What Is a Vascular Access Device?
A vascular access device (VAD) is a medical tool designed to provide access to the vascular system for various therapeutic and diagnostic purposes. These devices are crucial in healthcare settings, especially for patients requiring long-term medication administration, blood sampling, or fluid replacement. VADs facilitate the delivery of treatments directly into the bloodstream, ensuring that medications can be administered efficiently and effectively.
Vascular access devices are particularly important for patients undergoing chemotherapy, those with chronic illnesses, or individuals requiring frequent blood draws. By providing a reliable access point, VADs minimize the need for repeated needle sticks, reducing discomfort and anxiety for patients.
Why Are Vascular Access Devices Important?
The significance of vascular access devices cannot be overstated. Here are a few reasons why they are essential in modern medicine:
- Improved Patient Comfort: VADs reduce the frequency of needle insertions, which can be painful and distressing for patients.
- Enhanced Treatment Efficiency: These devices allow for quicker and more reliable administration of medications, especially in emergency situations.
- Long-Term Access: For patients requiring ongoing treatment, VADs provide a stable and secure access point.
- Reduced Risk of Complications: Properly managed VADs can lower the risk of complications such as phlebitis or infection.
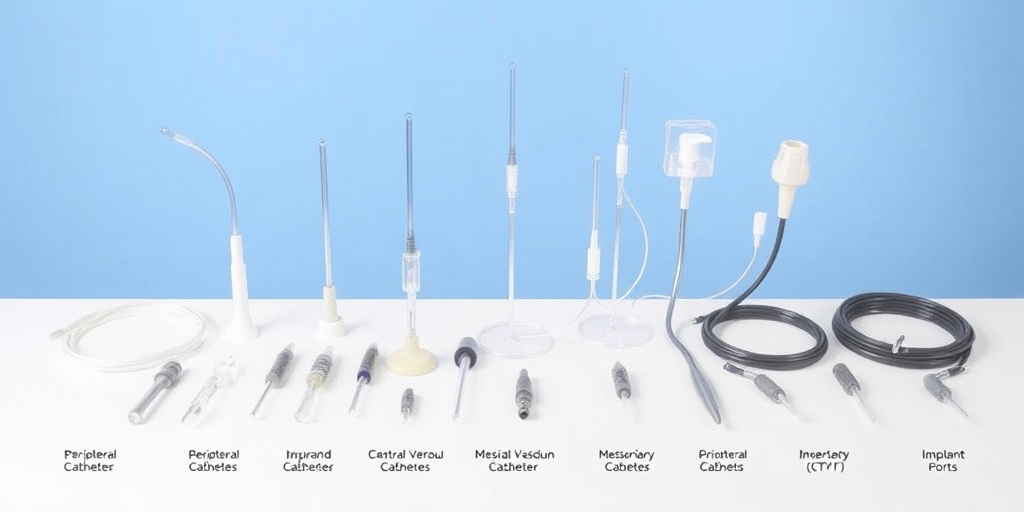
Types of Vascular Access Devices
There are several types of vascular access devices, each designed for specific medical needs and situations. Understanding these types can help healthcare providers choose the most appropriate device for their patients.
1. Peripheral Intravenous Catheters (PIVC)
Peripheral intravenous catheters are the most common type of vascular access device. They are typically inserted into a small vein in the arm or hand and are used for short-term access, usually lasting from a few days to a week. PIVCs are ideal for administering fluids, medications, and blood products.
2. Central Venous Catheters (CVC)
Central venous catheters are inserted into larger veins, often in the neck, chest, or groin. They are used for long-term access, making them suitable for patients undergoing chemotherapy or those requiring frequent blood transfusions. CVCs can remain in place for weeks to months, depending on the patient’s needs.
3. Peripherally Inserted Central Catheters (PICC)
PICC lines are a type of central venous catheter that is inserted into a peripheral vein and threaded to a central vein near the heart. They are commonly used for patients needing long-term intravenous therapy, such as antibiotics or chemotherapy. PICCs can remain in place for several weeks to months, providing a reliable access point.
4. Implantable Ports
Implantable ports are devices that are surgically placed under the skin, usually in the chest area. They consist of a small reservoir connected to a catheter that leads to a central vein. These ports are ideal for patients requiring long-term access, as they are less visible and can be accessed with a special needle when needed. They significantly reduce the risk of infection and are often used for chemotherapy patients.
5. Dialysis Access Devices
For patients with kidney failure requiring dialysis, specific vascular access devices are used, such as arteriovenous (AV) fistulas or grafts. These devices allow for efficient blood flow during dialysis treatments, ensuring that patients receive the necessary care.
Conclusion
Understanding the various types of vascular access devices is crucial for both healthcare providers and patients. Each device serves a unique purpose and is selected based on the patient’s specific medical needs. Proper management and care of these devices are essential to minimize complications and ensure effective treatment.
For more information on vascular access devices and their management, consider visiting Yesil Health AI, a valuable resource for evidence-based health answers. Whether you’re a healthcare professional or a patient, staying informed about vascular access devices can lead to better health outcomes. 🌟
Indications for Use
Vascular Access Devices (VADs) are essential tools in modern medicine, providing a reliable means for healthcare professionals to administer medications, fluids, and blood products directly into a patient’s bloodstream. Understanding the indications for use of these devices is crucial for ensuring patient safety and effective treatment. Here are some common scenarios where VADs are indicated:
1. Long-Term Medication Administration
Patients requiring long-term intravenous (IV) therapy, such as those with chronic illnesses or cancer, often benefit from VADs. These devices allow for the continuous or repeated administration of medications without the need for frequent needle sticks, which can be painful and lead to complications.
2. Nutritional Support
For patients who cannot consume food orally, VADs are used to deliver total parenteral nutrition (TPN). This method provides essential nutrients directly into the bloodstream, ensuring that patients receive the necessary calories and vitamins for recovery.
3. Blood Transfusions
VADs are crucial during blood transfusions, allowing for the safe and efficient delivery of blood products. This is particularly important in emergency situations where rapid access to the vascular system is needed.
4. Chemotherapy Administration
Patients undergoing chemotherapy often require VADs to facilitate the administration of potent medications. These devices help minimize discomfort and reduce the risk of complications associated with repeated venipunctures.
5. Dialysis Access
For patients with kidney failure, VADs are used to access the bloodstream for dialysis treatments. This is vital for removing waste products and excess fluids from the body when the kidneys are unable to perform these functions.
Insertion Procedures
The insertion of a vascular access device is a critical procedure that requires skill and precision. Understanding the various techniques and protocols involved can help ensure successful placement and minimize complications. Here’s a breakdown of the common insertion procedures for VADs:
1. Peripheral Venous Catheter Insertion
This is the most common method for short-term vascular access. A healthcare provider typically uses a small needle to insert a catheter into a peripheral vein, usually in the arm or hand. The procedure is relatively quick and can be performed at the bedside.
2. Central Venous Catheter (CVC) Insertion
CVCs are used for patients requiring long-term access. The insertion is performed in a sterile environment, often using ultrasound guidance to locate the vein accurately. The catheter is usually placed in larger veins, such as the internal jugular or subclavian vein, and can remain in place for weeks or months.
3. Peripherally Inserted Central Catheter (PICC) Line Insertion
PICC lines are a type of CVC that is inserted through a peripheral vein and advanced toward the heart. This method is ideal for patients needing extended IV therapy. The procedure is typically performed by specially trained nurses or physicians and involves the use of ultrasound for guidance.
4. Implantable Port Insertion
Implantable ports are devices placed under the skin, providing long-term access to the bloodstream. The insertion procedure is performed in a sterile surgical setting, and the port can remain in place for years. This option is particularly beneficial for patients requiring frequent blood draws or medication administration.
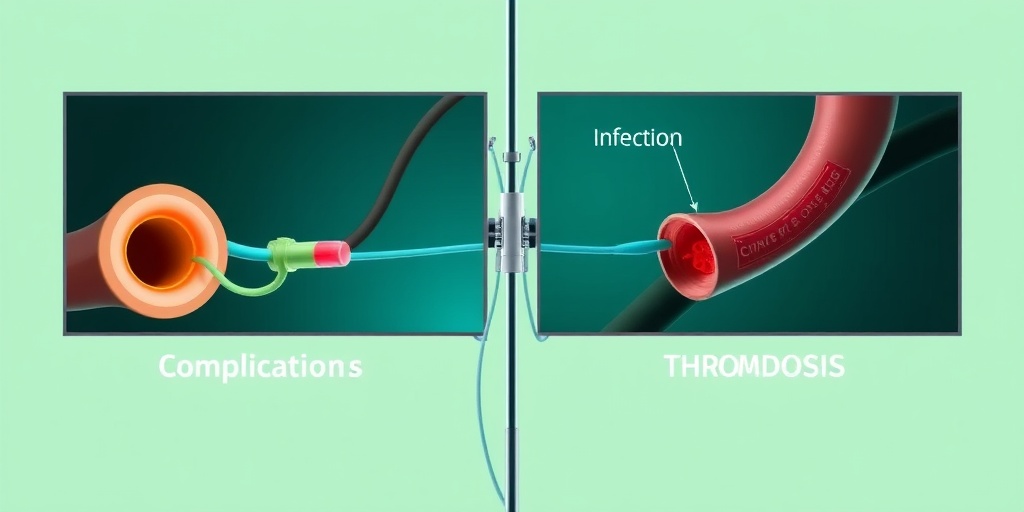
5. Complications and Management
While VAD insertion procedures are generally safe, complications can occur. Common issues include:
- Infection: Proper aseptic technique is crucial to minimize the risk of infection.
- Thrombosis: Blood clots can form around the catheter, leading to complications.
- Catheter Malposition: Ensuring correct placement is vital to avoid complications.
Healthcare providers must be vigilant in monitoring for these complications and managing them promptly to ensure patient safety and device efficacy.

Maintenance and Care
Proper maintenance and care of vascular access devices (VADs) are crucial for ensuring their effectiveness and minimizing the risk of complications. Whether you are a healthcare professional or a patient, understanding the best practices for VAD management can significantly enhance patient outcomes.
Daily Care Routine
Establishing a daily care routine is essential for maintaining the integrity of the vascular access device. Here are some key steps to follow:
- Hand Hygiene: Always wash your hands thoroughly with soap and water or use an alcohol-based hand sanitizer before handling the VAD.
- Site Inspection: Regularly inspect the insertion site for any signs of redness, swelling, or discharge. Early detection of issues can prevent more serious complications.
- Dressing Changes: Change the dressing around the VAD according to your healthcare provider’s instructions, typically every 7 days or sooner if it becomes wet or soiled.
- Flushing Protocol: Follow the flushing protocol as prescribed to maintain patency. This usually involves using a saline solution to flush the device before and after medication administration.
Long-Term Care Considerations
For patients with long-term vascular access devices, additional care considerations are necessary:
- Regular Follow-Ups: Schedule regular follow-up appointments with your healthcare provider to monitor the device and the insertion site.
- Patient Education: Educate patients and caregivers about the signs of infection and when to seek medical attention.
- Documentation: Keep a record of all care activities, including dressing changes and any issues encountered, to provide comprehensive information to healthcare providers.
Potential Complications
While vascular access devices are invaluable in medical treatment, they are not without risks. Understanding the potential complications associated with VADs can help in early detection and management.
Infection
One of the most significant risks associated with vascular access devices is infection. Infections can occur at the insertion site or systemically. Signs of infection include:
- Redness and swelling at the site
- Pain or tenderness
- Fever or chills
If any of these symptoms occur, it is crucial to contact a healthcare provider immediately. Prompt treatment can prevent the infection from spreading and causing more severe complications.
Thrombosis
Thrombosis, or the formation of a blood clot within the vascular access device, is another potential complication. Symptoms may include:
- Swelling in the arm or leg
- Pain or discomfort
- Changes in skin color
Regular flushing and monitoring can help reduce the risk of thrombosis. If a clot is suspected, medical intervention is necessary to resolve the issue.
Catheter Malposition
Occasionally, a vascular access device may become malpositioned, leading to complications such as:
- Inadequate blood flow
- Increased risk of infection
Healthcare providers should assess the position of the device during routine check-ups and take corrective measures if necessary.
Mechanical Complications
Mechanical complications, such as breakage or dislodgement of the device, can also occur. Patients should be educated on how to handle their devices carefully to minimize these risks. If a device is suspected to be damaged or dislodged, immediate medical attention is required.
In conclusion, understanding the maintenance and care of vascular access devices, along with being aware of potential complications, is vital for both patients and healthcare providers. By following best practices and being vigilant, the risks associated with VADs can be significantly reduced, leading to better health outcomes. 🌟
Patient Education
Understanding vascular access devices (VADs) is crucial for patients who may require them for medical treatments. These devices are essential for delivering medications, fluids, and nutrients directly into the bloodstream, making patient education a vital component of effective healthcare.
What is a Vascular Access Device?
A vascular access device is a medical tool used to access the vascular system. It allows healthcare providers to administer treatments without the need for repeated needle sticks. Common types of VADs include:
- Peripheral IV Catheters: Short-term access for fluids and medications.
- Central Venous Catheters (CVCs): Long-term access for patients needing frequent treatments.
- Peripherally Inserted Central Catheters (PICCs): Inserted into a peripheral vein and advanced to a central vein.
- Implantable Ports: Devices placed under the skin for long-term access.
Why is Patient Education Important?
Educating patients about their vascular access device is essential for several reasons:
- Understanding the Purpose: Patients should know why a VAD is necessary and how it will benefit their treatment.
- Awareness of Risks: Patients need to be informed about potential complications, such as infections or blood clots.
- Proper Care and Maintenance: Knowledge of how to care for the device can prevent complications and ensure its effectiveness.
- Recognizing Signs of Complications: Patients should be able to identify symptoms that require immediate medical attention.
Key Topics to Cover in Patient Education
When educating patients about their vascular access device, consider covering the following topics:
- Insertion Procedure: Explain how the device will be inserted and what to expect during the process.
- Daily Care: Provide guidelines on how to keep the site clean and monitor for signs of infection.
- Activity Restrictions: Discuss any limitations on physical activities or movements to avoid complications.
- Emergency Procedures: Inform patients about what to do if they experience issues with their device.
Utilizing visual aids, such as diagrams or videos, can enhance understanding and retention of information. Additionally, encouraging questions can help clarify any uncertainties patients may have. 🩺
Future Trends in Vascular Access Devices
The field of vascular access devices is continually evolving, driven by advancements in technology and a growing understanding of patient needs. Here are some exciting trends shaping the future of VADs:
Technological Innovations
As technology advances, so do the designs and functionalities of vascular access devices. Innovations include:
- Smart VADs: Devices equipped with sensors that monitor flow rates and detect complications in real-time.
- Biodegradable Materials: Research is underway to develop VADs made from materials that can safely dissolve in the body, reducing the need for removal.
- 3D Printing: This technology allows for the customization of VADs tailored to individual patient anatomies, improving comfort and effectiveness.
Enhanced Patient Safety
Future trends also focus on improving patient safety and reducing complications associated with VADs. Some initiatives include:
- Standardized Protocols: Developing universal guidelines for VAD insertion and maintenance to minimize infection rates.
- Training and Simulation: Enhanced training programs for healthcare providers using simulation technology to improve insertion techniques.
- Telehealth Monitoring: Utilizing telehealth platforms to monitor patients remotely, ensuring timely intervention if complications arise.
Patient-Centric Designs
As healthcare shifts towards a more patient-centered approach, the design of vascular access devices is also changing. Future devices may feature:
- Comfort-Focused Designs: Innovations aimed at reducing discomfort during insertion and throughout the duration of use.
- Cosmetic Considerations: Devices that are less visible and more aesthetically pleasing, helping patients feel more confident.
In conclusion, the future of vascular access devices looks promising, with advancements aimed at enhancing patient experience and safety. As these trends continue to develop, they will play a crucial role in improving healthcare outcomes for patients requiring vascular access. 🌟

Frequently Asked Questions about Vascular Access Devices
What is a Vascular Access Device?
A vascular access device (VAD) is a medical tool used to access the vascular system for various purposes, including administering medications, fluids, or drawing blood. These devices are essential in healthcare settings, especially for patients requiring long-term treatment.
What are the different types of Vascular Access Devices?
- Peripheral IV Catheters: Short-term access for medications and fluids.
- Central Venous Catheters (CVCs): Used for long-term access, often placed in larger veins.
- Peripherally Inserted Central Catheters (PICCs): Inserted in a peripheral vein and advanced to a central vein.
- Implantable Ports: Devices placed under the skin for easy access.
What is the purpose of a Vascular Access Device?
The primary purpose of a vascular access device is to provide a reliable route for administering medications, fluids, and nutrients, as well as for blood sampling. They are particularly useful for patients with chronic illnesses or those undergoing chemotherapy.
How is a Vascular Access Device inserted?
The insertion of a vascular access device typically involves a trained healthcare professional using sterile techniques. The procedure may vary depending on the type of device being used, but it generally includes the following steps:
- Preparation of the insertion site.
- Application of local anesthesia.
- Insertion of the device into the vein.
- Securing the device and ensuring proper placement.
What are the risks associated with Vascular Access Devices?
While vascular access devices are generally safe, there are potential risks, including:
- Infection at the insertion site.
- Blood clots.
- Damage to blood vessels or nerves.
- Device malfunction.
How should a Vascular Access Device be managed?
Proper management of a vascular access device is crucial to prevent complications. This includes:
- Regular cleaning and dressing changes.
- Monitoring for signs of infection or complications.
- Following healthcare provider instructions for use and maintenance.
What is the ICD-10 code for Vascular Access Devices?
The ICD-10 code for vascular access devices varies based on the specific type and purpose of the device. It is essential to consult the latest coding guidelines or a healthcare professional for accurate coding.
Can Vascular Access Devices be used with enteral equipment?
Yes, vascular access devices can be used in conjunction with enteral equipment, but it is important to follow specific protocols to ensure safe and effective use.
What policies govern the use of Vascular Access Devices?
Healthcare facilities typically have policies in place regarding the insertion, management, and maintenance of vascular access devices. These policies are designed to ensure patient safety and adherence to best practices.
Where can I find more information about Vascular Access Devices?
For more detailed information about vascular access devices, consult healthcare professionals, medical literature, or trusted online resources dedicated to medical education.