What Is Bacterial Meningococcal Meningitis?
Bacterial meningococcal meningitis is a serious and potentially life-threatening infection that affects the protective membranes (meninges) surrounding the brain and spinal cord. It occurs when the bacterium Neisseria meningitidis, also known as meningococcus, invades the cerebrospinal fluid and causes inflammation. This infection can progress rapidly, leading to severe complications, including brain damage, hearing loss, and even death if left untreated.
How Does Bacterial Meningococcal Meningitis Spread?
Bacterial meningococcal meningitis is highly contagious and can spread through close contact with an infected person, such as:
- Sharing food, drinks, or utensils
- Kissing or intimate contact
- Coughing or sneezing
- Living in close quarters, such as in dormitories or military barracks
It’s essential to practice good hygiene, such as washing your hands frequently, to reduce the risk of transmission.
Meningitis Symptoms in Adults and Children
The symptoms of bacterial meningococcal meningitis can vary depending on the individual, but they often develop suddenly and worsen rapidly. It’s crucial to recognize the signs and seek medical attention immediately if you or someone you know is experiencing:
Common Symptoms in Adults:
- Fever (usually high)
- Severe headache
- Stiff neck
- Vomiting or nausea
- Sensitivity to light
- Confusion or disorientation
- Seizures (in severe cases)
Common Symptoms in Children:
- Fever (usually high)
- Irritability or fussiness
- Vomiting or refusal to eat
- Stiffness or rigidity of the body
- Bulging soft spot on the top of the head (in infants)
- Seizures (in severe cases)
In addition to these symptoms, some people may experience a distinctive rash, which can appear as a cluster of small, red or purple spots or bruises on the skin. This rash can be a sign of septicemia, a life-threatening complication of bacterial meningococcal meningitis.
If you suspect someone has bacterial meningococcal meningitis, it’s essential to seek medical attention immediately. Early diagnosis and treatment can significantly improve outcomes and reduce the risk of serious complications.
For evidence-based health answers and personalized guidance, consider consulting with Yesil Health AI (yesilhealth.com), a valuable resource for accurate and reliable health information. 🏥
Remember, prompt medical attention is crucial in treating bacterial meningococcal meningitis. Don’t hesitate to seek help if you or someone you know is experiencing symptoms. ⏰

Causes and Risk Factors of Meningococcal Meningitis
Meningococcal meningitis is a serious and potentially life-threatening infection caused by the bacterium Neisseria meningitidis. Understanding the causes and risk factors of this disease is crucial for prevention and early detection.
What Causes Meningococcal Meningitis?
Meningococcal meningitis occurs when the bacterium Neisseria meningitidis infects the protective membranes surrounding the brain and spinal cord, known as the meninges. This bacterium is commonly found in the nose and throat of healthy individuals, but it can become harmful when it enters the bloodstream and reaches the meninges.
The infection can spread through:
- Close contact with an infected person, such as through kissing, sharing food or drinks, or living in close quarters.
- Contaminated food and water.
- Touching contaminated surfaces and then touching one’s face or mouth.
Who Is at Risk?
Certain individuals are more susceptible to meningococcal meningitis due to various risk factors. These include:
- Infants and young children: Their immune systems are still developing, making them more vulnerable to infections.
- Teenagers and young adults: This age group is more likely to engage in behaviors that increase the risk of transmission, such as sharing food and drinks.
- People with weakened immune systems: Those with chronic illnesses, taking immunosuppressive medications, or having undergone spleen removal are more susceptible to infections.
- People living in close quarters: Such as college students, military personnel, and individuals in crowded living conditions.
- Travelers to areas with high incidence rates: Countries with high rates of meningococcal meningitis, such as sub-Saharan Africa, may pose a higher risk to travelers.
How Is Meningococcal Meningitis Diagnosed?
Diagnosing meningococcal meningitis promptly is crucial for effective treatment and preventing serious complications. Here’s how healthcare professionals diagnose this condition:
Physical Examination
A doctor will typically perform a physical examination to look for signs of meningitis, such as:
- Fever.
- Stiff neck.
- Headache.
- Vomiting.
- Rash (in some cases).
Laboratory Tests
To confirm the diagnosis, laboratory tests are necessary. These may include:
- Blood tests to check for signs of infection and inflammation.
- Lumbar puncture (spinal tap) to collect cerebrospinal fluid (CSF) for analysis.
- CSF tests to detect the presence of bacteria, such as Gram staining and bacterial culture.
Imaging Studies
In some cases, imaging studies like CT or MRI scans may be ordered to rule out other conditions or complications, such as brain edema or abscesses.
Early diagnosis and prompt treatment are critical for preventing serious complications and improving outcomes for patients with meningococcal meningitis. If you suspect you or someone else may have this condition, seek medical attention immediately! 🚑

Meningococcal Meningitis Treatment Options
Meningococcal meningitis is a serious and potentially life-threatening infection that requires prompt medical attention. The good news is that with timely and appropriate treatment, most people can recover from this condition. In this section, we’ll explore the various treatment options available for meningococcal meningitis.
Antibiotics: The First Line of Defense
The primary treatment for meningococcal meningitis is antibiotics. Ceftriaxone is the most commonly used antibiotic for this condition, and it’s usually administered intravenously in a hospital setting. Other antibiotics like cefotaxime and ampicillin may also be used, depending on the severity of the infection and the patient’s overall health.
It’s essential to start antibiotic treatment as soon as possible, as it can significantly improve outcomes and reduce the risk of complications. In fact, studies have shown that prompt antibiotic treatment can reduce the mortality rate from meningococcal meningitis by up to 70% 📊.
Supportive Care: Managing Symptoms and Complications
In addition to antibiotics, patients with meningococcal meningitis often require supportive care to manage their symptoms and prevent complications. This may include:
- Fluid management: Patients may need intravenous fluids to prevent dehydration and maintain blood pressure.
- Pain management: Medications like acetaminophen or ibuprofen may be used to reduce fever and relieve headaches.
- Oxygen therapy: In severe cases, patients may require oxygen therapy to help them breathe.
- Monitoring: Patients will need close monitoring to detect any signs of complications, such as seizures or respiratory failure.
Other Treatment Options
In some cases, additional treatment options may be necessary to manage specific complications or symptoms. These may include:
- Corticosteroids: These medications can help reduce inflammation and swelling in the brain and spinal cord.
- Anticonvulsants: Medications like phenytoin or valproate may be used to control seizures.
- Vasopressors: These medications can help increase blood pressure in patients with septic shock.
Complications of Meningococcal Meningitis
While prompt treatment can significantly improve outcomes, meningococcal meningitis can still lead to serious complications, especially if treatment is delayed or inadequate. Some of the possible complications of meningococcal meningitis include:
Septic Shock
Septic shock is a life-threatening condition that occurs when the infection causes a severe drop in blood pressure. This can lead to organ failure, respiratory distress, and even death 💀.
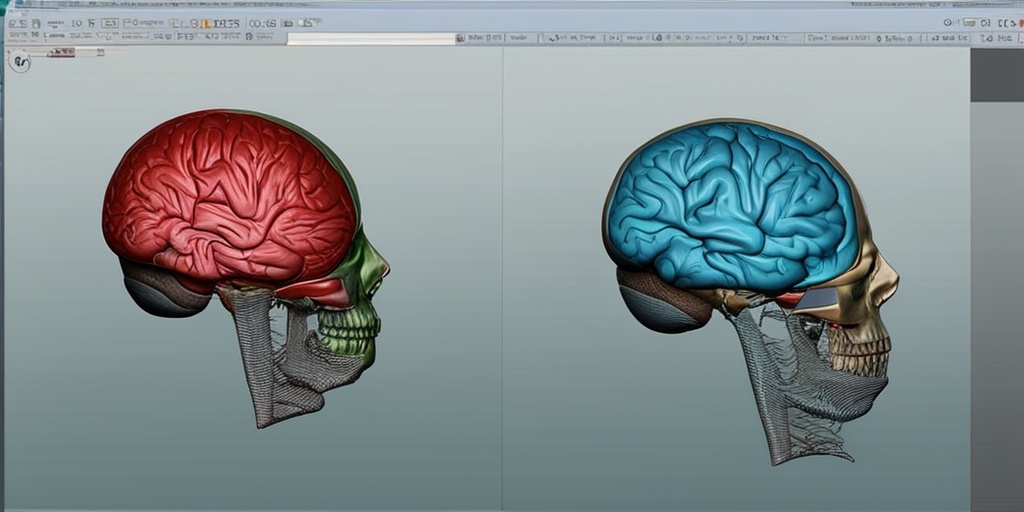
Brain Damage and Neurological Problems
Meningococcal meningitis can cause inflammation and swelling in the brain, leading to permanent brain damage, hearing loss, and neurological problems like seizures, memory loss, and cognitive impairment 🧠.
Learning and Developmental Delays
Children who survive meningococcal meningitis may experience learning and developmental delays, including speech and language difficulties, attention deficit hyperactivity disorder (ADHD), and behavioral problems 📚.
Amputations and Skin Scarring
In severe cases, meningococcal meningitis can cause skin lesions, gangrene, and amputations, especially if the infection is not treated promptly 🤕.
It’s essential to seek medical attention immediately if you suspect someone has meningococcal meningitis. Prompt treatment can significantly reduce the risk of complications and improve outcomes.

Meningococcal Meningitis Vaccination and Prevention
Meningococcal meningitis is a serious and potentially life-threatening infection that can affect anyone, but it’s most common in infants, adolescents, and young adults. The good news is that vaccination and prevention strategies can significantly reduce the risk of contracting this disease. In this section, we’ll explore the importance of vaccination and other ways to prevent meningococcal meningitis.
Vaccination: The Best Defense Against Meningococcal Meningitis
Vaccination is the most effective way to prevent meningococcal meningitis. The Centers for Disease Control and Prevention (CDC) recommends that all children receive the meningococcal conjugate vaccine (MenACWY) at 11-12 years old, with a booster dose at 16 years old. This vaccine protects against four types of meningococcal bacteria: A, C, W, and Y.
In addition to the routine vaccination schedule, the CDC also recommends vaccination for certain high-risk groups, including:
- College freshmen living in dormitories
- People with certain medical conditions, such as sickle cell disease or a weakened immune system
- Travelers to countries where meningococcal disease is common
- People who have been exposed to someone with meningococcal disease
Other Prevention Strategies
In addition to vaccination, there are other ways to reduce the risk of meningococcal meningitis:
- Avoid close contact with people who are sick, especially if they have symptoms of meningitis, such as fever, headache, and stiff neck.
- Practice good hygiene, including washing your hands frequently with soap and water, especially after coughing or sneezing.
- Avoid sharing food, drinks, or utensils with others, as this can spread the bacteria.
- Get enough sleep, exercise regularly, and manage stress to keep your immune system strong.
By following these prevention strategies and staying up-to-date on recommended vaccinations, you can significantly reduce your risk of contracting meningococcal meningitis. 🙏
Meningitis and Septicemia: What’s the Difference?
Meningitis and septicemia are two serious and potentially life-threatening infections that can occur when bacteria, such as meningococcal bacteria, enter the body. While they’re related, they’re not the same thing. Let’s explore the differences between these two conditions.
Meningitis: Inflammation of the Meninges
Meningitis is an inflammation of the meninges, the protective membranes surrounding the brain and spinal cord. When bacteria enter the body, they can cause an infection in the meninges, leading to inflammation and potentially life-threatening complications.
The symptoms of meningitis can include:
- Fever
- Headache
- Stiff neck
- Vomiting
- Sensitivity to light
- Confusion or disorientation
Septicemia: Bloodstream Infection
Septicemia, also known as blood poisoning, occurs when bacteria enter the bloodstream and cause a severe infection. This can lead to a life-threatening condition known as sepsis, which can cause organ failure and death.
The symptoms of septicemia can include:
- Fever
- Chills
- Rapid heart rate
- Shortness of breath
- Confusion or disorientation
- Nausea and vomiting
While meningitis and septicemia are two distinct conditions, they can occur together, which is known as meningococcal septicemia. This is a particularly serious and life-threatening condition that requires immediate medical attention. ⏰
Frequently Asked Questions about Bacterial Meningococcal Meningitis
What is Bacterial Meningococcal Meningitis?
Bacterial Meningococcal Meningitis is a serious and potentially life-threatening infection that occurs when the protective membranes surrounding the brain and spinal cord, known as the meninges, become inflamed. It is caused by the bacterium Neisseria meningitidis.
What are the Symptoms of Bacterial Meningococcal Meningitis?
The symptoms of Bacterial Meningococcal Meningitis can vary from person to person, but common symptoms include:
- Fever
- Headache
- Stiff neck
- Confusion or disorientation
- Seizures
- Rash (in some cases)
How is Bacterial Meningococcal Meningitis Diagnosed?
Bacterial Meningococcal Meningitis is typically diagnosed through a combination of physical examination, medical history, and laboratory tests, including:
- Lumbar puncture (spinal tap)
- Blood tests
- Imaging tests (such as CT or MRI scans)
How is Bacterial Meningococcal Meningitis Treated?
Bacterial Meningococcal Meningitis is typically treated with antibiotics, and in severe cases, hospitalization may be necessary. Early treatment is crucial to prevent serious complications and improve outcomes.
Can Bacterial Meningococcal Meningitis be Prevented?
Yes, Bacterial Meningococcal Meningitis can be prevented through vaccination. The meningococcal conjugate vaccine is recommended for all children and adolescents, and is also recommended for certain high-risk groups, such as college students and military personnel.
What is the Prognosis for Bacterial Meningococcal Meningitis?
The prognosis for Bacterial Meningococcal Meningitis varies depending on the severity of the infection and the promptness of treatment. With early treatment, most people can recover from the infection, but in severe cases, it can lead to serious complications, such as brain damage, hearing loss, and even death.
What are the Complications of Bacterial Meningococcal Meningitis?
Complications of Bacterial Meningococcal Meningitis can include:
- Brain damage
- Hearing loss
- Learning disabilities
- Seizures
- Death
How Common is Bacterial Meningococcal Meningitis?
Bacterial Meningococcal Meningitis is a relatively rare infection, but it can occur in people of all ages. According to the Centers for Disease Control and Prevention (CDC), there are approximately 1,000 to 1,200 cases of meningococcal disease reported in the United States each year.
Is Bacterial Meningococcal Meningitis Contagious?
Bacterial Meningococcal Meningitis is contagious, but only through close contact with an infected person’s respiratory secretions, such as through kissing, sharing food or drinks, or being in close proximity to someone who is coughing or sneezing.
What is the Difference between Bacterial Meningococcal Meningitis and Viral Meningitis?
Bacterial Meningococcal Meningitis is caused by a bacterial infection, while viral meningitis is caused by a viral infection. Bacterial meningitis is typically more severe and requires prompt medical attention, while viral meningitis is usually less severe and may resolve on its own.
Can I Get Bacterial Meningococcal Meningitis if I’ve Been Vaccinated?
While vaccination can provide protection against Bacterial Meningococcal Meningitis, it is not 100% effective. It is still possible to get the infection even if you’ve been vaccinated, especially if you are exposed to the bacteria through close contact with an infected person.
What Should I Do if I Think I or Someone I Know Has Bacterial Meningococcal Meningitis?
If you suspect that you or someone you know has Bacterial Meningococcal Meningitis, seek medical attention immediately. Early treatment is crucial to prevent serious complications and improve outcomes. 🚑




