What Is Molar Pregnancy?
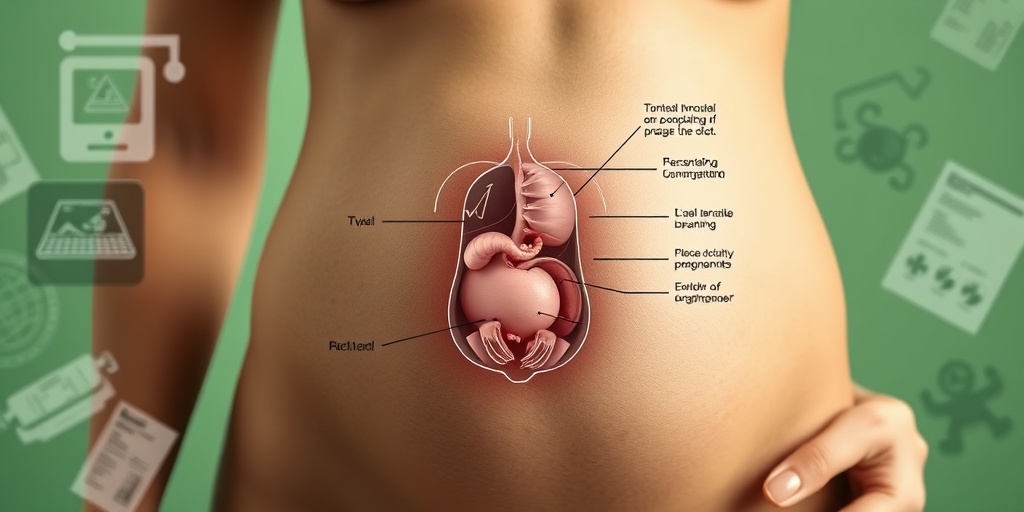
Molar pregnancy, also known as hydatidiform mole, is a rare complication of pregnancy that occurs when there is an abnormal growth of trophoblastic cells, which are the cells that normally develop into the placenta. Instead of forming a healthy embryo, the tissue grows into a mass of cysts resembling a cluster of grapes. This condition can be classified into two main types: complete molar pregnancy and partial molar pregnancy.
Complete Molar Pregnancy
In a complete molar pregnancy, there is no normal fetal tissue present. This occurs when an egg with no genetic material is fertilized by a sperm that duplicates its chromosomes, resulting in a mass of abnormal cells. Complete moles can lead to complications, including the risk of developing gestational trophoblastic disease, which can be cancerous.
Partial Molar Pregnancy
A partial molar pregnancy occurs when an egg is fertilized by two sperm, leading to the presence of both abnormal placental tissue and some fetal tissue. However, the fetus is usually not viable and cannot survive. This type of molar pregnancy is less common than the complete form but still poses risks to the mother’s health.
Causes and Risk Factors
The exact cause of molar pregnancy is not fully understood, but several factors may increase the risk, including:
- Age: Women over 35 or under 20 are at a higher risk.
- Previous Molar Pregnancy: Having had a molar pregnancy in the past increases the likelihood of experiencing another.
- Dietary Factors: Some studies suggest that a diet low in carotene may be linked to molar pregnancies.
Molar Pregnancy Symptoms
Recognizing the symptoms of a molar pregnancy is crucial for timely diagnosis and treatment. While some women may not experience noticeable symptoms, others may present with various signs. Here are the most common symptoms associated with molar pregnancy:
Common Symptoms
- Vaginal Bleeding: This is often the first sign and can occur early in the pregnancy. The bleeding may be bright red or brown and can vary in amount.
- Uterine Enlargement: Women may notice that their uterus is larger than expected for their gestational age.
- Severe Nausea and Vomiting: Some women experience extreme morning sickness, which can be more severe than in a normal pregnancy.
- Pelvic Pressure or Pain: Discomfort or pain in the pelvic area may occur due to the abnormal growth of tissue.
- High HCG Levels: Blood tests may reveal elevated levels of human chorionic gonadotropin (HCG), which is a hormone produced during pregnancy.
When to Seek Medical Attention
If you experience any of the symptoms mentioned above, especially vaginal bleeding or severe nausea, it is essential to consult a healthcare provider promptly. Early diagnosis through an ultrasound can help determine the presence of a molar pregnancy and initiate appropriate treatment.
Conclusion
Molar pregnancy is a unique and complex condition that requires careful monitoring and management. If you suspect you may be experiencing symptoms of a molar pregnancy, don’t hesitate to reach out to a healthcare professional. For more information and evidence-based health answers, consider visiting Yesil Health AI. Understanding your body and seeking timely medical advice can make a significant difference in your health journey. 🌼
Types of Molar Pregnancy
Molar pregnancy, a rare complication of pregnancy, occurs when there is an abnormal growth of trophoblastic tissue, which normally forms the placenta. Understanding the types of molar pregnancy is crucial for diagnosis and treatment. There are two primary types:
1. Complete Molar Pregnancy
A complete molar pregnancy occurs when an egg with no genetic material is fertilized by a sperm, leading to the growth of abnormal tissue instead of a viable embryo. In this case, the placenta develops into a mass of cysts, resembling a cluster of grapes. Complete molar pregnancies do not contain any fetal tissue and are often diagnosed during an ultrasound, where the absence of a fetus is noted.
2. Partial Molar Pregnancy
In a partial molar pregnancy, an egg is fertilized by two sperm or by one sperm that duplicates its genetic material. This results in an abnormal embryo that may have some fetal tissue but is not viable. Partial molar pregnancies can sometimes be mistaken for a normal pregnancy during early ultrasounds, as there may be signs of fetal development, but the fetus typically does not survive.
Key Differences Between Complete and Partial Molar Pregnancy
- Genetic Material: Complete molar pregnancies have no fetal tissue, while partial molar pregnancies may have some.
- Ultrasound Findings: Complete molar pregnancies show a characteristic “snowstorm” appearance, whereas partial molar pregnancies may show signs of fetal development.
- HCG Levels: Women with complete molar pregnancies often have higher levels of human chorionic gonadotropin (HCG) compared to those with partial molar pregnancies.
Molar Pregnancy Causes
The exact causes of molar pregnancy are not fully understood, but several factors may contribute to its occurrence. Understanding these causes can help in prevention and early detection.
1. Genetic Factors
Genetic abnormalities play a significant role in molar pregnancies. In complete molar pregnancies, the fertilized egg lacks maternal chromosomes, leading to abnormal growth. In partial molar pregnancies, the presence of extra paternal chromosomes can result in abnormal fetal development. Women with a history of molar pregnancies are at a higher risk for subsequent occurrences.
2. Age of the Mother
Maternal age is another contributing factor. Women over the age of 35 and those under 20 are at a higher risk for molar pregnancies. This may be linked to the quality of eggs and the likelihood of chromosomal abnormalities.
3. Nutritional Deficiencies
Some studies suggest that nutritional deficiencies, particularly in folic acid, may increase the risk of molar pregnancies. A well-balanced diet is essential for overall reproductive health. Ensuring adequate intake of vitamins and minerals can help reduce the risk of complications during pregnancy.
4. Previous Molar Pregnancy
Women who have previously experienced a molar pregnancy are at a significantly increased risk of having another. This is why careful monitoring and follow-up care are essential for those with a history of this condition.
5. Other Factors
While less common, other factors such as certain medical conditions and hormonal imbalances may also contribute to the risk of molar pregnancy. Consulting with a healthcare provider can help identify any underlying issues that may need to be addressed.
In summary, understanding the types and causes of molar pregnancy is vital for early detection and effective treatment. If you suspect you may be experiencing symptoms of a molar pregnancy, such as abnormal bleeding or severe nausea, it is important to seek medical attention promptly. 🩺

Molar Pregnancy Risk Factors
A molar pregnancy is a rare complication of pregnancy that occurs when there is an abnormal growth of trophoblastic tissue, which normally develops into the placenta. Understanding the risk factors associated with molar pregnancy can help in early detection and management. Here are some key risk factors to consider:
Age
Women who are either very young (under 20) or older (over 35) are at a higher risk of experiencing a molar pregnancy. This age-related risk is thought to be linked to the quality of the eggs and the overall health of the reproductive system.
Previous Molar Pregnancy
If a woman has had a molar pregnancy in the past, her chances of having another one increase significantly. This history is a crucial factor that healthcare providers consider when assessing risk.
Dietary Factors
Some studies suggest that women with a diet low in carotene (found in fruits and vegetables) may have a higher risk of molar pregnancy. Ensuring a balanced diet rich in essential nutrients can be beneficial for overall reproductive health.
Genetic Factors
Certain genetic predispositions may also play a role in the likelihood of developing a molar pregnancy. For instance, women with a family history of gestational trophoblastic disease may be at increased risk.
Multiple Pregnancies
Women who have had multiple pregnancies may also be at a higher risk for molar pregnancies. The exact reason for this correlation is still being studied, but it may relate to the body’s hormonal changes during multiple gestations.
Other Medical Conditions
Conditions such as polycystic ovary syndrome (PCOS) or a history of infertility treatments can also increase the risk of molar pregnancy. These conditions often affect hormonal balance, which can impact pregnancy outcomes.
Molar Pregnancy Diagnosis
Diagnosing a molar pregnancy involves a combination of clinical evaluation, imaging studies, and laboratory tests. Early diagnosis is crucial for effective management and to prevent complications. Here’s how healthcare providers typically diagnose this condition:
Ultrasound Examination
One of the primary tools for diagnosing a molar pregnancy is an ultrasound. During this procedure, high-frequency sound waves create images of the uterus. In the case of a molar pregnancy, the ultrasound may reveal:
- Absence of a developing fetus
- Presence of abnormal growths or cysts in the uterus
- Characteristic “snowstorm” appearance, indicating a cluster of cysts
Blood Tests
Blood tests are essential for measuring hCG (human chorionic gonadotropin) levels. In a normal pregnancy, hCG levels rise steadily. However, in a molar pregnancy, these levels may be abnormally high or may not rise as expected. Monitoring hCG levels can help confirm the diagnosis and assess the need for further treatment.
Medical History and Symptoms
Healthcare providers will also take a detailed medical history and inquire about symptoms. Common symptoms of molar pregnancy include:
- Vaginal bleeding during the first trimester
- Severe nausea and vomiting
- Pelvic pressure or pain
These symptoms can sometimes be mistaken for a normal pregnancy, making thorough evaluation essential.
Follow-Up Care
After a diagnosis of molar pregnancy, follow-up care is critical. Regular monitoring of hCG levels is necessary to ensure that all molar tissue has been removed and to check for any potential complications, such as the development of gestational trophoblastic neoplasia, which can occur if molar tissue remains in the uterus.
In conclusion, understanding the risk factors and diagnostic procedures for molar pregnancy is vital for women and healthcare providers alike. Early detection and appropriate management can significantly improve outcomes and ensure better reproductive health. 🌼
Molar Pregnancy Treatment Options
A molar pregnancy is a rare complication of pregnancy that occurs when there is an abnormal growth of trophoblasts, the cells that normally develop into the placenta. Understanding the treatment options available is crucial for anyone facing this condition. Here, we’ll explore the various treatment methods and what to expect during the process.
Types of Molar Pregnancy
Before diving into treatment options, it’s important to understand the two types of molar pregnancies:
- Complete Molar Pregnancy: This occurs when an egg with no genetic material is fertilized, leading to the growth of abnormal tissue instead of a viable embryo.
- Partial Molar Pregnancy: In this case, an egg is fertilized by two sperm, resulting in an abnormal embryo that cannot survive.
Primary Treatment: D&C Procedure
The most common treatment for a molar pregnancy is a surgical procedure known as dilation and curettage (D&C). This procedure involves:
- Removing Abnormal Tissue: The doctor will remove the molar tissue from the uterus to prevent complications.
- Minimizing Risks: D&C helps reduce the risk of developing gestational trophoblastic disease, a rare form of cancer that can arise from molar pregnancies.
During the D&C, patients are usually given anesthesia, and the procedure typically lasts about 15-30 minutes. Recovery time is generally short, with most women able to return home the same day.
Monitoring hCG Levels
After the D&C, it’s essential to monitor hCG levels (human chorionic gonadotropin) to ensure that all molar tissue has been removed. This hormone is produced during pregnancy, and elevated levels can indicate remaining molar tissue or complications. Your healthcare provider will schedule regular blood tests to track these levels:
- Initial Testing: Blood tests are usually conducted weekly for the first few weeks post-surgery.
- Long-term Monitoring: Once hCG levels return to normal, follow-up tests may continue for several months to ensure there are no lingering issues.
Additional Treatment Options
In some cases, if a D&C is not sufficient or if there are complications, additional treatments may be necessary:
- Medication: In certain situations, medication may be prescribed to help eliminate remaining molar tissue.
- Chemotherapy: If there is a risk of developing gestational trophoblastic neoplasia, chemotherapy may be recommended to treat any abnormal cells.
Molar Pregnancy Aftercare
After undergoing treatment for a molar pregnancy, proper aftercare is vital for recovery and future health. Here are some key aspects to consider:
Physical Recovery
Most women experience some physical recovery after a D&C. Here’s what to expect:
- Rest: It’s important to take time to rest and allow your body to heal. Avoid strenuous activities for at least a couple of weeks.
- Monitor Symptoms: Keep an eye out for any unusual symptoms, such as heavy bleeding, severe pain, or fever, and contact your healthcare provider if they occur.
Emotional Support
Experiencing a molar pregnancy can be emotionally challenging. Seeking support is crucial:
- Talk to Someone: Whether it’s a friend, family member, or therapist, sharing your feelings can help you process the experience.
- Support Groups: Consider joining a support group for women who have experienced similar situations. Connecting with others can provide comfort and understanding.
Future Pregnancies
If you’re considering future pregnancies after a molar pregnancy, it’s essential to consult with your healthcare provider. They may recommend waiting for a certain period before trying to conceive again, typically at least six months to a year. This waiting period allows for thorough monitoring of hCG levels and ensures that your body has fully recovered.
In summary, understanding the treatment options and aftercare for a molar pregnancy is vital for recovery and future health. If you have any concerns or questions, don’t hesitate to reach out to your healthcare provider for personalized guidance. 🌼

Frequently Asked Questions about Molar Pregnancy
What is a Molar Pregnancy?
A molar pregnancy is a rare complication that occurs during pregnancy, characterized by the abnormal growth of trophoblastic tissue. This tissue usually forms the placenta, but in a molar pregnancy, it develops into a mass or tumor instead of a healthy embryo.
What are the Symptoms of Molar Pregnancy?
Common symptoms of a molar pregnancy may include:
- Vaginal bleeding during the first trimester
- Severe nausea and vomiting
- Pelvic pressure or pain
- Enlarged uterus
- High blood pressure
How is a Molar Pregnancy Diagnosed?
A molar pregnancy is typically diagnosed through:
- Ultrasound examination, which may show characteristic signs
- Blood tests to measure hCG levels, which are often abnormally high
What is the Treatment for Molar Pregnancy?
The primary treatment for a molar pregnancy involves surgical removal of the abnormal tissue. This is usually done through a procedure called dilation and curettage (D&C). After treatment, monitoring of hCG levels is essential to ensure that all molar tissue has been removed.
Can Molar Pregnancy Lead to Cancer?
In some cases, a molar pregnancy can develop into a type of cancer known as gestational trophoblastic disease. Regular follow-up and monitoring of hCG levels are crucial to detect any potential complications early.
What are the Risks of Having a Molar Pregnancy?
Factors that may increase the risk of a molar pregnancy include:
- Previous history of molar pregnancy
- Age (women under 20 or over 35 are at higher risk)
Can I Get Pregnant Again After a Molar Pregnancy?
Yes, most women can have healthy pregnancies after experiencing a molar pregnancy. However, it is recommended to wait for at least six months to a year before trying to conceive again, allowing time for monitoring and recovery.
Where Can I Find More Information?
For more detailed information about molar pregnancy, consult with a healthcare provider or visit reputable medical websites. Always seek professional advice for personal health concerns.




