“`html
What Is Eczema?
Eczema, also known as atopic dermatitis, is a chronic skin condition that causes inflammation, redness, and irritation. It is most commonly seen in children but can occur at any age. The exact cause of eczema is not fully understood, but it is believed to be linked to a combination of genetic and environmental factors. People with eczema often have a compromised skin barrier, which makes their skin more susceptible to irritants and allergens.
Types of Eczema
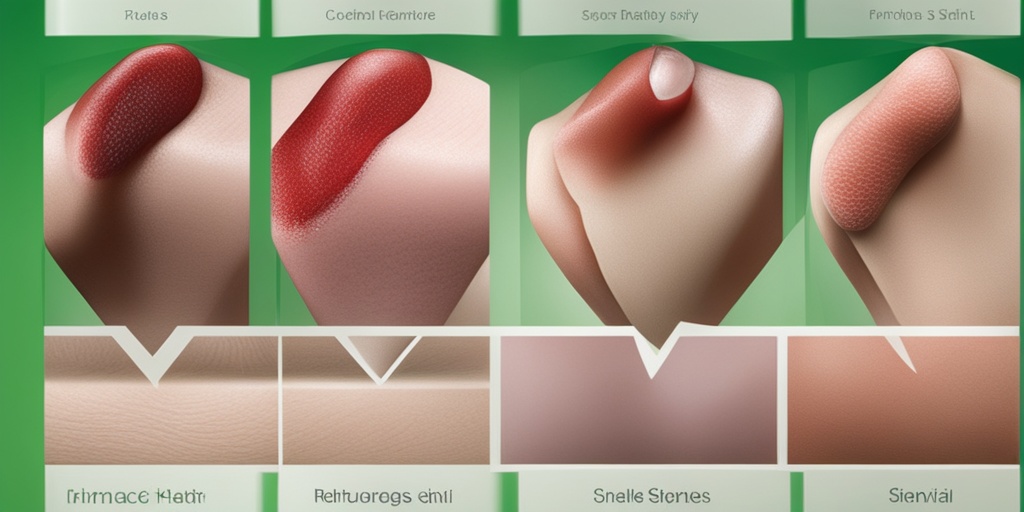
There are several types of eczema, each with its own characteristics:
- Atopic Dermatitis: The most common form, often associated with allergies and asthma.
- Contact Dermatitis: Caused by direct contact with irritants or allergens.
- Dyshidrotic Eczema: Characterized by small, itchy blisters on the hands and feet.
- Nummular Eczema: Appears as circular, coin-shaped spots on the skin.
- Seborrheic Dermatitis: Often affects oily areas of the body, such as the scalp and face.
- Stasis Dermatitis: Occurs when fluid builds up in the legs due to poor circulation.
Understanding Eczema Triggers
Identifying and avoiding triggers is crucial for managing eczema. Common triggers include:
- Environmental factors (pollution, weather changes)
- Allergens (pollen, pet dander, dust mites)
- Skin irritants (soaps, detergents, fabrics)
- Stress and anxiety
- Hormonal changes
Eczema Symptoms
The symptoms of eczema can vary from person to person and may change over time. Common symptoms include:
1. Dry, Sensitive Skin
Individuals with eczema often experience dry skin that can feel tight and sensitive. This dryness can lead to further irritation and discomfort.
2. Red, Inflamed Patches
Inflammation is a hallmark of eczema. Affected areas may appear red and swollen, particularly during flare-ups.
3. Itching
Itching is one of the most distressing symptoms of eczema. It can be intense and persistent, leading to scratching that exacerbates the condition.
4. Rash
Eczema rashes can appear anywhere on the body but are commonly found on the face, hands, and inside the elbows and knees. The rash may ooze or crust over, especially if scratched.
5. Thickened, Scaly Skin
Over time, chronic scratching can lead to thickened, leathery skin, a condition known as lichenification. This can make the skin appear darker and feel rough to the touch.
6. Eczema Herpeticum
In some cases, eczema can lead to a secondary infection known as eczema herpeticum, caused by the herpes simplex virus. This condition requires immediate medical attention and is characterized by painful blisters.
Managing Eczema Symptoms
While there is no cure for eczema, various treatments can help manage symptoms effectively. Options include:
- Moisturizers: Regularly applying eczema creams and lotions can help maintain skin hydration.
- Topical Steroids: These can reduce inflammation and itching during flare-ups.
- Antihistamines: These may help alleviate itching, especially at night.
- Phototherapy: Light therapy can be beneficial for severe cases.
- Medications: In some cases, systemic medications may be prescribed.
For personalized advice and evidence-based health answers, consider visiting Yesil Health AI. They provide valuable resources for managing eczema and other health conditions.
Understanding eczema and its symptoms is the first step toward effective management. If you or someone you know is struggling with eczema, seeking professional advice can lead to a tailored treatment plan that improves quality of life. 🌟
“`
“`html
Eczema Types
Eczema, also known as atopic dermatitis, is a common skin condition that can manifest in various forms. Understanding the different types of eczema is crucial for effective management and treatment. Here are the most prevalent types:
1. Atopic Dermatitis
This is the most common form of eczema, often starting in childhood. It is characterized by dry, itchy skin and can be triggered by environmental factors, allergens, or stress. Atopic dermatitis can appear anywhere on the body but is frequently found on the face, inside the elbows, and behind the knees.
2. Contact Dermatitis
Contact dermatitis occurs when the skin reacts to a specific substance, such as soaps, detergents, or metals. There are two types:
- Irritant Contact Dermatitis: Caused by direct damage to the skin from irritants.
- Allergic Contact Dermatitis: Triggered by an allergic reaction to a substance.
Symptoms include redness, itching, and swelling in the affected area.
3. Dyshidrotic Eczema
This type of eczema primarily affects the hands and feet, leading to small, itchy blisters. Dyshidrotic eczema can be triggered by stress, seasonal allergies, or exposure to certain metals like nickel.
4. Nummular Eczema
Nummular eczema presents as circular, coin-shaped patches on the skin. It often occurs after skin injuries, such as cuts or insect bites, and can be exacerbated by dry skin.
5. Seborrheic Dermatitis
6. Stasis Dermatitis
This type occurs in the lower legs due to poor circulation and fluid buildup. Stasis dermatitis can lead to swelling, redness, and itching, often requiring treatment for underlying venous issues.
Eczema Causes
The exact cause of eczema remains unclear, but several factors contribute to its development. Understanding these causes can help in managing and preventing flare-ups.
1. Genetic Factors
Individuals with a family history of eczema, allergies, or asthma are more likely to develop the condition. Genetic mutations affecting the skin barrier can lead to increased susceptibility to irritants and allergens.
2. Environmental Triggers
Various environmental factors can trigger eczema flare-ups, including:
- Weather Changes: Extreme temperatures, humidity, and dry air can exacerbate symptoms.
- Allergens: Pollen, pet dander, dust mites, and mold are common allergens that can trigger eczema.
- Irritants: Soaps, detergents, and certain fabrics can irritate sensitive skin.
3. Stress
Emotional stress can significantly impact eczema. Stress may lead to increased inflammation and worsen symptoms, creating a cycle that can be challenging to break.
4. Hormonal Changes
Many women report flare-ups during hormonal changes, such as menstruation or pregnancy. These fluctuations can affect skin sensitivity and exacerbate eczema symptoms.
5. Immune System Dysfunction
Individuals with eczema often have an overactive immune response to allergens and irritants. This dysfunction can lead to chronic inflammation and skin barrier impairment, making the skin more susceptible to infections.
6. Food Allergies
In some cases, food allergies can trigger eczema, particularly in children. Common allergens include dairy, eggs, nuts, and wheat. Identifying and avoiding these foods can help manage symptoms.
Understanding the types and causes of eczema is essential for effective treatment and management. By identifying triggers and working with healthcare professionals, individuals can find relief and improve their quality of life. 🌟
“`
“`html
Eczema Risk Factors
Eczema, also known as atopic dermatitis, is a chronic skin condition that can cause significant discomfort and distress. Understanding the risk factors associated with eczema is crucial for prevention and management. Here are some key factors that may increase the likelihood of developing eczema:
Genetic Predisposition
One of the most significant risk factors for eczema is a family history of the condition. If your parents or siblings have eczema, asthma, or hay fever, you may be more likely to develop eczema yourself. This genetic link suggests that certain individuals may inherit a tendency to develop skin conditions.
Environmental Factors
Environmental triggers can play a substantial role in the onset and exacerbation of eczema. Common environmental factors include:
- Climate: Extreme temperatures, humidity, and dry air can irritate the skin.
- Allergens: Exposure to allergens such as pollen, pet dander, and dust mites can trigger flare-ups.
- Pollution: Air pollution and exposure to harsh chemicals can worsen eczema symptoms.
Skin Barrier Dysfunction
Individuals with eczema often have a compromised skin barrier, which makes their skin more susceptible to irritants and allergens. This dysfunction can lead to increased moisture loss and dryness, further aggravating the condition.
Age
Eczema can occur at any age, but it is most commonly diagnosed in infants and young children. While many children outgrow eczema, some may continue to experience symptoms into adulthood. Understanding your age-related risk can help in managing the condition effectively.
Stress and Emotional Factors
Stress is a well-known trigger for many skin conditions, including eczema. Emotional stress can lead to increased inflammation and worsen existing symptoms. Finding effective stress management techniques, such as mindfulness or yoga, can be beneficial for those with eczema.
Food Allergies
Food allergies can also contribute to eczema flare-ups, particularly in children. Common allergens include:
- Milk
- Eggs
- Peanuts
- Soy
- Wheat
If you suspect that food allergies may be affecting your eczema, consult with a healthcare professional for appropriate testing and guidance.
Eczema Diagnosis
Diagnosing eczema typically involves a thorough evaluation by a healthcare professional. Here’s what you can expect during the diagnosis process:
Medical History Review
Your doctor will begin by taking a detailed medical history, including:
- Your symptoms and their duration
- Family history of eczema or other allergic conditions
- Any known triggers or irritants
Physical Examination
A physical examination of your skin will be conducted to assess the extent and severity of the eczema rash. The doctor will look for characteristic signs of eczema, such as:
- Red, inflamed patches of skin
- Dry, scaly areas
- Thickened skin from chronic scratching
Patch Testing
If your doctor suspects that allergens may be contributing to your eczema, they may recommend patch testing. This involves applying small amounts of various allergens to your skin to see if a reaction occurs. This can help identify specific triggers that you should avoid.
Skin Biopsy
In some cases, a skin biopsy may be necessary to rule out other skin conditions that can mimic eczema, such as psoriasis or fungal infections. A small sample of skin is taken and examined under a microscope to confirm the diagnosis.
Allergy Testing
For individuals with suspected food allergies, your doctor may recommend allergy testing. This can help determine if certain foods are triggering your eczema symptoms, allowing for better management of the condition.
Understanding the risk factors and the diagnosis process for eczema is essential for effective management and treatment. If you suspect you have eczema or are experiencing symptoms, consult with a healthcare professional for personalized advice and treatment options. 🌟
“`

“`html
Eczema Treatment Options
Eczema, also known as atopic dermatitis, is a chronic skin condition that can cause significant discomfort and distress. Fortunately, there are various eczema treatment options available to help manage symptoms and improve skin health. Understanding these options can empower you to make informed decisions about your care.
Topical Treatments
Topical treatments are often the first line of defense against eczema. These include:
- Corticosteroid Creams: These are anti-inflammatory medications that can reduce redness and itching. They come in various strengths, so it’s essential to follow your doctor’s recommendations.
- Calcineurin Inhibitors: Medications like tacrolimus and pimecrolimus help reduce inflammation without the side effects associated with steroids.
- Moisturizers: Keeping the skin hydrated is crucial. Look for thick creams or ointments that lock in moisture, especially after bathing.
Oral Medications
For more severe cases of eczema, oral medications may be necessary. These can include:
- Antihistamines: These can help alleviate itching, especially at night.
- Systemic Corticosteroids: Short-term use of oral steroids can help control severe flare-ups.
- Immunosuppressants: Medications like cyclosporine can be prescribed for chronic eczema that doesn’t respond to other treatments.
Phototherapy
Phototherapy, or light therapy, involves exposing the skin to controlled amounts of natural or artificial light. This treatment can be effective for moderate to severe eczema and is usually administered in a clinical setting.
Biologics
In recent years, biologic medications have emerged as a promising treatment for eczema. These are targeted therapies that can help manage symptoms by modulating the immune system. Dupilumab (Dupixent) is one such biologic that has shown significant efficacy in treating moderate to severe eczema.
Eczema Home Remedies
In addition to medical treatments, many people find relief from eczema symptoms through home remedies. These natural approaches can complement traditional treatments and help soothe irritated skin.
Moisturizing Techniques
Keeping the skin moisturized is vital for managing eczema. Here are some effective techniques:
- Oatmeal Baths: Colloidal oatmeal can soothe itchy skin. Add it to a lukewarm bath and soak for 15-20 minutes.
- Natural Oils: Coconut oil and sunflower oil are excellent for locking in moisture. Apply them directly to the skin after bathing.
- Humidifiers: Using a humidifier in your home can help maintain moisture in the air, preventing skin from drying out.
Dietary Considerations
Some individuals find that certain foods can trigger their eczema flare-ups. Keeping a food diary can help identify potential allergens. Consider incorporating:
- Anti-Inflammatory Foods: Foods rich in omega-3 fatty acids, such as salmon and flaxseeds, can help reduce inflammation.
- Probiotics: Yogurt and fermented foods may support gut health, which can positively impact skin conditions.
Natural Remedies
Several natural remedies have been reported to help with eczema symptoms:
- Honey: Known for its antibacterial properties, honey can help soothe and heal the skin.
- Aloe Vera: This plant is famous for its soothing properties and can be applied directly to the skin.
- Chamomile: Chamomile tea bags can be used as a compress to calm irritated skin.
Stress Management
Stress can exacerbate eczema symptoms, so incorporating stress-reducing techniques into your routine can be beneficial. Consider practices such as:
- Meditation: Mindfulness and meditation can help reduce stress levels.
- Yoga: Gentle yoga can promote relaxation and improve overall well-being.
- Deep Breathing Exercises: Simple breathing techniques can help calm the mind and body.
By exploring both medical treatments and home remedies, individuals with eczema can find a comprehensive approach to managing their condition. Remember, it’s essential to consult with a healthcare professional before starting any new treatment or remedy to ensure it’s appropriate for your specific situation. 🌿
“`

“`html
Frequently Asked Questions
What is the best treatment for eczema?
The best treatment for eczema often varies from person to person. Common options include:
- Topical creams and ointments to reduce inflammation.
- Moisturizers to keep the skin hydrated.
- Oral medications for severe cases.
- Phototherapy for chronic conditions.
Can eczema be cured?
Currently, there is no definitive cure for eczema, but many treatments can help manage symptoms effectively. Regular skincare routines and avoiding triggers can significantly improve the condition.
What are common triggers for eczema flare-ups?
Common triggers include:
- Environmental factors like pollen and dust mites.
- Skin irritants such as soaps and detergents.
- Stress and anxiety.
- Weather changes, particularly dry or cold conditions.
Is eczema contagious?
No, eczema is not contagious. It is a chronic skin condition that results from a combination of genetic and environmental factors.
How can I treat eczema on my face?
For eczema on the face, it is crucial to use gentle, fragrance-free products. Consider the following:
- Use a mild cleanser and avoid harsh scrubs.
- Apply a thick moisturizer regularly.
- Consult a dermatologist for appropriate topical treatments.
What is eczema herpeticum?
Eczema herpeticum is a viral infection that occurs when the herpes simplex virus infects skin that is already affected by eczema. It can cause painful blisters and requires prompt medical attention.
Can diet affect eczema symptoms?
Yes, certain foods may trigger or worsen eczema symptoms in some individuals. An anti-inflammatory diet rich in fruits, vegetables, and omega-3 fatty acids may help manage symptoms. It’s advisable to keep a food diary to identify potential triggers.
What is the role of honey in treating eczema?
Honey has natural antibacterial and anti-inflammatory properties, making it a popular home remedy for eczema. Applying honey to affected areas may help soothe the skin and promote healing.
Are there any specific creams recommended for eczema?
There are many creams available for eczema, including:
- Hydrocortisone cream for reducing inflammation.
- Emollient creams to lock in moisture.
- Prescription creams for more severe cases.
What should I do if my eczema flares up?
If you experience a flare-up, consider the following steps:
- Apply a thick moisturizer immediately.
- Use topical treatments as prescribed.
- Avoid known triggers and irritants.
- Consult your healthcare provider if symptoms worsen.
Can children get eczema?
Yes, eczema is common in children, often appearing in infancy. Many children outgrow it, but some may continue to experience symptoms into adulthood.
“`