What Is APLS?
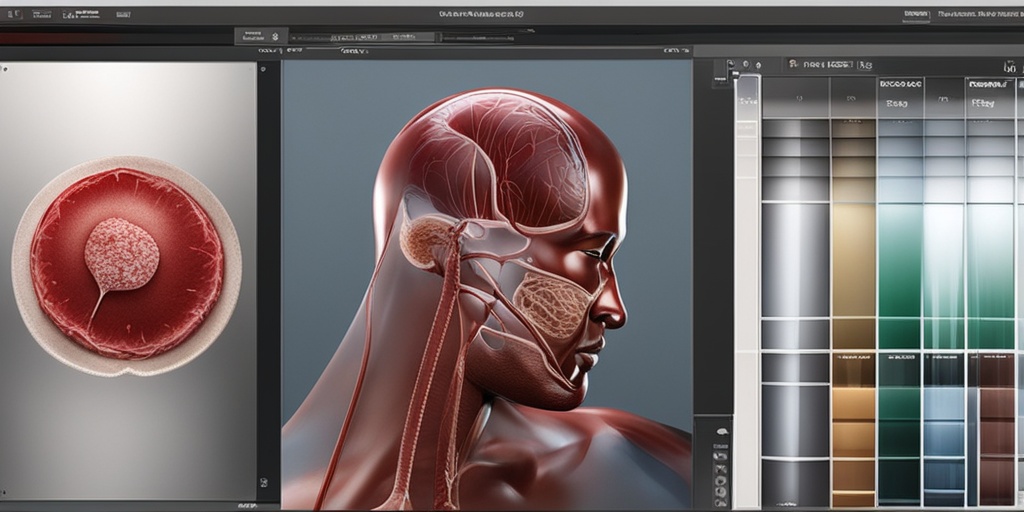
APLS, short for Antiphospholipid Syndrome, is a rare autoimmune disorder that affects the blood clotting process. In APLS, the immune system mistakenly produces antibodies that attack phospholipids, a type of fat found in cell membranes. This can lead to the formation of blood clots, which can cause a range of symptoms and complications.
What Causes APLS?
The exact cause of APLS is still unknown, but research suggests that it may be triggered by a combination of genetic and environmental factors. Some people may be more prone to developing APLS due to their genetic makeup, while others may be triggered by certain infections, medications, or other environmental factors.
How Is APLS Diagnosed?
Diagnosing APLS can be challenging, as the symptoms can be similar to those of other conditions. A diagnosis is typically made through a combination of physical examination, medical history, and laboratory tests. These tests may include blood tests to detect the presence of antiphospholipid antibodies, as well as imaging tests to rule out other conditions.
APLS Symptoms
APLS symptoms can vary widely from person to person, and may include:
- Blood clots: APLS can cause blood clots to form in the veins and arteries, which can lead to a range of complications, including stroke, heart attack, and pulmonary embolism.
- Recurrent miscarriage: Women with APLS may experience recurrent miscarriage, as the antibodies can attack the placenta and prevent the fetus from developing properly.
- Thrombocytopenia: APLS can cause a low platelet count, which can increase the risk of bleeding.
- Neurological symptoms: Some people with APLS may experience neurological symptoms, such as seizures, headaches, and cognitive impairment.
- Rash and skin lesions: APLS can cause a range of skin symptoms, including rash, skin lesions, and livedo reticularis (a net-like pattern of blood vessels).
If you’re experiencing any of these symptoms, it’s essential to speak with a healthcare professional for proper diagnosis and treatment. Remember, APLS is a complex condition that requires personalized care and attention.
For more information on APLS and other health topics, be sure to check out Yesil Health AI, a valuable resource for evidence-based health answers. 🏥
Stay tuned for the next part of this article, where we’ll explore APLS treatment options and management strategies! 💊
APLS Causes and Risk Factors
APLS, or Antiphospholipid Syndrome, is a complex autoimmune disorder that can lead to blood clots, pregnancy complications, and other serious health issues. While the exact causes of APLS are still not fully understood, research has identified several risk factors that can increase an individual’s likelihood of developing the condition.
Genetic Predisposition
Studies have shown that APLS can run in families, suggesting a possible genetic link. If you have a family history of APLS or other autoimmune disorders, you may be more likely to develop the condition. However, it’s essential to note that APLS can occur in individuals without a family history, and genetic predisposition is just one of many potential risk factors.
Infections and Environmental Triggers
Certain infections, such as Lyme disease, syphilis, and HIV, have been linked to the development of APLS. Additionally, environmental toxins, like pesticides and heavy metals, may also play a role in triggering the condition. It’s thought that these triggers can stimulate the immune system to produce antiphospholipid antibodies, which can lead to APLS.
Hormonal Imbalance
Hormonal fluctuations, particularly in women, can increase the risk of developing APLS. For example, women with polycystic ovary syndrome (PCOS) or those taking hormone replacement therapy (HRT) may be more likely to develop the condition.
Other Medical Conditions
Certain medical conditions, such as lupus, rheumatoid arthritis, and thyroid disorders, can increase the risk of developing APLS. Additionally, individuals with a history of blood clots, stroke, or heart attack may also be more likely to develop the condition.
APLS Diagnosis
Diagnosing APLS can be challenging, as the symptoms can be similar to those of other conditions. However, a combination of clinical evaluation, laboratory tests, and imaging studies can help healthcare providers diagnose APLS.
Clinical Evaluation
A healthcare provider will typically start by conducting a thorough medical history and physical examination to identify any signs or symptoms of APLS, such as blood clots, pregnancy complications, or neurological symptoms.
Laboratory Tests
Several laboratory tests can help diagnose APLS, including:
- Antiphospholipid antibody tests: These tests measure the levels of antiphospholipid antibodies in the blood, which can indicate the presence of APLS.
- Complete Blood Count (CBC): A CBC can help identify any abnormalities in blood cell counts, which can be indicative of APLS.
- Coagulation studies: These tests can help identify any abnormalities in blood clotting, which can be a sign of APLS.
Imaging Studies
Imaging studies, such as ultrasound, CT scans, or MRI, can help identify any blood clots or other complications associated with APLS.
🔍 Remember, diagnosing APLS requires a comprehensive approach that involves clinical evaluation, laboratory tests, and imaging studies. If you suspect you or a loved one may have APLS, consult with a healthcare provider to determine the best course of action.

APLS Treatment Options
When it comes to APLS (Antiphospholipid Syndrome), treatment options vary depending on the severity of the condition and the individual’s overall health. The primary goal of treatment is to prevent blood clots from forming and reduce the risk of complications. In this section, we’ll explore the different treatment options available for APLS.
Medications
Medications play a crucial role in managing APLS. The most commonly prescribed medications include:
- Anticoagulants: These medications, such as warfarin or heparin, help prevent blood clots from forming. They’re often prescribed for individuals with a history of blood clots or those at high risk of developing them.
- Antiplatelet agents: These medications, such as aspirin or clopidogrel, help prevent platelets from clumping together and forming blood clots.
- Corticosteroids: These medications, such as prednisone, can help reduce inflammation and prevent tissue damage.
Therapies
In addition to medications, various therapies can help manage APLS symptoms and prevent complications. These include:
- Physical therapy: Regular exercise and physical therapy can help improve circulation, reduce stiffness, and enhance overall mobility.
- Occupational therapy: This type of therapy focuses on helping individuals with APLS adapt to daily activities and maintain independence.
- Cognitive therapy: Cognitive therapy can help individuals cope with the emotional and psychological aspects of APLS.
Lifestyle Changes
In addition to medications and therapies, making lifestyle changes can help manage APLS symptoms and reduce the risk of complications. These changes include:
- Quitting smoking: Smoking can increase the risk of blood clots and worsen APLS symptoms. Quitting smoking can significantly reduce this risk.
- Maintaining a healthy weight: Excess weight can increase the risk of blood clots and other health problems. Maintaining a healthy weight through a balanced diet and regular exercise can help reduce this risk.
- Avoiding prolonged periods of immobility: Prolonged periods of sitting or lying down can increase the risk of blood clots. Taking regular breaks to stretch and move around can help reduce this risk.
APLS Home Care and Lifestyle Changes
While medical treatment is essential for managing APLS, making lifestyle changes and adapting to home care routines can significantly improve overall health and well-being. In this section, we’ll explore the importance of home care and lifestyle changes for individuals with APLS.
Home Care Routines
Establishing a daily routine can help individuals with APLS manage their symptoms and reduce the risk of complications. This includes:
- Monitoring blood pressure and heart rate: Regularly monitoring blood pressure and heart rate can help identify any changes or abnormalities.
- Taking medications as prescribed: Adhering to medication regimens is crucial for managing APLS symptoms and preventing complications.
- Practicing good wound care: Proper wound care can help prevent infections and promote healing.
Lifestyle Changes
In addition to home care routines, making lifestyle changes can help individuals with APLS manage their symptoms and improve their overall quality of life. These changes include:
- Staying hydrated: Drinking plenty of water can help prevent blood clots and reduce the risk of complications.
- Getting regular exercise: Regular exercise can help improve circulation, reduce stiffness, and enhance overall mobility.
- Managing stress: Stress can exacerbate APLS symptoms. Practicing stress-reducing techniques, such as meditation or deep breathing, can help manage stress and promote overall well-being.
By incorporating these treatment options, home care routines, and lifestyle changes into daily life, individuals with APLS can better manage their symptoms, reduce the risk of complications, and improve their overall quality of life. 💊🏥

APLS Complications and Prognosis
APLS, or Antiphospholipid Syndrome, is a chronic autoimmune disorder that can lead to various complications if left untreated or mismanaged. In this section, we’ll delve into the potential complications of APLS and discuss the prognosis for individuals diagnosed with this condition.
Complications of APLS
APLS can lead to a range of complications, some of which can be life-threatening. Some of the possible complications include:
- Recurrent miscarriages: Women with APLS are at a higher risk of experiencing recurrent miscarriages, which can be emotionally distressing and affect their reproductive health.
- Thrombosis: APLS increases the risk of thrombosis, which can lead to blood clots in the legs, lungs, or other parts of the body.
- Stroke and heart attack: The increased risk of thrombosis can also lead to stroke and heart attack, which can be fatal if not treated promptly.
- Pulmonary embolism: APLS can increase the risk of pulmonary embolism, a condition where a blood clot blocks an artery in the lungs.
- Kidney damage: APLS can cause kidney damage and even kidney failure in severe cases.
- Neurological symptoms: Some individuals with APLS may experience neurological symptoms such as seizures, headaches, and cognitive impairment.
Prognosis of APLS
The prognosis for individuals with APLS varies depending on the severity of the condition and the promptness of treatment. With proper management, many people with APLS can lead normal lives and reduce their risk of complications.
Early diagnosis and treatment can significantly improve the prognosis for individuals with APLS. Anticoagulant therapy, for example, can help reduce the risk of thrombosis and stroke. In some cases, medications such as aspirin and heparin may be prescribed to prevent blood clots.
In addition to medical treatment, lifestyle changes such as maintaining a healthy weight, exercising regularly, and quitting smoking can also help improve the prognosis for individuals with APLS.
APLS and Pregnancy
APLS can have a significant impact on pregnancy, and women with this condition require close monitoring and care to ensure a healthy pregnancy and birth.
Risks of APLS during Pregnancy
Women with APLS are at a higher risk of experiencing complications during pregnancy, including:
- Miscarriage: The risk of miscarriage is higher in women with APLS, especially in the first trimester.
- Preeclampsia: APLS increases the risk of preeclampsia, a condition characterized by high blood pressure and damage to organs such as the kidneys and liver.
- Placental abruption: APLS can cause placental abruption, a condition where the placenta separates from the uterus, which can be life-threatening for both the mother and the baby.
- Growth restriction: APLS can lead to growth restriction in the fetus, which can increase the risk of complications during delivery.
Managing APLS during Pregnancy
Women with APLS require close monitoring during pregnancy to minimize the risk of complications. This may involve:
- Regular blood tests: Regular blood tests can help monitor the levels of antiphospholipid antibodies and detect any potential complications early.
- Ultrasound monitoring: Regular ultrasound monitoring can help track the growth and development of the fetus.
- Medications: Medications such as aspirin and heparin may be prescribed to prevent blood clots and reduce the risk of complications.
- Close collaboration with healthcare providers: Women with APLS should work closely with their healthcare providers to develop a personalized plan for managing their condition during pregnancy.
By understanding the risks and complications associated with APLS during pregnancy, women can take steps to minimize their risk and ensure a healthy pregnancy and birth. 💕

Frequently Asked Questions about APLS
What does APLS stand for in medical terms? 🏥
In medical terms, APLS stands for Advanced Pediatric Life Support. It is a program that focuses on providing healthcare professionals with the skills and knowledge necessary to respond to pediatric emergencies.
What is the significance of APLS in laboratories? 🔬
In laboratory settings, APLS stands for Automated Plate Loader System. It is a device that automates the process of loading and unloading microplates, increasing efficiency and reducing manual labor.
What is the meaning of APLS in the context of shoes? 👠
In the context of shoes, APLS stands for Athletic Propulsion Labs. It is a brand that specializes in creating high-performance athletic shoes that provide superior comfort and support.
What are the criteria for APLS? 📝
The criteria for APLS vary depending on the context. In medical terms, the criteria for APLS certification include completing a training program and passing a written and practical exam. In laboratory settings, the criteria for APLS may include specifications for plate loading and unloading.
What is the difference between APLS and aplastic anemia? 🤕
APLS and aplastic anemia are two distinct terms. APLS refers to Advanced Pediatric Life Support or Automated Plate Loader System, depending on the context. Aplastic anemia, on the other hand, is a rare blood disorder characterized by the failure of the bone marrow to produce blood cells.
What does APLS mean in the context of stock? 📊
In the context of stock, APLS is the ticker symbol for Apex Labs, Inc. It is a publicly traded company that specializes in developing and commercializing innovative products.
What is the significance of APLS in 2025? 📆
The significance of APLS in 2025 is unclear, as it depends on the context. However, it is possible that APLS may refer to a specific event, conference, or milestone that is scheduled to take place in 2025.




