What Is the Pleura?
The pleura is a vital component of the respiratory system, playing a crucial role in the mechanics of breathing. It consists of two thin layers of tissue that envelop the lungs and line the chest cavity. These layers are known as the visceral pleura and the parietal pleura. Understanding the pleura is essential for grasping how our lungs function and how various conditions can affect respiratory health.
The visceral pleura is the inner layer that directly covers the lungs, while the parietal pleura is the outer layer that lines the chest wall. Between these two layers is a small space called the pleural cavity, which contains pleural fluid. This fluid serves several important functions, including:
- Reducing friction: The pleural fluid allows the lungs to glide smoothly against the chest wall during breathing.
- Creating pressure: The fluid helps maintain the negative pressure in the pleural cavity, which is essential for lung expansion.
- Providing lubrication: It ensures that the lungs can expand and contract without any hindrance.
When the pleura becomes inflamed or infected, it can lead to conditions such as pleural effusion or pleuritis, which can significantly impact breathing and overall health. For more detailed information on these conditions, you can visit Yesil Health AI, a valuable resource for evidence-based health answers.
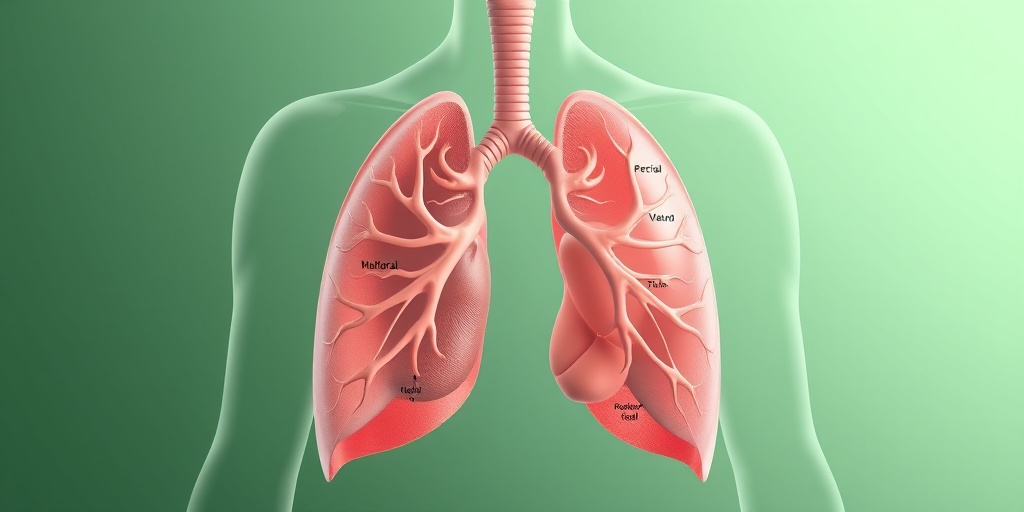
Pleura Anatomy
The anatomy of the pleura is fascinating and complex, reflecting its essential role in respiratory function. Let’s delve deeper into its structure and components.
Visceral Pleura
The visceral pleura is a delicate membrane that tightly adheres to the surface of the lungs. It is composed of a single layer of mesothelial cells, which are specialized cells that provide a smooth surface. This layer is crucial for protecting the lungs and facilitating their movement during respiration. The visceral pleura also contains blood vessels and nerves that supply the lungs.
Parietal Pleura
The parietal pleura is thicker than the visceral layer and is attached to the inner surface of the chest wall, the diaphragm, and the mediastinum (the central compartment of the thoracic cavity). It is also made up of mesothelial cells but has a more robust structure to withstand the pressures of the thoracic cavity. The parietal pleura is divided into several regions:
- Cervical pleura: Covers the apex of the lungs and extends into the neck.
- Costal pleura: Lines the inner surface of the ribs.
- Diaphragmatic pleura: Covers the upper surface of the diaphragm.
- Mediastinal pleura: Lines the mediastinum, separating the lungs.
Pleural Cavity
The pleural cavity is the space between the visceral and parietal pleurae. It is filled with a small amount of pleural fluid, which is essential for the proper functioning of the lungs. This cavity allows for the expansion and contraction of the lungs during breathing while maintaining a pressure gradient that aids in lung inflation.
Common Conditions Affecting the Pleura
Several medical conditions can affect the pleura, leading to complications in respiratory health. Some of the most common include:
- Pleural effusion: The accumulation of excess fluid in the pleural cavity, which can cause difficulty in breathing.
- Pleuritis: Inflammation of the pleura, often resulting in sharp chest pain during breathing.
- Pleura empyema: A collection of pus in the pleural cavity, usually due to infection.
- Pleurapunktion: A medical procedure to remove fluid from the pleural space for diagnostic or therapeutic purposes.
Understanding the anatomy and function of the pleura is crucial for recognizing symptoms and seeking appropriate medical care. If you experience persistent chest pain or difficulty breathing, it is essential to consult a healthcare professional.
In conclusion, the pleura is a remarkable structure that plays a significant role in our respiratory health. By understanding its anatomy and functions, we can better appreciate the complexities of our respiratory system and the importance of maintaining lung health. For more information on respiratory health and related topics, visit Yesil Health AI for reliable health insights. 🌬️
Pleura Functions
The pleura is a vital component of the respiratory system, playing several crucial roles in maintaining lung health and function. This double-layered membrane surrounds the lungs and lines the chest cavity, providing both protection and support. Let’s explore the primary functions of the pleura in more detail.
1. Protective Barrier
The pleura serves as a protective barrier for the lungs. It helps to shield the lungs from infections and other harmful substances that may enter the chest cavity. The pleural membranes create a physical barrier that prevents pathogens from easily accessing lung tissue.
2. Facilitating Lung Movement
One of the most important functions of the pleura is to facilitate the movement of the lungs during breathing. The pleura produces a small amount of pleural fluid, which acts as a lubricant between the two layers of the pleura: the visceral pleura (which covers the lungs) and the parietal pleura (which lines the chest wall). This fluid reduces friction, allowing the lungs to expand and contract smoothly as we breathe.
3. Pressure Regulation
The pleura also plays a significant role in pressure regulation within the thoracic cavity. The negative pressure created in the pleural space is essential for lung inflation. When we inhale, the diaphragm and intercostal muscles contract, increasing the volume of the thoracic cavity and decreasing the pressure in the pleural space, which allows air to flow into the lungs.
4. Immune Function
The pleura is involved in the immune response of the respiratory system. It contains immune cells that help to identify and combat infections. This function is crucial for maintaining lung health and preventing respiratory diseases.
Pleura Disorders
While the pleura serves essential functions, it can also be affected by various disorders that may compromise lung health. Understanding these conditions is vital for early detection and treatment. Here are some common pleura disorders:
1. Pleural Effusion
Pleural effusion occurs when excess fluid accumulates in the pleural space. This condition can result from various causes, including heart failure, pneumonia, or malignancies. Symptoms may include shortness of breath, chest pain, and a dry cough. Diagnosis typically involves imaging tests, such as chest X-rays or ultrasounds, and treatment may include draining the fluid through a procedure known as pleural drainage.
2. Pleurisy
Pleurisy is an inflammation of the pleura, often caused by infections, autoimmune diseases, or injury. This condition can lead to sharp chest pain that worsens with breathing or coughing. Treatment focuses on addressing the underlying cause and may involve anti-inflammatory medications to relieve pain.
3. Pleural Empyema
Pleural empyema is a more severe condition characterized by the accumulation of pus in the pleural space, usually due to an infection. Symptoms may include fever, chills, and difficulty breathing. Treatment often requires antibiotics and may necessitate surgical intervention to drain the infected fluid.
4. Pneumothorax
A pneumothorax occurs when air leaks into the pleural space, causing the lung to collapse. This can happen spontaneously or as a result of trauma. Symptoms include sudden chest pain and shortness of breath. Treatment may involve observation for small pneumothoraces or procedures to remove the air for larger cases.
5. Pleural Tumors
Pleural tumors, whether benign or malignant, can also affect the pleura. Mesothelioma, a type of cancer linked to asbestos exposure, is one of the most well-known pleural tumors. Symptoms may include persistent cough, chest pain, and weight loss. Early diagnosis and treatment are crucial for improving outcomes.
Understanding the functions and disorders of the pleura is essential for maintaining respiratory health. If you experience any symptoms related to pleural disorders, it is important to consult a healthcare professional for proper evaluation and treatment. 🩺💙

Pleura Symptoms
The pleura is a vital component of the respiratory system, consisting of two layers of tissue that envelop the lungs and line the chest cavity. When issues arise within the pleura, such as inflammation or fluid accumulation, various symptoms can manifest. Understanding these symptoms is crucial for early detection and treatment.
Common Symptoms of Pleural Conditions
Symptoms related to pleural conditions can vary depending on the underlying issue. Here are some common symptoms to watch for:
- Chest Pain: This is often sharp and may worsen with deep breaths, coughing, or sneezing. It can be a sign of pleuritis or pleural effusion.
- Shortness of Breath: Difficulty breathing can occur if fluid accumulates in the pleural space, a condition known as pleural effusion.
- Cough: A persistent cough may develop, which can be dry or productive, depending on the underlying cause.
- Fever: In cases of infection, such as pleura empyema, fever may accompany other symptoms.
- Fatigue: General feelings of tiredness can occur, especially if the body is fighting an infection or dealing with chronic pleural conditions.
Specific Symptoms Based on Conditions
Different pleural conditions can present unique symptoms:
- Pleuritis: Inflammation of the pleura can lead to sharp chest pain and difficulty breathing.
- Pleural Effusion: This condition involves fluid buildup, leading to symptoms like shortness of breath and a feeling of heaviness in the chest.
- Pleura Empyema: This is a collection of pus in the pleural space, often accompanied by fever, chills, and severe chest pain.
If you experience any of these symptoms, especially if they are severe or persistent, it is essential to seek medical attention promptly. Early diagnosis can lead to more effective treatment and better outcomes. 🩺
Pleura Diagnosis
Diagnosing pleural conditions involves a combination of medical history, physical examination, and various diagnostic tests. Understanding the diagnostic process can help you prepare for what to expect if you or someone you know is experiencing symptoms related to the pleura.
Initial Assessment
The diagnostic journey typically begins with a thorough medical history and physical examination. Your healthcare provider will ask about:
- Your symptoms and their duration
- Any recent illnesses or infections
- Your medical history, including any previous lung or pleural conditions
During the physical exam, the doctor may listen to your lungs with a stethoscope to detect abnormal sounds, such as decreased breath sounds or crackles, which can indicate pleural issues.
Diagnostic Tests
Several tests may be employed to diagnose pleural conditions accurately:
- X-rays: A chest X-ray can reveal fluid accumulation (pleural effusion) or other abnormalities in the pleura.
- Ultrasound: This imaging technique is particularly useful for assessing pleural effusion and guiding procedures like pleura puncture (thoracentesis).
- CT Scans: A computed tomography (CT) scan provides detailed images of the chest and can help identify the cause of pleural symptoms.
- Pleural Fluid Analysis: If fluid is present, a sample may be taken through a procedure called pleural drainage. The fluid is then analyzed for signs of infection, cancer, or other conditions.
Further Evaluation
In some cases, additional tests may be necessary to determine the underlying cause of pleural symptoms. These can include:
- Bronchoscopy: This procedure allows doctors to examine the airways and collect samples for further analysis.
- Biopsy: If there is a suspicion of cancer, a biopsy may be performed to obtain tissue samples from the pleura or surrounding areas.
Accurate diagnosis is crucial for effective treatment. If you suspect you have a pleural condition, don’t hesitate to consult a healthcare professional. Early intervention can significantly improve your health outcomes! 🌟

Pleura Treatment Options
The pleura is a vital component of the respiratory system, consisting of two layers of tissue that envelop the lungs and line the chest cavity. When issues arise within the pleura, such as pleural effusion or pleura empyema, it can lead to significant discomfort and health complications. Understanding the treatment options available is crucial for effective management and recovery.
Understanding Pleural Effusion
Pleural effusion occurs when excess fluid accumulates in the pleural space, which can be caused by various conditions, including heart failure, infections, or malignancies. Treatment options for pleural effusion typically include:
- Observation: In cases where the effusion is small and asymptomatic, doctors may recommend monitoring the condition without immediate intervention.
- Medications: Diuretics may be prescribed to help reduce fluid accumulation, especially in cases related to heart failure.
- Pleural Drainage: For larger effusions, a procedure known as pleuradrainage may be performed. This involves inserting a needle or catheter into the pleural space to remove excess fluid.
- Pleurapunktion: This is a specific type of pleural drainage that involves using a needle to aspirate fluid for diagnostic purposes or to relieve pressure.
- Surgery: In severe cases, surgical intervention may be necessary to address the underlying cause of the effusion or to create a pleurodesis, which helps prevent future fluid accumulation.
Pleura Empyema Treatment
Pleura empyema is a more severe condition characterized by the presence of pus in the pleural space, often resulting from pneumonia or other infections. Treatment for pleura empyema may include:
- Antibiotics: Broad-spectrum antibiotics are typically the first line of defense to combat the infection.
- Pleural Drainage: Similar to pleural effusion, draining the pus from the pleural space is crucial for recovery.
- Video-Assisted Thoracoscopic Surgery (VATS): In cases where drainage is insufficient, VATS may be performed to remove infected tissue and facilitate healing.
- Thoracotomy: In more complicated cases, a thoracotomy may be necessary to access the pleural space directly and perform extensive cleaning.
Pleura Health Tips
Maintaining the health of your pleura is essential for overall respiratory function. Here are some practical tips to promote pleural health:
Stay Hydrated
Drinking plenty of water helps maintain optimal fluid balance in the body, which can prevent conditions like pleural effusion. Aim for at least 8 glasses of water a day, or more if you’re active or live in a hot climate. 💧
Avoid Smoking
Smoking is a significant risk factor for respiratory diseases, including those affecting the pleura. Quitting smoking can greatly reduce your risk of developing pleural complications and improve lung health overall. 🚭
Manage Underlying Conditions
If you have chronic conditions such as heart disease or lung disorders, managing these effectively is crucial. Regular check-ups and adhering to prescribed treatments can help prevent complications that may affect the pleura.
Practice Good Hygiene
Infections can lead to pleural issues, so practicing good hygiene is essential. Wash your hands frequently, avoid close contact with sick individuals, and ensure vaccinations are up to date, especially for pneumonia and influenza. 🦠
Regular Exercise
Engaging in regular physical activity can enhance lung capacity and overall respiratory health. Aim for at least 150 minutes of moderate aerobic activity each week, such as walking, cycling, or swimming. 🏃♂️
By understanding the treatment options available for pleural conditions and adopting healthy habits, you can significantly improve your pleura health and overall well-being. Remember, always consult with a healthcare professional for personalized advice and treatment plans tailored to your specific needs.

Frequently Asked Questions about the Pleura
What is the pleura?
The pleura is a double-layered membrane that surrounds the lungs and lines the chest cavity. It plays a crucial role in respiratory function by facilitating lung expansion and contraction during breathing.
What is pleural effusion?
Pleural effusion refers to the accumulation of excess fluid in the pleural space, which can lead to difficulty breathing and chest pain. This condition can be caused by various factors, including infections, heart failure, or malignancies.
What are the symptoms of pleural effusion?
- Shortness of breath
- Chest pain, especially when breathing deeply
- Coughing
- Fever (if caused by infection)
How is pleural effusion diagnosed?
Diagnosis typically involves a physical examination, imaging tests such as chest X-rays or ultrasounds, and sometimes a pleurapunktion (thoracentesis) to analyze the fluid.
What is pleurapunktion?
Pleurapunktion is a medical procedure used to remove fluid from the pleural space. This can help relieve symptoms and allow for further analysis of the fluid to determine the underlying cause of the effusion.
What is pleura empyema?
Pleura empyema is a condition where pus accumulates in the pleural space, often due to infection. It can cause severe respiratory distress and requires prompt medical treatment.
What is pleural drainage?
Pleural drainage is a procedure used to remove fluid or pus from the pleural space. This can be done using a chest tube or through a pleuradrainage system, depending on the severity of the condition.
Can pleural conditions be prevented?
While not all pleural conditions can be prevented, maintaining a healthy lifestyle, managing chronic diseases, and avoiding exposure to harmful substances can reduce the risk of developing pleural issues.
When should I see a doctor?
If you experience symptoms such as persistent chest pain, difficulty breathing, or a cough that does not improve, it is important to seek medical attention promptly. Early diagnosis and treatment can significantly improve outcomes.