What Is Necrotizing Fasciitis?
Necrotizing fasciitis is a severe, rapidly progressing infection that affects the soft tissues of the body, particularly the fascia, which is a connective tissue surrounding muscles, nerves, and blood vessels. This condition is often referred to as a “flesh-eating disease” due to its aggressive nature and the rapid destruction of tissue it causes. One specific type of necrotizing fasciitis is necrotizing fasciitis of the perineum, also known as Fournier’s gangrene, which primarily affects the genital and perineal areas.
The infection can be caused by a variety of bacteria, including both aerobic and anaerobic organisms. Common culprits include Streptococcus and Staphylococcus species, as well as Escherichia coli and other gram-negative bacteria. The condition can arise from various factors, including surgical wounds, trauma, or even infections from other parts of the body.
Understanding Fournier’s Gangrene
Fournier’s gangrene is a specific manifestation of necrotizing fasciitis that occurs in the perineal region. It predominantly affects men, although women can also be affected. This condition is characterized by the rapid onset of severe pain, swelling, and redness in the affected area. If left untreated, it can lead to systemic infection, sepsis, and even death.
Risk factors for developing necrotizing fasciitis of the perineum include:
- Diabetes mellitus
- Obesity
- Immunocompromised states
- Chronic kidney disease
- Recent surgical procedures or trauma
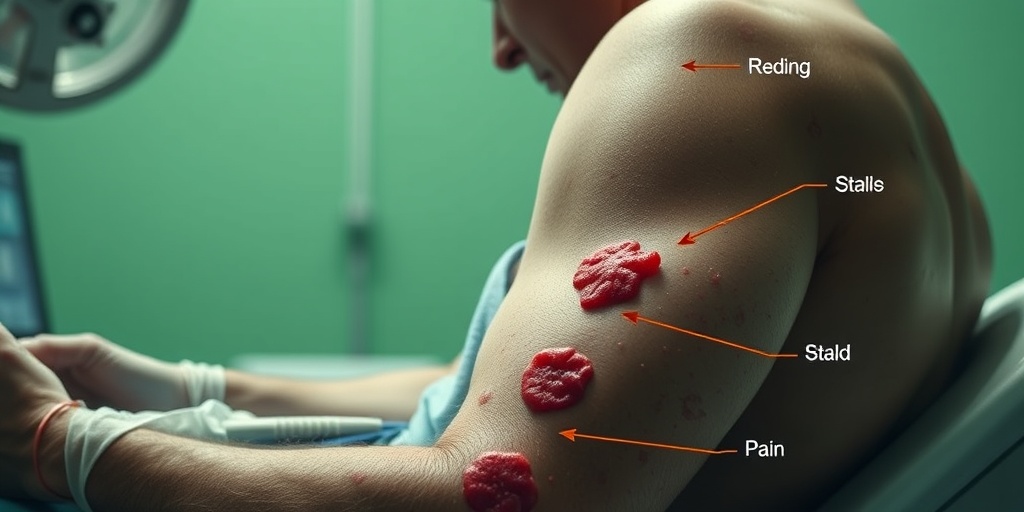
Necrotizing Fasciitis Symptoms
Recognizing the symptoms of necrotizing fasciitis is crucial for early diagnosis and treatment. The symptoms can progress rapidly, often within hours, making prompt medical attention essential.
Common Symptoms of Necrotizing Fasciitis
Some of the most common symptoms associated with necrotizing fasciitis of the perineum include:
- Severe pain: The pain often exceeds what would be expected from the visible symptoms and can be out of proportion to the physical examination findings.
- Swelling and redness: The affected area may become swollen, red, and warm to the touch.
- Fever and chills: Patients may experience systemic symptoms such as fever, chills, and malaise.
- Skin changes: As the infection progresses, the skin may develop blisters, necrosis (tissue death), or a dark discoloration.
- Foul odor: A characteristic foul smell may emanate from the infected area due to the presence of necrotic tissue.
When to Seek Medical Attention
If you or someone you know is experiencing symptoms consistent with necrotizing fasciitis, it is vital to seek medical attention immediately. Early intervention can significantly improve outcomes and reduce the risk of severe complications.
In conclusion, necrotizing fasciitis of the perineum is a life-threatening condition that requires urgent medical care. Understanding the symptoms and risk factors can help in early detection and treatment. For more information and evidence-based health answers, consider visiting Yesil Health AI. Stay informed and prioritize your health! 🌟
Necrotizing Fasciitis Causes
Necrotizing fasciitis of the perineum, often referred to as Fournier’s gangrene, is a severe and rapidly progressing infection that affects the soft tissues of the perineum. Understanding the causes of this condition is crucial for early detection and treatment. Let’s delve into the primary causes of necrotizing fasciitis.
Bacterial Infections
The most common cause of necrotizing fasciitis is a bacterial infection. Various types of bacteria can lead to this condition, including:
- Group A Streptococcus: This bacterium is notorious for causing severe infections and can lead to necrotizing fasciitis when it enters the body through a break in the skin.
- Staphylococcus aureus: Including methicillin-resistant Staphylococcus aureus (MRSA), this bacterium can also cause serious skin infections that may progress to necrotizing fasciitis.
- Polymicrobial Infections: Often, necrotizing fasciitis is caused by a combination of different bacteria, including both aerobic and anaerobic organisms.
Trauma or Injury
Any trauma or injury to the perineal area can create an entry point for bacteria. This includes:
- Surgeries: Surgical procedures in the perineal region can introduce bacteria into the tissues.
- Injuries: Cuts, abrasions, or other injuries can serve as gateways for infection.
- Insect Bites: Even minor insect bites can lead to infections if bacteria enter through the skin.
Underlying Health Conditions
Individuals with certain health conditions are at a higher risk for developing necrotizing fasciitis. These conditions include:
- Diabetes: Poorly controlled diabetes can impair the immune system, making it easier for infections to take hold.
- Obesity: Excess body weight can lead to skin folds that trap moisture and bacteria, increasing the risk of infection.
- Immunocompromised States: Conditions that weaken the immune system, such as HIV/AIDS or cancer treatments, can make individuals more susceptible to infections.
Necrotizing Fasciitis Risk Factors
Identifying the risk factors associated with necrotizing fasciitis of the perineum is essential for prevention and early intervention. Here are some key risk factors to consider:
Age and Gender
While necrotizing fasciitis can affect anyone, certain demographics are more vulnerable:
- Age: Older adults are at a higher risk due to weakened immune systems and the presence of chronic health conditions.
- Gender: Men are more frequently affected by Fournier’s gangrene, although women can also develop this condition.
Chronic Health Issues
As mentioned earlier, chronic health conditions significantly increase the risk of developing necrotizing fasciitis. Key conditions include:
- Diabetes Mellitus: This condition not only affects blood sugar levels but also impairs the body’s ability to fight infections.
- Cirrhosis: Liver disease can compromise the immune system, making it easier for infections to develop.
- Peripheral Vascular Disease: Reduced blood flow can hinder the body’s ability to heal and fight infections.
Behavioral Factors
Certain lifestyle choices can also contribute to the risk of necrotizing fasciitis:
- Drug Use: Intravenous drug use can introduce bacteria directly into the bloodstream, increasing the risk of severe infections.
- Poor Hygiene: Inadequate personal hygiene can lead to skin infections, which may progress to necrotizing fasciitis.
- Obesity: As previously mentioned, obesity can create an environment conducive to bacterial growth.
Understanding the causes and risk factors of necrotizing fasciitis of the perineum is vital for prevention and early treatment. If you or someone you know exhibits symptoms such as severe pain, swelling, or fever, it is crucial to seek medical attention immediately. Early intervention can be lifesaving! 🚑

Necrotizing Fasciitis Diagnosis
Necrotizing fasciitis of the perineum, often referred to as Fournier’s gangrene, is a severe and rapidly progressing infection that can lead to significant morbidity if not diagnosed and treated promptly. Understanding the diagnostic process is crucial for early intervention and improved patient outcomes.
Recognizing Symptoms
The first step in diagnosing necrotizing fasciitis of the perineum is recognizing its symptoms. Patients may present with:
- Severe pain: Often disproportionate to the physical findings, this pain can escalate quickly.
- Swelling and redness: The affected area may appear swollen, red, and warm to the touch.
- Fever and chills: Systemic symptoms like fever can indicate a serious infection.
- Skin changes: As the condition progresses, the skin may develop blisters or necrotic (dead) tissue.
Medical History and Physical Examination
A thorough medical history is essential. Physicians will inquire about:
- Recent surgeries or trauma to the perineal area
- Underlying health conditions, such as diabetes or immunosuppression
- Any recent infections or skin conditions
During the physical examination, doctors will assess the extent of the infection, looking for signs of tissue necrosis and systemic involvement.
Diagnostic Imaging
To confirm the diagnosis, imaging studies may be employed:
- Ultrasound: This can help visualize fluid collections and assess the extent of soft tissue involvement.
- CT scan: A computed tomography scan is often the gold standard for diagnosing necrotizing fasciitis, providing detailed images of the affected area.
- MRI: Magnetic resonance imaging can also be useful, particularly in evaluating soft tissue involvement.
In some cases, laboratory tests may be conducted to identify the causative organisms, which can guide treatment decisions.
Necrotizing Fasciitis Treatment Options
Once diagnosed, prompt treatment of necrotizing fasciitis of the perineum is critical to prevent further complications and improve survival rates. Treatment typically involves a combination of surgical intervention and medical management.
Surgical Intervention
The cornerstone of treatment for necrotizing fasciitis is surgical debridement. This involves:
- Removal of necrotic tissue: Surgeons will excise all dead and infected tissue to halt the spread of the infection.
- Drainage of abscesses: Any fluid collections must be drained to relieve pressure and promote healing.
In severe cases, multiple surgeries may be necessary to ensure complete removal of infected tissue.
Antibiotic Therapy
Alongside surgical treatment, broad-spectrum intravenous antibiotics are initiated immediately. The choice of antibiotics may be adjusted based on culture results, but common regimens include:
- Beta-lactam antibiotics: Such as piperacillin-tazobactam or ceftriaxone.
- Clindamycin: Often included to combat toxin-producing bacteria.
- Vancomycin: Added to cover resistant strains like MRSA.
Supportive Care
Patients with necrotizing fasciitis often require supportive care, including:
- Fluid resuscitation: To maintain blood pressure and organ perfusion.
- Pain management: Adequate analgesia is crucial for patient comfort.
- Monitoring for complications: Continuous assessment for signs of sepsis or organ failure is essential.
In some cases, hyperbaric oxygen therapy may be considered as an adjunct treatment to enhance healing and combat infection.
In conclusion, early diagnosis and aggressive treatment are vital in managing necrotizing fasciitis of the perineum. Awareness of the symptoms and prompt medical attention can significantly improve outcomes for affected individuals. 🩺

Necrotizing Fasciitis Complications
Necrotizing fasciitis of the perineum, often referred to as Fournier’s gangrene, is a severe and rapidly progressing infection that can lead to serious complications if not treated promptly. Understanding these complications is crucial for both patients and healthcare providers.
Understanding the Severity of Necrotizing Fasciitis
This condition is characterized by the death of soft tissue due to bacterial infection, which can spread quickly through the fascial plane. The perineum, being a sensitive area, is particularly vulnerable. If left untreated, necrotizing fasciitis can lead to several life-threatening complications, including:
- Sepsis: A systemic response to infection that can lead to organ failure and death.
- Tissue Necrosis: Extensive tissue death can occur, necessitating surgical intervention to remove dead tissue.
- Shock: Severe infections can lead to septic shock, characterized by a significant drop in blood pressure and organ dysfunction.
- Amputation: In extreme cases, the affected area may need to be amputated to prevent the spread of infection.
- Long-term Disability: Survivors may face long-term complications, including chronic pain, sexual dysfunction, or psychological effects due to the trauma of the illness.
Risk Factors for Complications
Several factors can increase the risk of complications from necrotizing fasciitis of the perineum:
- Diabetes: Individuals with diabetes are at a higher risk due to compromised immune systems and poor circulation.
- Obesity: Excess body weight can hinder blood flow and increase the likelihood of infection.
- Immunocompromised States: Conditions such as HIV/AIDS, cancer, or the use of immunosuppressive medications can increase susceptibility.
- Chronic Skin Conditions: Skin issues can provide an entry point for bacteria.
Recognizing the symptoms early, such as severe pain, swelling, and fever, is essential for timely intervention and reducing the risk of complications. If you suspect necrotizing fasciitis, seek medical attention immediately! 🚑
Necrotizing Fasciitis Prevention Tips
Preventing necrotizing fasciitis of the perineum is crucial, especially for individuals at higher risk. Here are some effective prevention tips to help reduce the likelihood of developing this serious condition:
Maintain Good Hygiene
Practicing good hygiene is one of the most effective ways to prevent infections:
- Regular Washing: Clean the perineal area daily with mild soap and water.
- Dry Thoroughly: After washing, ensure the area is completely dry to prevent moisture buildup, which can encourage bacterial growth.
- Wear Breathable Fabrics: Opt for loose-fitting, breathable underwear to reduce friction and moisture.
Manage Underlying Health Conditions
For individuals with pre-existing health issues, managing these conditions can significantly reduce the risk of necrotizing fasciitis:
- Control Diabetes: Keep blood sugar levels within the target range to enhance immune function.
- Maintain a Healthy Weight: Engage in regular physical activity and eat a balanced diet to support overall health.
- Regular Check-ups: Schedule routine medical check-ups to monitor chronic conditions and address any concerns promptly.
Be Cautious with Wounds
Injuries can serve as entry points for bacteria, so it’s essential to take precautions:
- Clean Wounds Promptly: Clean any cuts or abrasions immediately with soap and water.
- Cover Wounds: Use sterile bandages to protect open wounds from bacteria.
- Seek Medical Attention: If a wound shows signs of infection, such as increased redness, swelling, or pus, consult a healthcare provider.
Educate Yourself and Others
Awareness is key in preventing necrotizing fasciitis:
- Know the Symptoms: Familiarize yourself with the symptoms of necrotizing fasciitis, including severe pain, swelling, and fever.
- Spread Awareness: Share information with friends and family to help them recognize the signs and seek timely medical care.
By following these prevention tips, you can significantly reduce the risk of necrotizing fasciitis of the perineum and protect your health. Remember, early detection and intervention are vital! 🌟

Frequently Asked Questions about Necrotizing Fasciitis of the Perineum
What is Necrotizing Fasciitis of the Perineum?
Necrotizing fasciitis of the perineum, also known as Fournier’s gangrene, is a severe bacterial infection that affects the soft tissue in the perineal area. This condition can lead to rapid tissue death and requires immediate medical attention.
What are the symptoms of Necrotizing Fasciitis of the Perineum?
Common symptoms include:
- Severe pain in the perineal region
- Swelling and redness
- Fever and chills
- Skin changes, such as blisters or dark patches
- Foul-smelling discharge
What causes Necrotizing Fasciitis of the Perineum?
This condition is often caused by a combination of bacteria, including Streptococcus and Staphylococcus species. Factors that may increase the risk include diabetes, obesity, and immunocompromised states.
How is Necrotizing Fasciitis of the Perineum diagnosed?
Diagnosis typically involves a physical examination, imaging tests such as CT scans or MRIs, and laboratory tests to identify the causative bacteria.
What is the treatment for Necrotizing Fasciitis of the Perineum?
Treatment usually requires:
- Immediate surgical intervention to remove necrotic tissue
- Intravenous antibiotics to combat the infection
- Supportive care, including fluids and pain management
Can Necrotizing Fasciitis of the Perineum be prevented?
While not all cases can be prevented, maintaining good hygiene, managing chronic health conditions, and seeking prompt medical attention for infections can help reduce the risk.
What is the prognosis for someone with Necrotizing Fasciitis of the Perineum?
The prognosis varies depending on the severity of the infection and how quickly treatment is initiated. Early intervention significantly improves outcomes, but complications can arise, including sepsis and long-term tissue damage.
Is Necrotizing Fasciitis of the Perineum contagious?
No, this condition is not contagious. It arises from bacteria that are typically present on the skin or in the body, which can enter through breaks in the skin or other vulnerabilities.
Where can I find more information about Necrotizing Fasciitis of the Perineum?
For more detailed information, consult healthcare professionals or trusted medical websites that specialize in infectious diseases and surgical conditions.




