“`html
What Is Sarcoidosis?
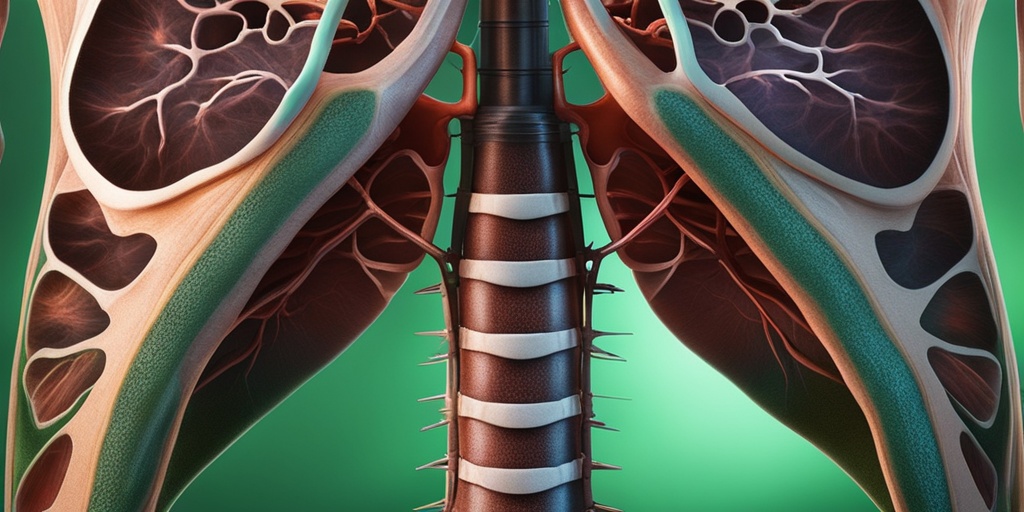
Sarcoidosis is a complex inflammatory disease that primarily affects the lungs, but it can also impact other organs such as the skin, heart, and lymph nodes. This condition is characterized by the formation of tiny clumps of inflammatory cells, known as granulomas, which can disrupt normal organ function. While the exact cause of sarcoidosis remains unknown, it is believed to involve a combination of genetic and environmental factors.
The disease can occur in anyone, but it is most commonly diagnosed in adults between the ages of 20 and 40. Interestingly, sarcoidosis is more prevalent among African Americans compared to Caucasians, and it tends to be more severe in women than in men.
Understanding the Granulomas
Granulomas are the hallmark of sarcoidosis. These small clusters of immune cells form as a response to an unknown trigger, which may include infections, allergens, or even certain chemicals. When these granulomas accumulate in various organs, they can lead to inflammation and damage, resulting in a range of symptoms.
Types of Sarcoidosis
Sarcoidosis can be classified into different types based on the organs affected:
- Sarcoidosis of the Lung: The most common form, affecting respiratory function.
- Sarcoidosis of the Skin: Characterized by rashes, lesions, or nodules on the skin.
- Cardiac Sarcoidosis: Involves the heart and can lead to serious complications.
- Neurosarcoidosis: Affects the nervous system, potentially causing neurological symptoms.
Sarcoidosis Symptoms
The symptoms of sarcoidosis can vary widely depending on the organs involved and the severity of the disease. Some individuals may experience mild symptoms, while others may face significant health challenges. Here are some common symptoms associated with sarcoidosis:
Respiratory Symptoms
Since sarcoidosis often affects the lungs, respiratory symptoms are among the most common:
- Persistent Cough: A dry cough that does not go away.
- Shortness of Breath: Difficulty breathing, especially during physical activity.
- Chest Pain: Discomfort or pain in the chest area.
Skin Symptoms
Sarcoidosis can manifest on the skin in various ways:
- Rashes: Red or purple patches on the skin.
- Nodules: Raised bumps that can be painful or itchy.
- Changes in Skin Color: Areas of skin may become darker or lighter.
Other Symptoms
In addition to respiratory and skin symptoms, sarcoidosis can affect other systems in the body:
- Fatigue: A common complaint among those with sarcoidosis.
- Fever: Low-grade fever may occur.
- Joint Pain: Inflammation in the joints can lead to discomfort.
- Vision Problems: In some cases, sarcoidosis can affect the eyes, leading to blurred vision or sensitivity to light.
When to Seek Medical Advice
If you experience any of these symptoms, especially if they persist or worsen, it is crucial to consult a healthcare professional. Early diagnosis and treatment can significantly improve outcomes and quality of life for individuals with sarcoidosis.
For more detailed information and resources on sarcoidosis, consider visiting Yesil Health AI, where you can find evidence-based health answers tailored to your needs. 🌟
In conclusion, understanding sarcoidosis is essential for recognizing its symptoms and seeking timely medical intervention. Whether it affects the lungs, skin, or other organs, being informed can empower you to manage this condition effectively.
“`
“`html
Sarcoidosis Causes
Sarcoidosis is a complex inflammatory disease that can affect multiple organs in the body, most commonly the lungs. While the exact causes of sarcoidosis remain unclear, researchers believe that a combination of genetic, environmental, and immune system factors may play a role in its development.
Genetic Factors
Genetics can significantly influence the likelihood of developing sarcoidosis. Studies have shown that individuals with a family history of the disease are at a higher risk. Specific genes related to the immune response may predispose certain individuals to sarcoidosis, suggesting that hereditary factors could be involved.
Environmental Triggers
Environmental factors are also thought to contribute to the onset of sarcoidosis. Some potential triggers include:
- Inhaled substances: Exposure to certain dust, chemicals, or biological agents may initiate an inflammatory response.
- Infections: Some researchers suggest that viral or bacterial infections could trigger sarcoidosis in genetically susceptible individuals.
- Occupational exposures: Certain professions, such as those involving firefighting or working in healthcare, may increase exposure to potential triggers.
Immune System Response
The immune system plays a crucial role in sarcoidosis. It is believed that an abnormal immune response to an unknown antigen leads to the formation of granulomas—small clusters of inflammatory cells. These granulomas can accumulate in various organs, causing symptoms and complications associated with the disease.
Sarcoidosis Risk Factors
Understanding the risk factors for sarcoidosis can help in identifying individuals who may be more susceptible to the disease. While anyone can develop sarcoidosis, certain factors increase the likelihood of its occurrence.
Age and Gender
Sarcoidosis can affect individuals of any age, but it is most commonly diagnosed in adults between the ages of 20 and 40. Additionally, women are more likely to develop sarcoidosis than men, although the reasons for this disparity are not fully understood.
Ethnicity
Ethnicity also plays a significant role in the prevalence of sarcoidosis. The disease is more common in individuals of African descent compared to Caucasians and is less frequently seen in Asian populations. This suggests that genetic predisposition may be a contributing factor.
Geographic Location
Geographic factors can influence the incidence of sarcoidosis. For instance, the disease is more prevalent in certain regions, such as the United States and Northern Europe. Environmental exposures unique to these areas may contribute to the higher rates of sarcoidosis.
Other Health Conditions
Individuals with certain health conditions may also be at a higher risk for developing sarcoidosis. These conditions include:
- Autoimmune diseases: People with autoimmune disorders may have an altered immune response, increasing their susceptibility.
- Chronic infections: Ongoing infections can potentially trigger an inflammatory response that leads to sarcoidosis.
In summary, while the exact causes of sarcoidosis remain elusive, a combination of genetic, environmental, and immune system factors likely contributes to its development. Recognizing the risk factors associated with sarcoidosis can aid in early detection and management of the disease. If you suspect you may be at risk, it’s essential to consult with a healthcare professional for further evaluation and guidance. 🩺
“`

“`html
Sarcoidosis Diagnosis
Sarcoidosis is a complex inflammatory disease that can affect various organs in the body, most commonly the lungs. Diagnosing sarcoidosis can be challenging due to its wide range of symptoms and the fact that it can mimic other conditions. Here, we will explore the diagnostic process for sarcoidosis, including the tests and evaluations that healthcare professionals typically use.
Understanding the Symptoms
The first step in diagnosing sarcoidosis often involves recognizing its symptoms. Common sarcoidosis symptoms include:
- Persistent cough
- Shortness of breath
- Fatigue
- Fever
- Weight loss
- Skin lesions or rashes
Because these symptoms can overlap with other diseases, a thorough evaluation is essential.
Medical History and Physical Examination
Your healthcare provider will begin with a detailed medical history and a physical examination. They will ask about your symptoms, any previous health issues, and family history of autoimmune diseases. During the physical exam, they may check for swollen lymph nodes or skin lesions, which can be indicative of sarcoidosis.
Diagnostic Tests
To confirm a diagnosis of sarcoidosis, several tests may be conducted:
- Chest X-ray: This is often the first imaging test performed. It can reveal enlarged lymph nodes or lung involvement.
- CT Scan: A more detailed imaging test that provides a clearer picture of the lungs and other organs.
- Biopsy: A definitive diagnosis often requires a biopsy of affected tissue. This can be done through various methods, including bronchoscopy or skin biopsy.
- Pulmonary Function Tests: These tests measure how well your lungs are working and can help assess the impact of sarcoidosis on lung function.
- Blood Tests: These can help rule out other conditions and check for markers of inflammation.
Specialist Consultation
In some cases, your primary care physician may refer you to a specialist, such as a pulmonologist or a dermatologist, depending on the symptoms you present. Sarcoidosis specialists have the expertise to interpret complex cases and recommend appropriate management strategies.
Sarcoidosis Treatment Options
Once diagnosed, the next step is to discuss sarcoidosis treatment options. Treatment can vary significantly based on the severity of the disease, the organs involved, and the symptoms experienced by the patient.
Observation and Monitoring
In many cases, especially when symptoms are mild, doctors may recommend a “watchful waiting” approach. This involves regular monitoring without immediate treatment, as sarcoidosis can sometimes resolve on its own. Regular follow-ups are crucial to ensure that the condition does not worsen.
Medications
If treatment is necessary, several medication options are available:
- Corticosteroids: These are the most common treatment for sarcoidosis. Prednisone is often prescribed to reduce inflammation and suppress the immune response.
- Immunosuppressants: In cases where corticosteroids are ineffective or cause significant side effects, medications like methotrexate or azathioprine may be used.
- Biologics: Newer treatments, such as infliximab, target specific pathways in the immune system and may be beneficial for some patients.
Supportive Therapies
In addition to medications, supportive therapies can help manage symptoms:
- Physical Therapy: This can help improve lung function and overall physical health.
- Oxygen Therapy: For patients with significant lung involvement, supplemental oxygen may be necessary.
- Nutrition and Lifestyle Changes: A balanced diet and regular exercise can support overall health and well-being.
When to Consider Advanced Treatments
In rare cases where sarcoidosis severely affects organ function, more advanced treatments may be necessary. This could include:
- Organ Transplant: For patients with severe lung or heart involvement, a transplant may be considered.
- Clinical Trials: Participating in clinical trials can provide access to new therapies that are not yet widely available.
Understanding your treatment options is crucial for managing sarcoidosis effectively. Always consult with your healthcare provider to determine the best approach for your specific situation. 🌟
“`

“`html
Sarcoidosis Complications
Sarcoidosis is a complex inflammatory disease that can affect multiple organs in the body. While many individuals may experience mild symptoms or even remain asymptomatic, others may face serious complications. Understanding these potential complications is crucial for effective management and treatment.
Common Complications of Sarcoidosis
Some of the most common complications associated with sarcoidosis include:
- Pulmonary Complications: The lungs are the most frequently affected organs in sarcoidosis. Pulmonary sarcoidosis can lead to chronic cough, shortness of breath, and even pulmonary fibrosis, which is a scarring of lung tissue that can severely impact lung function.
- Cardiac Sarcoidosis: This occurs when granulomas form in the heart, potentially leading to arrhythmias, heart failure, or other serious cardiovascular issues. Symptoms may include chest pain, palpitations, or fainting spells.
- Neurological Complications: Neuro-sarcoidosis can affect the nervous system, leading to symptoms such as headaches, seizures, or changes in mental status. This can be particularly challenging to diagnose and manage.
- Ocular Complications: Sarcoidosis can cause eye problems, including uveitis, which can lead to vision loss if not treated promptly. Symptoms may include redness, pain, and blurred vision.
- Skin Complications: Skin lesions are common in sarcoidosis, presenting as red or purple bumps, often on the face, arms, or legs. These can be itchy or painful and may require dermatological treatment.
Long-term Effects of Sarcoidosis
While many individuals with sarcoidosis may experience a remission of symptoms, others may face long-term effects. Chronic lung disease, for instance, can significantly impact quality of life and may require ongoing medical care. Additionally, the psychological impact of living with a chronic condition can lead to anxiety and depression, making it essential to address mental health alongside physical health.
Monitoring and Management
Regular follow-ups with healthcare providers are vital for monitoring potential complications. This may include:
- Routine Imaging: Chest X-rays or CT scans can help assess lung involvement and detect any changes over time.
- Cardiac Evaluations: For those at risk of cardiac sarcoidosis, regular heart monitoring may be necessary.
- Neurological Assessments: If neurological symptoms arise, a neurologist may conduct tests to evaluate brain and nerve function.
Early detection and intervention can significantly improve outcomes and quality of life for individuals living with sarcoidosis.
Sarcoidosis: Living with the Condition
Living with sarcoidosis can be a unique journey, filled with challenges and triumphs. Understanding the condition and finding effective coping strategies can empower individuals to lead fulfilling lives despite the diagnosis.
Understanding Your Diagnosis
Receiving a diagnosis of sarcoidosis can be overwhelming. It’s essential to educate yourself about the disease, including its symptoms, potential complications, and treatment options. Knowledge is power, and being informed can help you make better decisions regarding your health.
Building a Support System
Having a strong support system is crucial for anyone living with a chronic illness. This can include:
- Family and Friends: Open communication with loved ones about your condition can foster understanding and support.
- Support Groups: Connecting with others who have sarcoidosis can provide emotional support and practical advice. Online forums and local support groups can be invaluable resources.
- Healthcare Team: Regular check-ins with your healthcare providers, including specialists, can help manage symptoms and monitor for complications.
Managing Symptoms and Treatment
Effective management of sarcoidosis often involves a combination of medication and lifestyle changes. Common treatments may include:
- Corticosteroids: These are often the first line of treatment to reduce inflammation.
- Immunosuppressants: In some cases, medications that suppress the immune system may be necessary.
- Lifestyle Modifications: Regular exercise, a balanced diet, and stress management techniques can help improve overall well-being.
Emotional and Mental Health
Living with a chronic condition like sarcoidosis can take a toll on mental health. It’s important to prioritize emotional well-being by:
- Seeking Professional Help: Therapy or counseling can provide coping strategies and emotional support.
- Practicing Mindfulness: Techniques such as meditation and yoga can help reduce stress and improve mental clarity.
- Staying Connected: Engaging in social activities and hobbies can enhance your mood and provide a sense of normalcy.
By taking proactive steps to manage both the physical and emotional aspects of sarcoidosis, individuals can lead fulfilling lives and navigate the challenges of this condition with resilience. 🌟
“`

“`html
Frequently Asked Questions about Sarcoidosis
What is Sarcoidosis?
Sarcoidosis is a systemic disease characterized by the formation of tiny clumps of inflammatory cells, known as granulomas, in various organs of the body. It most commonly affects the lungs, skin, and lymph nodes.
What are the common symptoms of Sarcoidosis?
The symptoms of sarcoidosis can vary widely depending on the organs involved. Common symptoms include:
- Fatigue
- Shortness of breath
- Persistent cough
- Skin rashes or lesions
- Joint pain
How is Sarcoidosis diagnosed?
Diagnosis of sarcoidosis typically involves a combination of:
- Medical history review
- Physical examination
- Imaging tests such as X-rays or CT scans
- Biopsy of affected tissue
Can Sarcoidosis affect the heart?
Yes, sarcoidosis can affect the heart, leading to a condition known as cardiac sarcoidosis. This can result in arrhythmias, heart failure, or other serious complications.
What is the treatment for Sarcoidosis?
Treatment for sarcoidosis may not be necessary for everyone, as some individuals may experience spontaneous remission. However, for those who require treatment, options may include:
- Corticosteroids to reduce inflammation
- Immunosuppressive medications for more severe cases
- Regular monitoring of symptoms and organ function
Is there a specific diet for Sarcoidosis patients?
While there is no specific diet for sarcoidosis, maintaining a healthy diet rich in fruits, vegetables, whole grains, and lean proteins can support overall health and immune function.
Where can I find specialists for Sarcoidosis?
It is advisable to consult with a pulmonologist or a specialist in autoimmune diseases for comprehensive care and management of sarcoidosis. They can provide tailored treatment plans based on individual needs.
Can Sarcoidosis be cured?
Currently, there is no known cure for sarcoidosis, but many individuals can manage their symptoms effectively with appropriate treatment and lifestyle adjustments.
What should I do if I suspect I have Sarcoidosis?
If you suspect you have sarcoidosis or are experiencing symptoms, it is important to consult a healthcare professional for an accurate diagnosis and appropriate management.
“`




