What Are Cutaneous T-Cell Lymphomas?
Cutaneous T-cell lymphomas (CTCLs) are a type of cancer that affects the skin. They occur when T-cells, a type of white blood cell, become cancerous and multiply uncontrollably in the skin. This can lead to a range of symptoms, including skin rashes, lesions, and tumors.
What Causes Cutaneous T-Cell Lymphomas?
The exact cause of CTCLs is still not fully understood, but research suggests that it may be linked to genetic mutations, exposure to certain chemicals, and weakened immune systems. In some cases, CTCLs may be associated with other medical conditions, such as autoimmune disorders or viral infections.
How Are Cutaneous T-Cell Lymphomas Diagnosed?
Diagnosing CTCLs typically involves a combination of physical examinations, medical history, and laboratory tests. A skin biopsy is usually performed to examine the affected skin cells under a microscope. Imaging tests, such as CT or PET scans, may also be used to check for any signs of cancer spread to other parts of the body.
Types of Cutaneous T-Cell Lymphomas
There are several subtypes of CTCLs, each with distinct characteristics and symptoms. Here are some of the most common types:
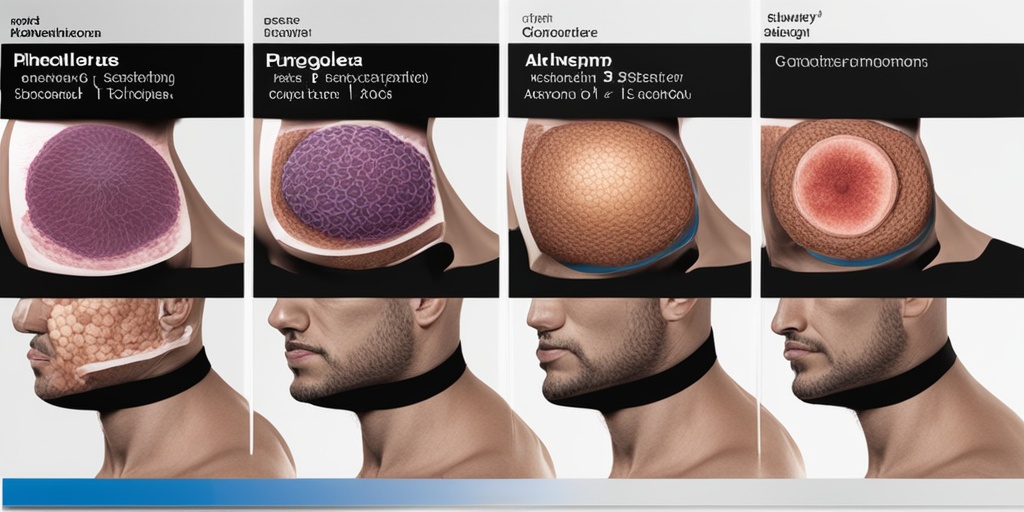
Mycosis Fungoides
This is the most common type of CTCL, accounting for about 50% of all cases. Mycosis fungoides typically starts as a skin rash or patch, which can progress to tumors and lesions over time.
Sézary Syndrome
This is a rare and aggressive type of CTCL, characterized by the presence of cancerous T-cells in the blood. Sézary syndrome often causes widespread skin lesions, as well as symptoms such as fever, weight loss, and fatigue.
Primary Cutaneous CD30-Positive Lymphoproliferative Disorders
This type of CTCL is characterized by the presence of CD30-positive cells in the skin. It often presents as a single skin lesion or a small group of lesions, which can be treated with local therapies such as radiation or surgery.
Other Types of Cutaneous T-Cell Lymphomas
There are several other subtypes of CTCLs, including lymphomatoid papulosis, primary cutaneous anaplastic large cell lymphoma, and subcutaneous panniculitis-like T-cell lymphoma. Each of these subtypes has distinct characteristics and treatment options.
It’s essential to consult a healthcare professional for an accurate diagnosis and treatment plan if you suspect you or a loved one may have CTCL. Remember, early detection and treatment can significantly improve outcomes. 💊
For more information on cutaneous T-cell lymphomas and other health topics, visit Yesil Health AI, a valuable resource for evidence-based health answers. 🌟
Cutaneous T-Cell Lymphoma Symptoms
Cutaneous T-cell lymphomas (CTCLs) are a type of cancer that affects the skin. The symptoms of CTCL can vary widely from person to person, and they may resemble those of other skin conditions. It’s essential to consult a doctor if you notice any unusual changes in your skin. Here are some common symptoms of cutaneous T-cell lymphoma:
Skin Lesions and Rashes
The most common symptom of CTCL is the appearance of skin lesions or rashes. These can take many forms, including:
- Patches: Flat, discolored areas on the skin that may be itchy or scaly.
- Plaques: Raised, thickened areas of skin that may be itchy or scaly.
- Nodules: Small, raised bumps on the skin that may be itchy or painful.
- Tumors: Large, raised growths on the skin that may be itchy, painful, or ulcerated.
These skin lesions can appear anywhere on the body, but they most commonly occur on the skin folds, such as the armpits, groin, and buttocks.
Other Symptoms
In addition to skin lesions, people with CTCL may experience:
- Fatigue: Feeling tired or weak, which can be a sign that the cancer has spread to other parts of the body.
- Fever: A high temperature that can be a sign of infection or inflammation.
- Weight loss: Losing weight without trying, which can be a sign that the cancer is advanced.
- Swollen lymph nodes: Enlarged lymph nodes in the neck, armpits, or groin, which can be a sign that the cancer has spread to the lymphatic system.
It’s essential to remember that these symptoms can also be caused by other conditions, so it’s crucial to consult a doctor for an accurate diagnosis.
Cutaneous T-Cell Lymphoma Causes and Risk Factors
While the exact causes of cutaneous T-cell lymphoma are not fully understood, there are several risk factors that may increase a person’s likelihood of developing the condition. Here are some of the known causes and risk factors:
Genetic Mutations
CTCL is caused by genetic mutations that affect the T-cells in the skin. These mutations can occur spontaneously or be inherited from one’s parents. Research suggests that certain genetic mutations, such as those affecting the STAT3 and STAT5B genes, may increase the risk of developing CTCL.
Immune System Dysfunction
People with weakened immune systems, such as those with HIV/AIDS or taking immunosuppressive medications, may be more susceptible to developing CTCL.
Environmental Factors
Exposure to certain environmental toxins, such as pesticides, herbicides, and industrial chemicals, may increase the risk of developing CTCL. However, more research is needed to confirm this link.
Age and Gender
CTCL typically affects people over the age of 50, and men are more likely to develop the condition than women.
While these risk factors may increase a person’s likelihood of developing CTCL, it’s essential to remember that anyone can develop the condition. If you’re concerned about your risk or have noticed any unusual changes in your skin, consult a doctor for an accurate diagnosis and treatment plan. 💊
How Is Cutaneous T-Cell Lymphoma Diagnosed?
Diagnosing cutaneous T-cell lymphoma (CTCL) can be a complex process, as the symptoms can be similar to those of other skin conditions. However, a combination of physical examination, medical history, and diagnostic tests can help doctors accurately diagnose CTCL.
Physical Examination
A doctor will typically start by performing a physical examination to look for any visible signs of skin lesions, rashes, or other skin abnormalities. They may also ask questions about your medical history, including any previous skin conditions, allergies, or exposure to toxins.
Diagnostic Tests
To confirm a diagnosis of CTCL, the following diagnostic tests may be ordered:
- Blood tests: Complete blood counts (CBC) and blood chemistry tests can help identify any abnormalities in the blood, such as anemia or elevated liver enzymes.
- Skin biopsy: A skin biopsy involves removing a small sample of skin tissue for examination under a microscope. This can help identify the presence of abnormal T-cells in the skin.
- Immunophenotyping: This test helps identify the specific type of T-cells present in the skin, which can aid in diagnosing CTCL.
- Molecular diagnostics: Tests such as polymerase chain reaction (PCR) or fluorescence in situ hybridization (FISH) can help identify specific genetic mutations associated with CTCL.
Staging and Classification
Once a diagnosis of CTCL is confirmed, the disease is typically staged and classified based on the severity of the symptoms and the extent of skin involvement. The most commonly used staging system for CTCL is the TNMB system, which takes into account the following factors:
- Tumor (T): The size and extent of the skin lesions.
- Node (N): The involvement of lymph nodes.
- Metastasis (M): The presence of cancer cells in other parts of the body.
- Blood (B): The presence of abnormal T-cells in the blood.
Stages of Cutaneous T-Cell Lymphoma
CTCL is typically staged from IA to IVB, with higher stages indicating more advanced disease. The stages are defined as follows:
Stage IA
Stage IA CTCL is characterized by a limited number of skin lesions, typically on the skin of the trunk or extremities. The lesions are usually small and may appear as patches, plaques, or tumors.
Stage IB
Stage IB CTCL is characterized by a larger number of skin lesions, which may be more widespread and cover a larger area of the skin.
Stage IIA
Stage IIA CTCL is characterized by the involvement of lymph nodes in addition to skin lesions. The lymph nodes may be enlarged, but the cancer has not spread to other parts of the body.
Stage IIB
Stage IIB CTCL is characterized by the presence of tumors on the skin, which may be larger and more widespread than in earlier stages.
Stage III
Stage III CTCL is characterized by the involvement of lymph nodes and the presence of abnormal T-cells in the blood.
Stage IV
Stage IV CTCL is the most advanced stage, characterized by the spread of cancer to other parts of the body, such as the liver, spleen, or lungs.
Understanding the stage and classification of CTCL is crucial in determining the most appropriate treatment plan. 💊

Cutaneous T-Cell Lymphoma Treatment Options
Cutaneous T-cell lymphoma (CTCL) is a rare type of cancer that affects the skin. While it can be challenging to treat, there are various treatment options available to manage the condition and improve the quality of life for patients. The choice of treatment depends on the severity of the disease, the location and size of the lesions, and the overall health of the patient.
Topical Treatments
For early-stage CTCL, topical treatments are often the first line of defense. These creams, gels, or ointments are applied directly to the skin to reduce inflammation and slow the growth of cancer cells. Topical corticosteroids, retinoids, and nitrogen mustard are commonly used topical treatments for CTCL.
Phototherapy
Phototherapy involves the use of ultraviolet (UV) light to treat CTCL. There are two types of phototherapy: ultraviolet B (UVB) and psoralen plus ultraviolet A (PUVA). UVB therapy uses a specific wavelength of UV light to reduce inflammation and slow the growth of cancer cells. PUVA therapy combines a medication called psoralen with UVA light to treat CTCL.
Systemic Treatments
For more advanced CTCL, systemic treatments may be necessary. These treatments are taken orally or intravenously and work to target cancer cells throughout the body. Systemic treatments for CTCL include:
- Chemotherapy: Chemotherapy drugs can be used to kill cancer cells or slow their growth.
- Immunotherapy: Immunotherapy drugs work to boost the immune system’s ability to fight cancer cells.
- Targeted therapy: Targeted therapy drugs target specific proteins or genes that contribute to the growth and survival of cancer cells.
- Biological therapy: Biological therapy uses living organisms or substances derived from living organisms to treat CTCL.
Other Treatment Options
In addition to topical, phototherapy, and systemic treatments, there are other treatment options available for CTCL. These include:
- Radiotherapy: Radiotherapy uses high-energy radiation to kill cancer cells.
- Stem cell transplantation: Stem cell transplantation involves replacing damaged bone marrow cells with healthy stem cells.
- Clinical trials: Clinical trials offer patients the opportunity to participate in research studies and access new and innovative treatments.
Living with Cutaneous T-Cell Lymphoma
While there is no cure for CTCL, it is possible to manage the condition and improve the quality of life with the right treatment and self-care strategies. Here are some tips for living with CTCL:
Self-Care Strategies
Living with CTCL can be challenging, but there are several self-care strategies that can help. These include:
- Moisturize: Keeping the skin moisturized can help reduce dryness and irritation.
- Protect your skin from the sun: Avoiding excessive sun exposure and using sunscreen can help reduce the risk of skin damage.
- Stay active: Regular exercise can help improve overall health and reduce stress.
- Join a support group: Connecting with others who have CTCL can provide emotional support and help you feel less isolated.
Managing Symptoms
CTCL can cause a range of symptoms, including skin lesions, itching, and fatigue. Here are some tips for managing symptoms:
- Keep a symptom journal: Tracking your symptoms can help you identify patterns and communicate more effectively with your healthcare team.
- Practice stress-reducing techniques: Stress can exacerbate CTCL symptoms. Practicing stress-reducing techniques like meditation or deep breathing can help.
- Get enough rest: Getting enough rest can help reduce fatigue and improve overall health.
By understanding the treatment options available and incorporating self-care strategies into your daily routine, you can improve your quality of life and manage the symptoms of CTCL. 💪

Frequently Asked Questions about Cutaneous T-Cell Lymphomas
What are Cutaneous T-Cell Lymphomas?
Cutaneous T-Cell Lymphomas (CTCLs) are a type of cancer that affects the skin and is caused by the abnormal growth of T-cells, a type of white blood cell. CTCLs are a subtype of Non-Hodgkin Lymphoma (NHL).
What are the symptoms of Cutaneous T-Cell Lymphomas?
The symptoms of CTCLs can vary depending on the stage and severity of the disease. Common symptoms include:
- Rashes or skin lesions that can appear as patches, plaques, or tumors
- Itching, burning, or stinging sensations on the skin
- Swollen lymph nodes
- Fatigue
- Weight loss
- Fever
How are Cutaneous T-Cell Lymphomas diagnosed?
Diagnosing CTCLs typically involves a combination of physical examination, medical history, and laboratory tests, including:
- Blood tests to check for abnormal T-cell counts and genetic markers
- Skin biopsies to examine skin tissue for cancerous cells
- Imaging tests, such as CT or PET scans, to check for lymph node involvement
What are the treatment options for Cutaneous T-Cell Lymphomas?
Treatment for CTCLs depends on the stage and severity of the disease, as well as the individual’s overall health. Treatment options may include:
- Topical creams or ointments to treat skin lesions
- Phototherapy, such as ultraviolet B (UVB) or psoralen plus ultraviolet A (PUVA)
- Stem cell transplantation
What is the prognosis for Cutaneous T-Cell Lymphomas?
The prognosis for CTCLs varies depending on the stage and severity of the disease. Early-stage CTCLs have a better prognosis, with a 5-year survival rate of around 80-90%. Advanced-stage CTCLs have a poorer prognosis, with a 5-year survival rate of around 30-50%.
Can Cutaneous T-Cell Lymphomas be prevented?
There is no known way to prevent CTCLs, as the exact causes of the disease are still not fully understood. However, reducing exposure to environmental toxins and maintaining a healthy immune system may help reduce the risk of developing CTCLs.
What is the latest research on Cutaneous T-Cell Lymphomas?
Researchers are continuously working to develop new and more effective treatments for CTCLs. Some of the latest research focuses on:
- Immunotherapy, such as checkpoint inhibitors and CAR-T cell therapy
- Targeted therapies, such as histone deacetylase inhibitors and proteasome inhibitors
- Stem cell transplantation and gene therapy
💡 Remember to consult a healthcare professional for personalized information and advice on Cutaneous T-Cell Lymphomas.