What Is Raynaud’s Phenomenon?
Raynaud’s Phenomenon is a medical condition that affects blood flow to certain parts of the body, primarily the fingers and toes. This phenomenon occurs when small blood vessels in these areas constrict excessively in response to cold temperatures or stress, leading to a temporary reduction in blood supply. As a result, affected areas may turn white or blue and feel cold and numb. When blood flow returns, the skin may turn red and throb as warmth returns.
There are two types of Raynaud’s: primary and secondary. Primary Raynaud’s, also known as Raynaud’s disease, occurs without any underlying health issues, while secondary Raynaud’s is associated with other medical conditions, such as autoimmune diseases like lupus or scleroderma. Understanding the differences between these two types is crucial for effective management and treatment.
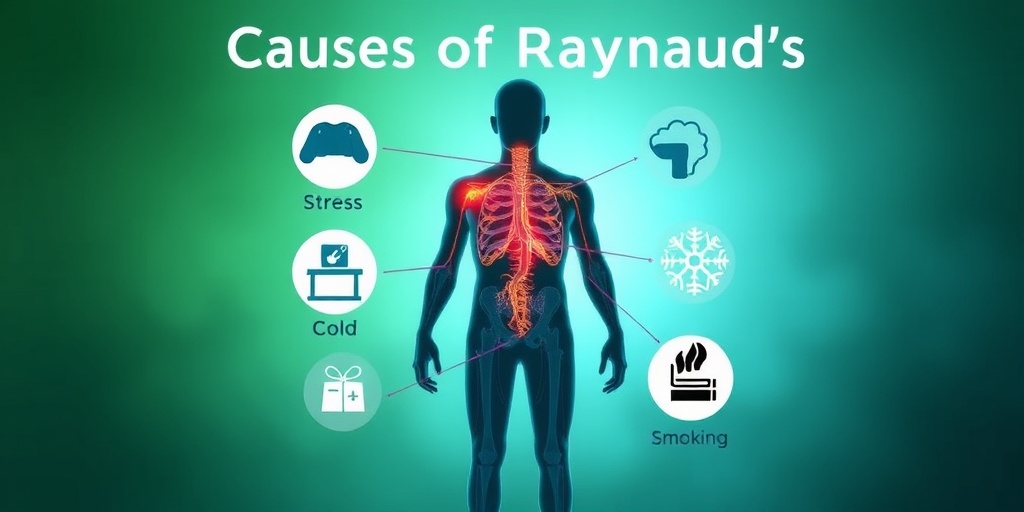
Causes of Raynaud’s Phenomenon
The exact cause of Raynaud’s Phenomenon is not fully understood, but several factors can trigger its symptoms:
- Cold temperatures: Exposure to cold weather or handling cold objects can provoke an episode.
- Stress: Emotional stress can lead to the constriction of blood vessels.
- Certain medications: Some medications, particularly those that constrict blood vessels, can exacerbate symptoms.
- Underlying health conditions: Conditions like lupus, rheumatoid arthritis, and scleroderma can lead to secondary Raynaud’s.
It’s essential to recognize these triggers to manage and prevent episodes effectively. If you suspect you have Raynaud’s Phenomenon, consulting a healthcare professional is vital for proper diagnosis and treatment options.
Raynaud’s Symptoms
The symptoms of Raynaud’s Phenomenon can vary in severity and duration. Common symptoms include:
- Color changes: Affected areas may turn white or blue during an episode, indicating reduced blood flow. Once blood flow returns, the skin may appear red.
- Coldness: Fingers and toes may feel unusually cold to the touch, especially in response to cold weather.
- Numbness or tingling: Affected areas may experience a tingling sensation or numbness during an episode.
- Pain or throbbing: As blood flow returns, individuals may experience pain or throbbing in the affected areas.
Recognizing an Episode
Episodes of Raynaud’s can last from a few minutes to several hours. They often occur in response to cold or stress, and recognizing the signs early can help in managing the condition. If you notice frequent episodes or if they become more severe, it’s crucial to seek medical advice.
When to Seek Medical Attention
While Raynaud’s Phenomenon is often manageable, there are instances when medical attention is necessary. If you experience:
- Severe pain during an episode
- Skin sores or ulcers on your fingers or toes
- Changes in skin color that last longer than usual
These symptoms may indicate a more serious underlying condition, and timely intervention can prevent complications.
For more information on Raynaud’s Phenomenon and its management, consider visiting Yesil Health AI, a valuable resource for evidence-based health answers. Understanding your condition is the first step towards effective management and improving your quality of life.
In conclusion, Raynaud’s Phenomenon is a manageable condition with proper awareness and care. By recognizing the symptoms and triggers, individuals can take proactive steps to minimize episodes and maintain a healthy lifestyle. 🌟

Types of Raynaud’s
Raynaud’s Phenomenon is a condition characterized by episodes of reduced blood flow to the fingers and toes, often triggered by cold temperatures or stress. Understanding the different types of Raynaud’s can help in managing the symptoms effectively. There are two primary types of Raynaud’s: Primary Raynaud’s and Secondary Raynaud’s.
Primary Raynaud’s
Primary Raynaud’s is the more common form and is not associated with any other underlying medical condition. It typically occurs on its own and is often less severe. Individuals with primary Raynaud’s may experience:
- Episodes of color changes in the fingers and toes (white, blue, and red).
- Coldness or numbness in the affected areas.
- Discomfort or pain during an episode.
This type is often hereditary, meaning it can run in families. While it can be uncomfortable, primary Raynaud’s usually does not lead to serious health issues.
Secondary Raynaud’s
Secondary Raynaud’s, also known as Raynaud’s disease, is less common but can be more serious. It occurs as a result of an underlying health condition, such as:
- Autoimmune diseases (e.g., lupus, scleroderma).
- Arterial diseases (e.g., atherosclerosis).
- Carpal tunnel syndrome.
- Certain medications (e.g., beta-blockers, some chemotherapy drugs).
Individuals with secondary Raynaud’s may experience more severe symptoms and complications, including skin ulcers or gangrene in extreme cases. It’s crucial for those diagnosed with secondary Raynaud’s to work closely with their healthcare provider to manage the underlying condition effectively.
Causes of Raynaud’s
The exact cause of Raynaud’s Phenomenon is not fully understood, but it is believed to be related to the narrowing of blood vessels in response to cold or stress. Here are some common factors that can contribute to the development of Raynaud’s:
Environmental Factors
Cold temperatures are the most significant trigger for Raynaud’s episodes. When exposed to cold, the body naturally constricts blood vessels to conserve heat, which can lead to reduced blood flow in the extremities. Additionally, sudden changes in temperature, such as moving from a warm environment to a cold one, can also provoke symptoms.
Emotional Stress
Stress can trigger the body’s fight-or-flight response, leading to the release of hormones that constrict blood vessels. This can result in an episode of Raynaud’s, particularly in individuals who are already predisposed to the condition.
Underlying Health Conditions
As mentioned earlier, secondary Raynaud’s is linked to various health issues. Some of the most common conditions associated with Raynaud’s include:
- Scleroderma: A chronic autoimmune disease that affects the skin and connective tissues.
- Lupus: An autoimmune disease that can affect multiple systems in the body.
- Thyroid disorders: Conditions that affect thyroid function can also influence blood flow.
Other Contributing Factors
Several other factors may increase the risk of developing Raynaud’s, including:
- Smoking: Nicotine constricts blood vessels, which can exacerbate symptoms.
- Gender: Women are more likely to develop Raynaud’s than men.
- Age: It often begins between the ages of 15 and 30.
Understanding the types and causes of Raynaud’s Phenomenon is essential for effective management and treatment. If you suspect you have Raynaud’s or are experiencing symptoms, consult with a healthcare professional for a proper diagnosis and personalized care plan. 🩺💙
Risk Factors for Raynaud’s Phenomenon
Raynaud’s Phenomenon is a condition that affects blood flow to certain parts of the body—most commonly the fingers and toes. Understanding the risk factors associated with this condition can help in early identification and management. Here are some key factors that may increase the likelihood of developing Raynaud’s:
1. Gender and Age
Women are significantly more likely to develop Raynaud’s than men. Additionally, the condition often appears in individuals aged between 15 and 30 years. However, it can occur at any age.
2. Family History
If you have a family history of Raynaud’s or other autoimmune diseases, your risk may be higher. Genetic predisposition plays a crucial role in the development of this condition.
3. Underlying Health Conditions
Certain health conditions can increase the risk of Raynaud’s Phenomenon, including:
- Autoimmune diseases: Conditions like lupus, scleroderma, and rheumatoid arthritis are commonly associated with Raynaud’s.
- Peripheral artery disease: Reduced blood flow due to narrowed arteries can trigger symptoms.
- Thyroid disorders: An underactive thyroid can contribute to circulation issues.
4. Environmental Factors
Exposure to cold temperatures is a significant trigger for Raynaud’s. Cold weather can cause blood vessels to constrict, leading to symptoms. Additionally, emotional stress can also provoke episodes.
5. Lifestyle Choices
Certain lifestyle factors can exacerbate the condition:
- Smoking: Tobacco use can constrict blood vessels and worsen circulation.
- High caffeine intake: Excessive caffeine can also lead to blood vessel constriction.
6. Occupation
Jobs that involve repetitive motions or exposure to vibrating tools (like jackhammers) can increase the risk of developing Raynaud’s. This is often referred to as vibration white finger.
Raynaud’s Diagnosis
Diagnosing Raynaud’s Phenomenon involves a combination of medical history, physical examination, and sometimes additional tests. Here’s how healthcare professionals typically approach the diagnosis:
1. Medical History
Your doctor will start by asking about your symptoms, including:
- Frequency and duration of episodes
- Triggers, such as cold exposure or stress
- Any associated symptoms, like numbness or color changes in the fingers and toes
2. Physical Examination
A thorough physical examination will be conducted to assess blood flow and check for any signs of underlying conditions. Your doctor may look for:
- Color changes in your fingers and toes during an episode
- Skin temperature differences
- Signs of other health issues, such as joint swelling or skin changes
3. Nailfold Capillaroscopy
This test involves examining the small blood vessels at the base of your fingernails under a microscope. It helps to identify any abnormalities that may indicate an underlying autoimmune condition.
4. Blood Tests
Blood tests may be ordered to check for autoimmune diseases or other conditions that could be contributing to your symptoms. Common tests include:
- Antinuclear antibody (ANA) test: This test checks for autoimmune disorders.
- Complete blood count (CBC): This helps assess overall health and detect a variety of disorders.
5. Cold Stimulation Test
In some cases, a cold stimulation test may be performed. This involves exposing your hands to cold temperatures and monitoring blood flow and color changes to assess the severity of Raynaud’s symptoms.
Understanding the risk factors and the diagnostic process for Raynaud’s Phenomenon is crucial for effective management and treatment. If you suspect you have this condition, consult a healthcare professional for a thorough evaluation and personalized care. 🌡️💙

Raynaud’s Treatment Options
Raynaud’s Phenomenon is a condition that affects blood flow to certain parts of the body—usually the fingers and toes—resulting in episodes of reduced blood flow, often triggered by cold temperatures or stress. Understanding the treatment options available can help manage symptoms effectively and improve quality of life.
Medications
Several medications can help alleviate the symptoms of Raynaud’s Phenomenon. These include:
- Calcium Channel Blockers: These medications, such as amlodipine and nifedipine, help relax and widen blood vessels, improving blood flow.
- Vasodilators: Drugs like topical nitroglycerin can be applied to the skin to help dilate blood vessels and reduce the frequency of attacks.
- Antidepressants: Certain antidepressants, particularly selective serotonin reuptake inhibitors (SSRIs), may help improve blood flow and reduce symptoms.
Lifestyle Changes
In addition to medications, making some lifestyle adjustments can significantly impact the management of Raynaud’s Phenomenon:
- Stay Warm: Dress in layers and wear gloves or warm socks when exposed to cold temperatures. Keeping your core warm can also help.
- Manage Stress: Stress can trigger episodes, so practicing relaxation techniques such as yoga, meditation, or deep breathing can be beneficial.
- Avoid Smoking: Smoking constricts blood vessels, worsening symptoms. Quitting smoking can improve circulation and overall health.
Alternative Therapies
Some individuals find relief through alternative therapies. While scientific evidence may vary, these options can be worth exploring:
- Biofeedback: This technique teaches you to control physiological functions, potentially helping to reduce the frequency of Raynaud’s attacks.
- Acupuncture: Some patients report improvement in symptoms after acupuncture treatments, which may help enhance blood flow.
- Herbal Supplements: Certain herbs, like ginkgo biloba, are thought to improve circulation, but consult with a healthcare provider before starting any supplements.
Surgical Options
In severe cases where other treatments have failed, surgical options may be considered:
- Sympathectomy: This procedure involves cutting nerves that cause blood vessels to constrict, potentially improving blood flow to affected areas.
- Digital Nerve Block: This technique can help relieve symptoms by blocking nerve signals that cause blood vessel constriction.
Living with Raynaud’s
Living with Raynaud’s Phenomenon can be challenging, but with the right strategies, individuals can lead fulfilling lives. Here are some tips to help manage the condition:
Daily Management Strategies
Incorporating daily management strategies can make a significant difference:
- Keep a Symptom Diary: Tracking your symptoms can help identify triggers and patterns, allowing for better management.
- Stay Active: Regular exercise improves circulation and can help reduce the frequency of attacks. Aim for activities that keep you warm and engaged.
- Hydration: Staying well-hydrated is essential for overall health and can help maintain good circulation.
Support and Resources
Connecting with others who understand your experience can be invaluable:
- Support Groups: Joining a support group, either in-person or online, can provide emotional support and practical advice from those who share similar experiences.
- Educational Resources: Websites and organizations dedicated to Raynaud’s Phenomenon can offer valuable information and updates on research and treatments.
Communicating with Healthcare Providers
Effective communication with your healthcare provider is crucial for managing Raynaud’s Phenomenon:
- Be Open About Symptoms: Discuss all symptoms, even those that may seem unrelated, to help your provider understand your condition better.
- Ask Questions: Don’t hesitate to ask about treatment options, lifestyle changes, and any concerns you may have regarding your condition.
By understanding Raynaud’s Phenomenon and implementing effective treatment and management strategies, individuals can navigate their daily lives with greater ease and comfort. Remember, you are not alone in this journey! 🌈

Frequently Asked Questions about Raynaud’s Phenomenon
What is Raynaud’s Phenomenon?
Raynaud’s Phenomenon is a condition that affects blood flow to certain parts of the body—usually the fingers and toes. It occurs when small blood vessels in these areas constrict excessively in response to cold or stress, leading to color changes, numbness, and discomfort.
What causes Raynaud’s Phenomenon?
The exact cause of Raynaud’s Phenomenon is not fully understood, but it can be triggered by various factors, including:
- Cold temperatures
- Emotional stress
- Certain medications
- Underlying health conditions, such as autoimmune diseases
How is Raynaud’s Phenomenon treated?
Treatment for Raynaud’s Phenomenon focuses on managing symptoms and preventing attacks. Common approaches include:
- Keeping warm in cold weather
- Avoiding stress
- Medications to improve blood flow
- Lifestyle changes, such as quitting smoking
What is the difference between Raynaud’s Phenomenon and Raynaud’s Disease?
Raynaud’s Disease is a primary form of Raynaud’s Phenomenon that occurs without any underlying health issues. In contrast, Raynaud’s Phenomenon can be secondary to other medical conditions, such as scleroderma or lupus.
Is Raynaud’s Phenomenon serious?
While Raynaud’s Phenomenon itself is usually not serious, it can lead to complications if blood flow is severely restricted for extended periods. In rare cases, it can cause skin sores or ulcers.
Can Raynaud’s Phenomenon occur without gangrene?
Yes, Raynaud’s Phenomenon can occur without gangrene. Most individuals experience symptoms like color changes and numbness without severe complications. However, it’s essential to monitor symptoms and consult a healthcare provider if they worsen.
What is the ICD-10 code for Raynaud’s Phenomenon?
The ICD-10 code for Raynaud’s Phenomenon is I73.00, which is used for billing and documentation purposes in healthcare settings.
Where can I find more information about Raynaud’s Phenomenon?
For more detailed information, you can visit reputable health websites, consult with healthcare professionals, or refer to resources provided by organizations like the NHS.




