What Are Pressure Sores?
Pressure sores, also known as bedsores or pressure ulcers, are injuries to the skin and underlying tissue that occur when there is prolonged pressure on the skin. They typically develop over bony areas of the body, such as the heels, hips, and tailbone, and can affect anyone who has limited mobility or is bedridden for extended periods. Understanding pressure sores is crucial for prevention and treatment, especially for individuals at higher risk.
How Do Pressure Sores Develop?
Pressure sores develop due to a combination of factors, including:
- Pressure: Continuous pressure on the skin reduces blood flow to the area, leading to tissue damage.
- Friction: Rubbing against clothing or bedding can damage the skin, making it more susceptible to sores.
- Shear: When the skin moves in one direction while the underlying bone moves in another, it can cause tissue to stretch and tear.
- Moisture: Excess moisture from sweat or incontinence can weaken the skin and increase the risk of sores.
Individuals with limited mobility, such as those recovering from surgery, elderly patients, or individuals with certain medical conditions, are particularly vulnerable to developing pressure sores. Recognizing the risk factors is essential for effective prevention.
Pressure Sores Symptoms
Identifying the symptoms of pressure sores early can significantly improve treatment outcomes. Here are the common signs to watch for:
Early Symptoms
In the initial stages, pressure sores may not be visible as open wounds. Instead, you might notice:
- Redness: Affected areas may appear red and feel warm to the touch.
- Discoloration: Darker skin tones may show a purplish or bluish hue.
- Skin Changes: The skin may feel different in texture, becoming softer or firmer than surrounding areas.
- Pain or Discomfort: Individuals may experience tenderness or pain in the affected area.
Advanced Symptoms
If pressure sores progress without treatment, they can develop into more severe stages, leading to:
- Open Wounds: The skin may break down, forming blisters or ulcers.
- Infection: Signs of infection include increased redness, swelling, pus, or a foul odor.
- Deep Tissue Damage: Advanced sores can extend into deeper layers of skin and muscle, causing significant pain and complications.
It’s essential to monitor any changes in the skin, especially for those at risk. If you notice any of these symptoms, seeking medical advice promptly can help prevent further complications.
Prevention and Care
Preventing pressure sores is often more effective than treating them. Here are some strategies to consider:
- Regular Position Changes: Encourage individuals to change positions every two hours to relieve pressure.
- Use Supportive Surfaces: Specialized mattresses and cushions can help distribute weight more evenly.
- Maintain Skin Hygiene: Keep the skin clean and dry to reduce moisture buildup.
- Nutrition: A balanced diet rich in vitamins and minerals supports skin health and healing.
For more detailed information on pressure sores and their management, consider visiting Yesil Health AI, a valuable resource for evidence-based health answers.
In conclusion, understanding pressure sores, their symptoms, and prevention strategies is vital for anyone at risk. By being proactive, you can help protect yourself or your loved ones from these painful injuries. Remember, early detection and intervention are key! 🌟

Causes of Pressure Sores
Pressure sores, also known as bedsores or pressure ulcers, are injuries to the skin and underlying tissue that occur when there is prolonged pressure on the skin. Understanding the causes of pressure sores is crucial for prevention and effective treatment. Here are the primary factors that contribute to the development of these painful sores:
Prolonged Pressure
The most significant cause of pressure sores is sustained pressure on a specific area of the body. This pressure restricts blood flow to the skin, leading to tissue damage. Common areas where pressure sores develop include:
- Buttocks
- Heels
- Elbows
- Shoulders
- Back of the head
Individuals who are bedridden or use a wheelchair are particularly at risk due to the constant pressure on these areas.
Friction and Shear
Friction occurs when the skin rubs against clothing or bedding, which can damage the skin and make it more susceptible to pressure sores. Shear, on the other hand, happens when the skin moves in one direction while the underlying bone moves in another. This can occur when a person slides down in bed or is pulled up without proper support. Both friction and shear can exacerbate the effects of pressure, leading to skin breakdown.
Moisture
Excess moisture from sweat, urine, or other bodily fluids can weaken the skin, making it more prone to damage. Moist skin is less resilient and can break down more easily under pressure. Maintaining skin hygiene and dryness is essential in preventing pressure sores.
Medical Conditions
Certain medical conditions can increase the risk of developing pressure sores. These include:
- Diabetes: Poor circulation and nerve damage can hinder healing.
- Vascular diseases: Conditions that affect blood flow can lead to tissue damage.
- Neurological disorders: Conditions like stroke or spinal cord injuries can impair sensation and mobility.
- Malnutrition: A lack of essential nutrients can weaken the skin and slow down healing.
Risk Factors for Pressure Sores
Identifying risk factors for pressure sores is vital for prevention, especially for individuals who may be more susceptible. Here are some key risk factors to consider:
Immobility
Individuals who are unable to move independently, whether due to surgery, illness, or disability, are at a higher risk for pressure sores. The longer a person remains in one position, the greater the risk of developing sores.
Age
Older adults are more prone to pressure sores due to thinner skin and decreased blood flow. Additionally, age-related conditions may limit mobility and sensation, increasing the risk.
Incontinence
Incontinence can lead to skin irritation and moisture, making the skin more vulnerable to pressure sores. It is essential to manage incontinence effectively to reduce this risk.
Poor Nutrition
A diet lacking in essential nutrients can impair skin health and healing. Individuals who are malnourished or dehydrated are at a higher risk for developing pressure sores. Ensuring a balanced diet rich in vitamins and minerals is crucial for skin integrity.
Medical Devices
Devices such as casts, braces, or oxygen masks can create pressure points on the skin. Regularly checking the skin under these devices is important to prevent sores from developing.
Chronic Health Conditions
Conditions such as heart disease, lung disease, and diabetes can affect circulation and healing, increasing the risk of pressure sores. Managing these conditions effectively can help reduce the risk.
By understanding the causes and risk factors of pressure sores, caregivers and individuals can take proactive steps to prevent these painful injuries. Regular skin assessments, repositioning, and maintaining skin hygiene are essential strategies in the fight against pressure sores. 🛌💪

Diagnosing Pressure Sores
Pressure sores, also known as bedsores or pressure ulcers, are injuries to the skin and underlying tissue that occur when there is prolonged pressure on the skin. They are most commonly found on areas of the body where bones are close to the skin, such as the heels, elbows, and buttocks. Early diagnosis is crucial for effective treatment and prevention of complications. Here’s how healthcare professionals diagnose pressure sores.
Identifying Symptoms
The first step in diagnosing pressure sores is recognizing the symptoms. Common signs include:
- Redness or discoloration of the skin that does not fade when pressure is relieved.
- Swelling or warmth in the affected area.
- Pain or tenderness in the area, which may be more pronounced when pressure is applied.
- Open wounds or blisters that may develop as the sore progresses.
Physical Examination
A healthcare provider will conduct a thorough physical examination to assess the affected area. They will look for:
- The size and depth of the sore.
- The condition of the surrounding skin, checking for signs of infection.
- The location of the sore, as certain areas are more prone to pressure sores.
Grading Pressure Sores
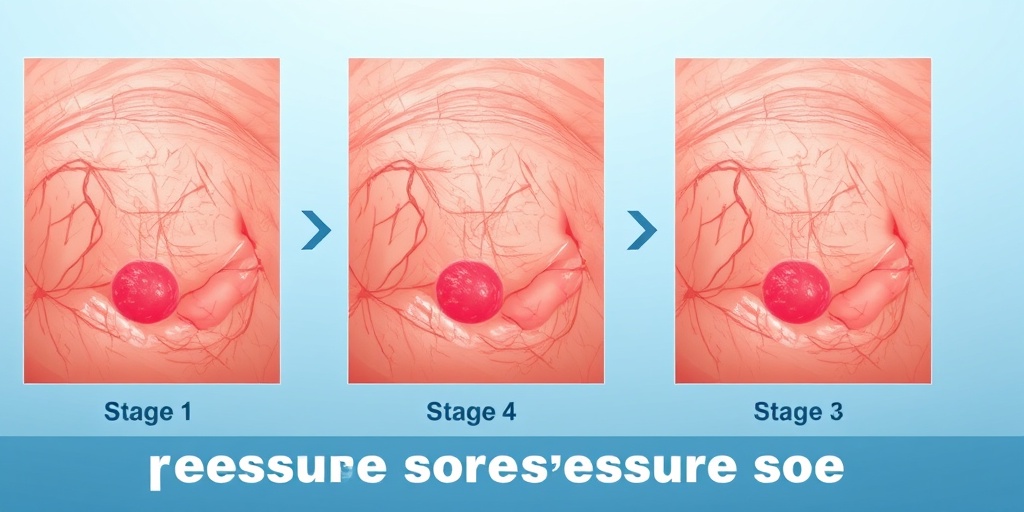
Pressure sores are graded based on their severity, which helps in determining the appropriate treatment. The grading system typically includes:
- Stage 1: Non-blanchable redness of intact skin.
- Stage 2: Partial thickness loss of skin, presenting as a shallow open ulcer.
- Stage 3: Full thickness tissue loss, with visible fat but no bone, tendon, or muscle.
- Stage 4: Full thickness tissue loss with exposed bone, tendon, or muscle.
Understanding the stages of pressure sores is essential for effective treatment and management. If you suspect you or someone you care for has a pressure sore, it’s important to seek medical attention promptly. Early intervention can significantly improve outcomes and prevent further complications. 🩺
Stages of Pressure Sores
Pressure sores progress through various stages, each indicating a different level of severity. Recognizing these stages is vital for effective treatment and prevention. Here’s a detailed look at the stages of pressure sores.
Stage 1: Non-blanchable Redness
In this initial stage, the skin appears red and does not turn white when pressed. The area may feel warm, firm, or soft compared to surrounding skin. This stage is crucial for intervention, as it indicates that the skin is at risk of further damage. Early treatment can often reverse the condition.
Stage 2: Partial Thickness Loss
At this stage, the sore has progressed to a partial thickness loss of skin. It may present as an open ulcer or a blister filled with clear fluid. The surrounding skin may be red and inflamed. Treatment at this stage focuses on keeping the area clean and protected to promote healing.
Stage 3: Full Thickness Tissue Loss
Stage 3 pressure sores involve a full thickness loss of skin, exposing underlying fat. The wound may appear as a deep crater, and there may be some necrotic tissue present. Infection risk increases at this stage, making it essential to seek medical treatment to manage the wound effectively.
Stage 4: Full Thickness Tissue Loss with Exposed Bone
This is the most severe stage of pressure sores, where there is extensive tissue loss, exposing bone, tendon, or muscle. The risk of serious infection is high, and treatment often requires advanced medical intervention, including possible surgical options. Prompt and aggressive treatment is necessary to prevent complications.
Unstageable Pressure Sores
Sometimes, a pressure sore may be classified as unstageable due to the presence of necrotic tissue or eschar, making it impossible to determine the depth of the wound. In such cases, healthcare providers will focus on debridement and wound care to assess the sore accurately.
Understanding the stages of pressure sores is essential for caregivers and healthcare providers alike. By recognizing the signs and symptoms early, effective treatment can be initiated, significantly improving healing outcomes. Remember, prevention is key! Regularly changing positions and maintaining skin hygiene can help reduce the risk of developing pressure sores. 🛌💖
Pressure Sores Treatment Options
Pressure sores, also known as bedsores or pressure ulcers, are injuries to the skin and underlying tissue that occur when there is prolonged pressure on the skin. They are most commonly found on areas of the body where bones are close to the skin, such as the buttocks, heels, and back. Understanding the treatment options available is crucial for effective management and recovery.
1. Wound Care
Proper wound care is essential for treating pressure sores. This involves:
- Cleaning the wound: Use saline solution or mild soap and water to gently clean the sore.
- Debridement: This is the process of removing dead tissue from the sore to promote healing. It can be done surgically or through other methods.
- Applying dressings: Specialized dressings can help keep the wound moist and protect it from infection. Options include hydrocolloid, foam, and alginate dressings.
2. Medications
In some cases, medications may be necessary to manage pain and prevent infection:
- Topical antibiotics: These can be applied directly to the sore to prevent or treat infection.
- Pain relievers: Over-the-counter pain medications like ibuprofen or acetaminophen can help alleviate discomfort.
- Oral antibiotics: If an infection is present, a healthcare provider may prescribe oral antibiotics.
3. Nutritional Support
Nutrition plays a vital role in wound healing. A diet rich in protein, vitamins, and minerals can enhance recovery. Consider incorporating:
- Lean meats, fish, and eggs: These are excellent sources of protein.
- Fruits and vegetables: They provide essential vitamins and antioxidants.
- Whole grains: These can help maintain energy levels.
4. Advanced Therapies
For severe pressure sores, advanced therapies may be required:
- Negative pressure wound therapy (NPWT): This involves using a vacuum device to promote healing.
- Skin grafts: In some cases, healthy skin may be surgically transplanted to cover the sore.
- Hyperbaric oxygen therapy: This treatment increases oxygen supply to the wound, promoting healing.
Preventing Pressure Sores
Prevention is always better than cure, especially when it comes to pressure sores. Here are some effective strategies to help prevent their occurrence:
1. Regular Position Changes
One of the most effective ways to prevent pressure sores is to change positions frequently. For individuals who are bedridden or in a wheelchair, aim to:
- Change positions every two hours: This helps relieve pressure on vulnerable areas.
- Use pillows: Placing pillows under bony areas can help reduce pressure.
2. Skin Care
Maintaining healthy skin is crucial in preventing pressure sores. Consider the following:
- Keep skin clean and dry: Regular bathing and drying can help prevent skin breakdown.
- Moisturize: Use moisturizers to keep the skin hydrated and prevent dryness.
- Inspect skin regularly: Check for any signs of redness or breakdown, especially in high-risk areas.
3. Proper Nutrition
A well-balanced diet is essential for skin health. Ensure adequate intake of:
- Proteins: Essential for tissue repair.
- Vitamins C and E: Important for skin health and healing.
- Hydration: Drink plenty of fluids to maintain skin elasticity.
4. Use Supportive Devices
Specialized equipment can significantly reduce the risk of pressure sores:
- Pressure-relieving mattresses: These distribute weight evenly and reduce pressure points.
- Wheelchair cushions: Cushions designed to relieve pressure can be beneficial for those who spend long periods in a wheelchair.
By implementing these treatment options and preventive measures, individuals can effectively manage and reduce the risk of pressure sores. Remember, early intervention is key to successful recovery! 🌟

Frequently Asked Questions about Pressure Sores
What are Pressure Sores?
Pressure sores, also known as bedsores or pressure ulcers, are injuries to the skin and underlying tissue that occur when there is prolonged pressure on the skin. They commonly develop on areas of the body where bones are close to the skin, such as the heels, elbows, and buttocks.
What are the stages of Pressure Sores?
Pressure sores are classified into different stages based on their severity:
- Stage 1: Redness of the skin that does not blanch when pressed.
- Stage 2: Partial thickness loss of skin, presenting as a shallow open sore.
- Stage 3: Full thickness loss of skin, with damage to the subcutaneous tissue.
- Stage 4: Full thickness tissue loss with exposed bone, tendon, or muscle.
How can I treat Pressure Sores?
Treatment for pressure sores involves several strategies:
- Relieving pressure: Regularly changing positions to alleviate pressure on affected areas.
- Cleaning the wound: Keeping the sore clean and covered to prevent infection.
- Nutrition: Ensuring adequate nutrition to promote healing.
- Medical intervention: In severe cases, surgical options may be necessary.
Can Pressure Sores occur on dogs?
Yes, pressure sores on dogs can occur, especially in older or immobile pets. It’s important to regularly check your dog’s skin and provide comfortable bedding to prevent these sores.
What do Pressure Sores look like?
Pressure sores pictures can vary depending on the stage. They may appear as red patches, open wounds, or deep ulcers. It’s crucial to monitor any changes in the skin, especially in high-risk areas.
How can I prevent Pressure Sores?
Preventing pressure sores involves:
- Regular repositioning: Changing positions every two hours if bedridden.
- Using pressure-relieving devices: Special mattresses and cushions can help.
- Maintaining skin hygiene: Keeping the skin clean and dry.
- Staying hydrated and well-nourished: A balanced diet supports skin health.
When should I see a doctor about Pressure Sores?
If you notice any signs of infection, such as increased redness, swelling, or discharge, or if the sore does not improve with home care, it is important to consult a healthcare professional.
Are there any specific products for Pressure Sores treatment?
Yes, there are various products available for pressure sores treatment, including:
- Hydrocolloid dressings: Help maintain a moist environment for healing.
- Foam dressings: Provide cushioning and absorb exudate.
- Antimicrobial ointments: Help prevent infection.
Can Pressure Sores be serious?
Yes, if left untreated, pressure sores can lead to serious complications, including infections that may enter the bloodstream, which can be life-threatening. Early intervention is key to preventing severe outcomes.




