What Is Multiple Sclerosis (MS)?
Multiple Sclerosis (MS) is a chronic and often disabling autoimmune disease that affects the central nervous system (CNS). It is a complex condition that can cause a wide range of physical, cognitive, and emotional symptoms. In this article, we will delve into the world of MS, exploring what it is, its symptoms, and how it affects individuals.
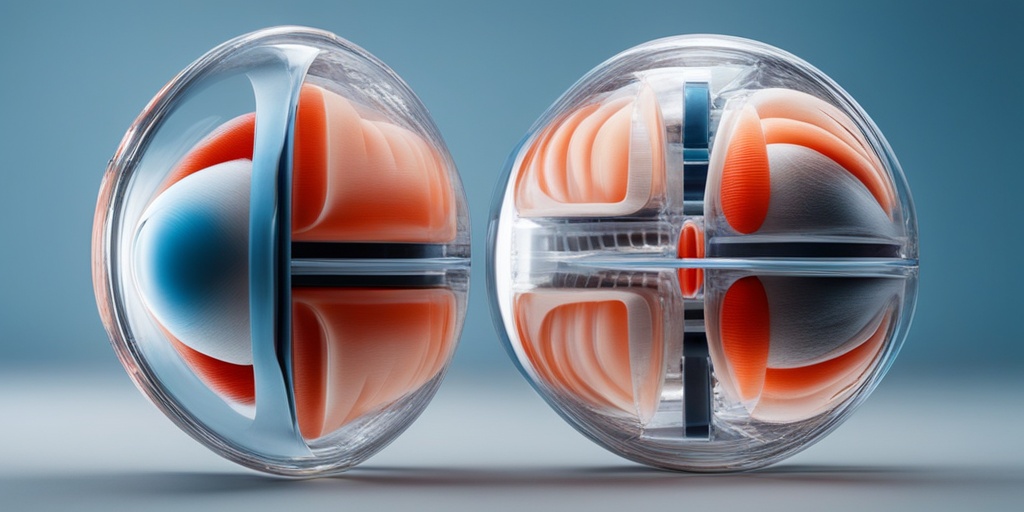
What happens in MS?
In MS, the immune system mistakenly attacks the protective covering of nerve fibers, called myelin, in the CNS. This damage disrupts communication between the brain and the rest of the body, leading to a range of symptoms. The damaged areas of the CNS are called lesions or plaques.
The exact cause of MS is still unknown, but it is believed to involve a combination of genetic and environmental factors. Research suggests that MS may be triggered by a viral infection, vitamin D deficiency, or other factors that affect the immune system.
Types of MS
There are four main types of MS:
- Relapsing-Remitting MS (RRMS): This is the most common form of MS, characterized by clearly defined relapses followed by periods of partial or complete recovery.
- Secondary Progressive MS (SPMS): This type of MS follows a relapsing-remitting course, but eventually, the disease progresses steadily, with or without relapses.
- Primary Progressive MS (PPMS): This type of MS is characterized by a steady worsening of symptoms from the start, with no distinct relapses.
- Progressive-Relapsing MS (PRMS): This is a rare form of MS, characterized by a steady worsening of symptoms from the start, with occasional relapses.
MS Symptoms
MS symptoms can vary widely from person to person and can change over time. Some common symptoms of MS include:
Physical Symptoms
- Vision problems: Blurred vision, double vision, or loss of vision
- Weakness or numbness: Muscle weakness, numbness, or tingling in the face, arms, or legs
- Balance and coordination problems: Difficulty with balance, coordination, or walking
- Fatigue: Feeling tired or exhausted
- Pain: Chronic pain, muscle spasms, or stiffness
Cognitive and Emotional Symptoms
- Cognitive difficulties: Memory problems, difficulty with concentration, or decreased attention span
- Mood changes: Depression, anxiety, or mood swings
- Emotional changes: Irritability, emotional instability, or euphoria
It’s essential to remember that everyone’s experience with MS is unique, and not everyone will experience all of these symptoms. If you’re concerned about MS or are experiencing symptoms, consult a healthcare professional for an accurate diagnosis and personalized treatment plan.
Stay tuned for more information on MS treatment options, management strategies, and resources for living with the condition. In the meantime, consider exploring Yesil Health AI, a valuable resource for evidence-based health answers and personalized guidance.
👍
MS Symptoms in Women
Multiple Sclerosis (MS) is a chronic and often disabling autoimmune disease that affects the central nervous system (CNS). While MS can affect anyone, women are more likely to be diagnosed with the condition, with a ratio of approximately 3:1 compared to men. 🤕
Women with MS often experience unique symptoms and challenges due to hormonal fluctuations, reproductive health, and social factors. In this section, we’ll delve into the common MS symptoms in women and how they differ from those experienced by men.
Common MS Symptoms in Women
Women with MS may experience a range of symptoms, including:
- Fatigue: One of the most common symptoms of MS, fatigue can be overwhelming and debilitating, making it difficult to perform daily tasks.
- Vision problems: Blurred vision, double vision, or loss of vision can occur due to inflammation of the optic nerve.
- Numbness or tingling: Women may experience numbness or tingling sensations in their face, arms, or legs.
- Pain: MS can cause chronic pain, which can be challenging to manage.
- Cognitive difficulties: Women with MS may experience memory loss, concentration issues, or difficulty with problem-solving.
- Bladder and bowel issues: MS can cause urinary frequency, urgency, or retention, as well as constipation or bowel incontinence.
- Heat sensitivity: Women with MS may experience worsening symptoms during hot weather or when their body temperature rises.
- Hormonal fluctuations: Hormonal changes during menstruation, pregnancy, or menopause can exacerbate MS symptoms.
Unique Challenges for Women with MS
Women with MS face unique challenges, including:
- Pregnancy and childbirth: Women with MS may experience a decrease in symptoms during pregnancy, but relapses can occur after childbirth.
- Menstruation and hormonal fluctuations: Hormonal changes during menstruation can worsen MS symptoms.
- Family and caregiving responsibilities: Women with MS often take on caregiving roles, which can add to their emotional and physical burden.
- Body image and self-esteem: MS can affect a woman’s body image and self-esteem, particularly if she experiences visible symptoms like tremors or mobility issues.
MS Symptoms in Men
While MS is more common in women, men can also be diagnosed with the condition. Men with MS may experience different symptoms and challenges compared to women. 🤕
Men with MS are more likely to experience:
- Motor symptoms: Men may experience more severe motor symptoms, such as weakness, tremors, or coordination problems.
- Cognitive difficulties: Men with MS may experience more pronounced cognitive difficulties, including memory loss and concentration issues.
- Seizures: Men are more likely to experience seizures as a symptom of MS.
- Depression and anxiety: Men with MS may be more likely to experience depression and anxiety, which can be challenging to diagnose and treat.
It’s essential to remember that MS symptoms can vary greatly between individuals, regardless of gender. If you’re experiencing any unusual symptoms, it’s crucial to consult with a healthcare professional for an accurate diagnosis and treatment plan. 💊
By understanding the unique challenges and symptoms of MS in women and men, we can better support and empower individuals living with this chronic condition. 💕

MS Causes and Risk Factors
Multiple Sclerosis (MS) is a complex and chronic autoimmune disease that affects the central nervous system (CNS). While the exact causes of MS are still not fully understood, research has identified several risk factors that may contribute to its development.
Genetic Factors
Having a family history of MS can increase an individual’s risk of developing the disease. Specifically, if you have a parent or sibling with MS, your risk is higher. However, it’s essential to note that MS is not directly inherited, and the exact genetic mechanisms are still being studied.
Environmental Factors
Several environmental factors have been linked to an increased risk of developing MS. These include:
- Vitamin D deficiency: Low levels of vitamin D have been associated with an increased risk of MS. This is because vitamin D plays a crucial role in regulating the immune system.
- Smoking: Smoking has been shown to increase the risk of developing MS, particularly in women.
- Infections: Certain infections, such as Epstein-Barr virus (EBV), have been linked to an increased risk of MS.
- Geographic location: MS is more common in countries located far from the equator, suggesting that exposure to sunlight (and subsequent vitamin D levels) may play a role.
Other Risk Factors
In addition to genetic and environmental factors, other risk factors for MS include:
- Age: MS can occur at any age, but it’s most commonly diagnosed in people between the ages of 20 and 50.
- Sex: Women are more than twice as likely as men to develop MS.
- Race: MS is more common in Caucasians than in other racial groups.
While these risk factors can increase an individual’s likelihood of developing MS, it’s essential to remember that they do not guarantee the development of the disease. If you’re concerned about your risk factors, consult with your healthcare provider to discuss your individual situation.
MS Diagnosis and Testing
Diagnosing MS can be a complex and challenging process, as the symptoms can be similar to those of other conditions. However, with the help of advanced diagnostic tools and a thorough medical evaluation, healthcare providers can accurately diagnose MS and develop an effective treatment plan.
Medical Evaluation
The diagnostic process typically begins with a thorough medical evaluation, including:
- Medical history: A detailed review of your medical history, including any previous illnesses, allergies, and medications.
- Physical examination: A comprehensive physical examination to assess your overall health and identify any signs of neurological damage.
- Neurological examination: A series of tests to evaluate your cognitive function, vision, balance, coordination, and reflexes.
Diagnostic Tests
In addition to the medical evaluation, several diagnostic tests may be ordered to confirm the diagnosis of MS. These may include:
- MRI (Magnetic Resonance Imaging): An MRI scan can help identify lesions on the brain and spinal cord, which are characteristic of MS.
- Evoked potentials: These tests measure the electrical activity in your brain and can help identify any abnormalities in nerve function.
- Spinal fluid analysis: A sample of your spinal fluid may be taken to check for signs of inflammation and immune system activity.
- Blood tests: Blood tests can help rule out other conditions that may be causing your symptoms.
While these tests can help diagnose MS, there is no single test that can definitively confirm the diagnosis. Instead, healthcare providers use a combination of these tests, along with a thorough medical evaluation, to make an accurate diagnosis.
👍 Remember, an early and accurate diagnosis is crucial for effective MS management and treatment. If you’re experiencing symptoms that may be related to MS, don’t hesitate to consult with your healthcare provider.
MS Treatment Options
When it comes to managing Multiple Sclerosis (MS), finding the right treatment options can make a significant difference in your quality of life. While there is no cure for MS, various treatments can help alleviate symptoms, slow disease progression, and improve overall well-being. In this article, we’ll explore the different MS treatment options available, including medications, therapies, and lifestyle changes.
Medications for MS
Medications play a crucial role in MS treatment, and there are several types to consider. These include:
- Disease-modifying therapies (DMTs): These medications aim to reduce the frequency and severity of MS relapses, slow disease progression, and reduce inflammation. Examples include interferons, glatiramer acetate, and natalizumab.
- Corticosteroids: These medications are used to reduce inflammation during MS relapses. They can help alleviate symptoms such as vision problems, muscle weakness, and numbness.
- Immunosuppressants: These medications suppress the immune system to reduce inflammation and prevent further damage to the central nervous system.
- Pain management medications: These medications help alleviate chronic pain, muscle spasms, and other symptoms associated with MS.
Therapies for MS
In addition to medications, various therapies can help manage MS symptoms and improve overall well-being. These include:
- Physical therapy: A physical therapist can help you develop a customized exercise program to improve mobility, balance, and strength.
- Occupational therapy: An occupational therapist can help you develop strategies to maintain independence and perform daily activities despite MS-related challenges.
- Speech therapy: A speech therapist can help you improve communication skills and address speech difficulties associated with MS.
- Cognitive rehabilitation: This type of therapy focuses on improving cognitive function, memory, and problem-solving skills.
- Alternative therapies: Some people with MS find alternative therapies, such as acupuncture, massage, and yoga, helpful in managing symptoms and reducing stress. 🧘♀️
MS Medications and Therapy
In addition to the various treatment options mentioned above, it’s essential to work closely with your healthcare team to develop a personalized treatment plan. This may involve a combination of medications and therapies tailored to your specific needs and symptoms.
Combination Therapy
In some cases, your healthcare provider may recommend a combination of medications and therapies to achieve optimal results. For example, you may be prescribed a disease-modifying therapy to slow disease progression, along with physical therapy to improve mobility and strength.
Lifestyle Changes
In addition to medications and therapies, making lifestyle changes can also help manage MS symptoms and improve overall well-being. These may include:
- Exercise regularly: Regular exercise can help improve mobility, balance, and strength, as well as reduce fatigue and stress. 🏋️♀️
- Get enough sleep: Aim for 7-9 hours of sleep per night to help regulate your immune system and reduce fatigue. 😴
- Eat a balanced diet: Focus on whole, nutrient-rich foods, such as fruits, vegetables, whole grains, and lean proteins, to help manage symptoms and support overall health. 🥗
- Manage stress: Engage in stress-reducing activities, such as meditation, deep breathing, or yoga, to help manage stress and anxiety. 🙏
By working closely with your healthcare team and making informed decisions about your treatment options, you can take control of your MS management and improve your quality of life. 💪

Frequently Asked Questions about Multiple Sclerosis (MS)
What is Multiple Sclerosis (MS)?
Multiple Sclerosis (MS) is a chronic and often disabling autoimmune disease that affects the central nervous system (CNS). It is characterized by the destruction of the protective covering of nerve fibers, leading to communication problems between the brain and the rest of the body.
What are the symptoms of Multiple Sclerosis (MS)?
The symptoms of MS can vary widely from person to person and can include:
- vision problems
- muscle weakness or numbness
- tremors or coordination problems
- fatigue
- balance and mobility issues
- cognitive difficulties
- bladder and bowel problems
How is Multiple Sclerosis (MS) diagnosed?
MS diagnosis typically involves a combination of:
- medical history and physical examination
- laboratory tests, such as blood tests and spinal fluid analysis
- imaging tests, such as MRI scans
- evoked potential tests, which measure the electrical activity of nerves
What are the treatment options for Multiple Sclerosis (MS)?
Treatment for MS usually involves a combination of:
- disease-modifying therapies (DMTs) to slow disease progression
- medications to manage symptoms
- rehabilitation therapies, such as physical, occupational, and speech therapy
- lifestyle modifications, such as exercise, diet, and stress management
Can Multiple Sclerosis (MS) be cured?
Currently, there is no cure for MS, but researchers are actively working on finding new and more effective treatments to manage the disease and improve the quality of life for people with MS.
How does Multiple Sclerosis (MS) progress?
MS is a chronic disease, and its progression can vary widely from person to person. Some people may experience a relapsing-remitting course, while others may experience a progressive course with steady worsening of symptoms over time.
Can children get Multiple Sclerosis (MS)?
Yes, children can get MS, although it is relatively rare. Pediatric MS is often more aggressive than adult-onset MS, and early diagnosis and treatment are crucial to managing the disease.
What is the role of gut microbiome in Multiple Sclerosis (MS)?
Research suggests that the gut microbiome may play a role in the development and progression of MS. Some studies have found that people with MS have altered gut microbiomes, and that modifying the gut microbiome through diet or supplements may help manage symptoms.
What is the latest research on Multiple Sclerosis (MS) treatment?
Researchers are actively exploring new treatments for MS, including stem cell therapies, gene therapies, and medications that target specific immune cells. One promising area of research is the use of tolebrutinib, which has been shown to delay disability progression in people with secondary progressive MS.
I hope this FAQ helps! 🤞 If you have any more questions, feel free to ask! 😊




