Confusion – Difficulty in thinking clearly or concentrating.
- Fatigue – A persistent feeling of tiredness or lack of energy.
- Depression – Mood changes that can affect daily life.
3. Musculoskeletal Symptoms
Muscle and bone health can be compromised due to hypercalcemia, resulting in:
- Muscle Weakness – A noticeable decrease in strength.
- Bone Pain – Discomfort or pain in the bones, which can be debilitating.
4. Cardiovascular Symptoms
Elevated calcium levels can also affect heart function, leading to:
- Irregular Heartbeat – Palpitations or a feeling of the heart racing.
- High Blood Pressure – Increased pressure in the arteries, which can strain the heart.
5. Kidney-Related Symptoms
Finally, hypercalcemia can impact kidney function, resulting in:
- Increased Thirst – A constant feeling of needing to drink more fluids.
- Frequent Urination – Needing to urinate more often than usual.
If you or someone you know is experiencing these symptoms, it is essential to consult a healthcare professional for proper evaluation and treatment. 🩺
Symptoms of Supravalvar Aortic Stenosis
Supravalvar aortic stenosis (SVAS) is a rare congenital heart defect that involves narrowing of the aorta just above the aortic valve. This condition can lead to various symptoms, particularly as the severity of the stenosis increases. Here are some key symptoms to be aware of:
1. Heart-Related Symptoms
Individuals with SVAS may experience several heart-related symptoms, including:
- Chest Pain – Discomfort or pain in the chest, especially during physical activity.
- Shortness of Breath – Difficulty breathing, particularly during exertion.
- Fatigue – Unusual tiredness, even with minimal activity.
2. Symptoms in Infants and Children
In infants and young children, symptoms may manifest differently. Parents should look for:
- Poor Feeding – Difficulty in feeding or a lack of interest in food.
- Failure to Thrive – Not gaining weight or growing as expected.
- Rapid Breathing – Increased respiratory rate, which may indicate distress.
3. Symptoms Related to Blood Flow
As the condition progresses, symptoms related to blood flow may become apparent:
- Cold Extremities – Hands and feet may feel unusually cold due to reduced blood flow.
- Weak Pulse – A diminished pulse in the arms or legs.
4. Other Associated Symptoms
In some cases, individuals may experience additional symptoms, such as:
- Heart Murmur – An abnormal sound heard during a heartbeat, often detected during a physical exam.
- High Blood Pressure – Elevated blood pressure readings, particularly in the arms.
Recognizing these symptoms early can lead to timely intervention and management of supravalvar aortic stenosis. If you suspect that you or a loved one may be experiencing these symptoms, it is crucial to seek medical advice promptly. ❤️

Causes of Hypercalcemia
Hypercalcemia, characterized by elevated levels of calcium in the blood, can arise from various underlying conditions and lifestyle factors. Understanding these causes is crucial for effective diagnosis and treatment. Here are some of the primary causes of hypercalcemia:
1. Primary Hyperparathyroidism
One of the most common causes of hypercalcemia is primary hyperparathyroidism. This condition occurs when one or more of the parathyroid glands become overactive, leading to excessive production of parathyroid hormone (PTH). PTH regulates calcium levels in the body, and its overproduction can result in increased calcium release from bones, enhanced intestinal absorption, and reduced renal excretion of calcium.
2. Malignancies
Certain types of cancer can lead to hypercalcemia, particularly those that metastasize to the bones, such as breast, lung, and multiple myeloma. These cancers can cause bone resorption, releasing calcium into the bloodstream. Additionally, some tumors can produce substances that mimic PTH, further elevating calcium levels.
3. Vitamin D Overdose
Excessive intake of vitamin D can lead to hypercalcemia by increasing intestinal absorption of calcium. This is often seen in individuals taking high doses of vitamin D supplements without medical supervision. It’s essential to monitor vitamin D levels to avoid this complication.
4. Granulomatous Diseases
Conditions such as sarcoidosis and tuberculosis can cause hypercalcemia due to the production of calcitriol (the active form of vitamin D) by macrophages in granulomas. This leads to increased calcium absorption from the gut and elevated serum calcium levels.
5. Medications
Some medications can contribute to hypercalcemia. For example, thiazide diuretics can reduce calcium excretion in the urine, leading to higher blood calcium levels. Additionally, lithium, used for bipolar disorder, can affect parathyroid function and calcium metabolism.
6. Dehydration
Dehydration can lead to a relative increase in calcium concentration in the blood. When the body is dehydrated, the kidneys conserve water, which can inadvertently concentrate calcium levels. Ensuring adequate hydration is vital for maintaining normal calcium levels.
7. Other Endocrine Disorders
Conditions such as hyperthyroidism and adrenal insufficiency can also lead to hypercalcemia. In hyperthyroidism, increased bone turnover can release calcium into the bloodstream, while adrenal insufficiency can disrupt calcium metabolism.
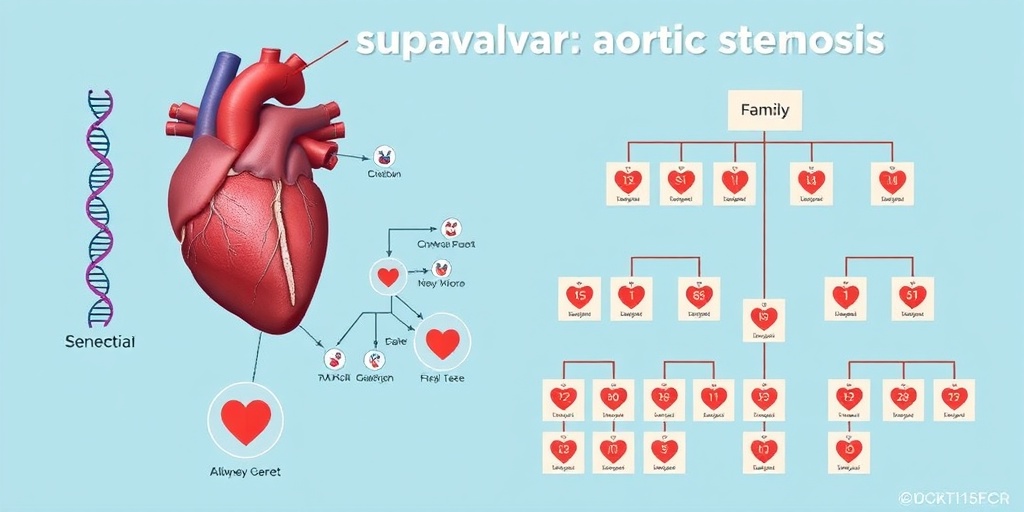
Causes of Supravalvar Aortic Stenosis
Supravalvar aortic stenosis (SVAS) is a rare congenital heart defect characterized by a narrowing of the aorta just above the aortic valve. Understanding the causes of SVAS is essential for early diagnosis and management. Here are the primary causes:
1. Genetic Factors
SVAS is often associated with genetic syndromes, particularly Williams syndrome. This genetic disorder is caused by a deletion of genetic material on chromosome 7 and is characterized by cardiovascular abnormalities, including SVAS. Genetic counseling may be beneficial for families with a history of this condition.
2. Congenital Heart Defects
In some cases, SVAS can occur as an isolated defect or in conjunction with other congenital heart defects. These may include coarctation of the aorta or other structural abnormalities that affect blood flow and pressure in the heart and vessels.
3. Environmental Factors
While the exact environmental factors contributing to SVAS are not well understood, certain maternal conditions during pregnancy, such as diabetes or exposure to teratogenic substances, may increase the risk of congenital heart defects, including SVAS.
4. Familial Patterns
There is evidence suggesting that SVAS can run in families, indicating a potential hereditary component. If a child is diagnosed with SVAS, it may be advisable for family members to undergo screening for similar conditions.
5. Other Syndromic Associations
SVAS can also be associated with other syndromes, such as Alagille syndrome and Turner syndrome. These syndromes may present with a range of symptoms, including heart defects, and require comprehensive management strategies.
Understanding the causes of both hypercalcemia and supravalvar aortic stenosis is crucial for effective diagnosis and treatment. If you or someone you know is experiencing symptoms related to these conditions, it is essential to consult a healthcare professional for proper evaluation and management. 🩺
Diagnosis of Hypercalcemia
Hypercalcemia, characterized by elevated levels of calcium in the blood, can lead to various health issues, including kidney stones, bone pain, and even cardiovascular problems. Diagnosing hypercalcemia involves a combination of clinical evaluation, laboratory tests, and imaging studies.
Clinical Evaluation
The first step in diagnosing hypercalcemia is a thorough clinical evaluation. Healthcare providers will typically start by reviewing the patient’s medical history and conducting a physical examination. Key symptoms to look out for include:
- Fatigue: Persistent tiredness that doesn’t improve with rest.
- Nausea and vomiting: Gastrointestinal disturbances can be common.
- Increased thirst and urination: Hypercalcemia can lead to dehydration.
- Bone pain: Elevated calcium levels can affect bone density.
Laboratory Tests
Once hypercalcemia is suspected, laboratory tests are essential for confirmation. The primary test is a serum calcium test, which measures the total calcium level in the blood. If hypercalcemia is confirmed, further tests may include:
- Ionized calcium test: This measures the active form of calcium in the blood.
- Parathyroid hormone (PTH) test: Helps determine if the parathyroid glands are functioning properly.
- Vitamin D levels: To assess if vitamin D is contributing to elevated calcium levels.
- Kidney function tests: To evaluate how well the kidneys are filtering calcium.
Imaging Studies
In some cases, imaging studies may be necessary to identify the underlying cause of hypercalcemia. These can include:
- X-rays: To check for bone abnormalities or fractures.
- CT scans: To visualize organs and detect tumors that may be causing elevated calcium levels.
- Bone scans: To assess bone metabolism and identify any lesions.
Understanding the diagnosis of hypercalcemia is crucial for effective treatment. By identifying the underlying cause, healthcare providers can tailor a management plan that addresses the specific needs of the patient. 🩺
Diagnosis of Supravalvar Aortic Stenosis
Supravalvar aortic stenosis (SVAS) is a rare congenital heart defect characterized by a narrowing of the aorta just above the aortic valve. Diagnosing SVAS typically involves a combination of clinical assessment, imaging techniques, and sometimes genetic testing.
Clinical Assessment
The diagnosis of SVAS often begins with a clinical assessment, where healthcare providers look for specific symptoms and risk factors. Common signs and symptoms may include:
- Heart murmur: An abnormal sound heard during a heartbeat, often detected during a routine examination.
- Chest pain: Discomfort or pain in the chest, especially during physical activity.
- Shortness of breath: Difficulty breathing, particularly during exertion.
- Fatigue: Unusual tiredness, especially in children during play.
Imaging Techniques
Imaging studies play a crucial role in diagnosing SVAS. The following techniques are commonly used:
- Echocardiogram: This ultrasound test provides detailed images of the heart’s structure and function, allowing doctors to visualize the narrowing of the aorta.
- Cardiac MRI: Magnetic resonance imaging can offer a comprehensive view of the heart and blood vessels, helping to assess the severity of the stenosis.
- Chest X-ray: While not definitive, it can reveal changes in the heart’s size and shape.
Genetic Testing
In some cases, especially if there is a family history of congenital heart defects, genetic testing may be recommended. This can help identify any underlying genetic syndromes associated with SVAS, such as Williams syndrome. Understanding the genetic factors can provide valuable insights into the patient’s condition and potential treatment options.
Diagnosing supravalvar aortic stenosis is essential for determining the appropriate management and treatment strategies. Early detection can significantly improve outcomes and quality of life for those affected. ❤️

Frequently Asked Questions about Hypercalcemia-Supravalvar Aortic Stenosis
What is Hypercalcemia-Supravalvar Aortic Stenosis?
Hypercalcemia-Supravalvar Aortic Stenosis is a rare condition characterized by elevated calcium levels in the blood, which can lead to the narrowing of the aorta just above the heart valve. This condition can affect blood flow and may lead to various cardiovascular complications.
What are the symptoms of Hypercalcemia-Supravalvar Aortic Stenosis?
Symptoms may vary, but common signs include:
- Chest pain or discomfort
- Shortness of breath
- Dizziness or fainting
- Fatigue during physical activity
Can calcium supplements cause aortic stenosis?
There is ongoing research regarding the relationship between calcium supplements and aortic stenosis. While some studies suggest a potential link, it is essential to consult with a healthcare provider before making any changes to calcium intake.
How can I reduce calcium levels in the aorta?
Reducing calcium levels in the aorta typically involves managing underlying conditions and lifestyle changes. Some strategies may include:
- Adopting a heart-healthy diet
- Regular exercise
- Medication as prescribed by a healthcare professional
Is aortic calcification the same as aortic stenosis?
Aortic calcification refers to the buildup of calcium deposits in the aorta, while aortic stenosis is the narrowing of the aortic valve opening. Although they are related, they are not the same condition. Aortic calcification can contribute to the development of aortic stenosis.
What is severe calcific aortic stenosis?
Severe calcific aortic stenosis is a condition where the aortic valve becomes significantly narrowed due to calcium buildup, leading to restricted blood flow from the heart. This can result in serious health issues and often requires medical intervention.
What should I do if I experience symptoms of aortic stenosis?
If you experience symptoms such as chest pain, shortness of breath, or dizziness, it is crucial to seek medical attention promptly. Early diagnosis and treatment can significantly improve outcomes.
Are there any specific tests for diagnosing Hypercalcemia-Supravalvar Aortic Stenosis?
Diagnosis typically involves a combination of physical examinations, imaging tests such as echocardiograms, and blood tests to assess calcium levels. Your healthcare provider will determine the most appropriate tests based on your symptoms and medical history.
Can lifestyle changes help manage Hypercalcemia-Supravalvar Aortic Stenosis?
Yes, lifestyle changes can play a significant role in managing this condition. Maintaining a balanced diet, engaging in regular physical activity, and avoiding smoking can help improve overall cardiovascular health.
Where can I find support for Hypercalcemia-Supravalvar Aortic Stenosis?
Support groups and online communities can provide valuable resources and emotional support for individuals and families affected by Hypercalcemia-Supravalvar Aortic Stenosis. Consider reaching out to healthcare providers for recommendations on local or online support networks.




