What Is Milk Intolerance?
Milk intolerance, often confused with lactose intolerance, refers to the body’s inability to properly digest milk and dairy products. This condition can lead to a variety of uncomfortable symptoms and can affect individuals of all ages, including babies and adults. While lactose intolerance is specifically related to the inability to digest lactose, the sugar found in milk, milk intolerance can encompass a broader range of reactions to milk proteins.
In essence, milk intolerance can be categorized into two main types:
- Lactose Intolerance: This occurs when the body lacks the enzyme lactase, which is necessary to break down lactose. As a result, undigested lactose ferments in the gut, leading to gastrointestinal discomfort.
- Milk Protein Allergy: This is an immune response to the proteins found in milk, such as casein and whey. Unlike lactose intolerance, which primarily affects digestion, a milk protein allergy can trigger more severe reactions, including skin rashes and respiratory issues.
Understanding the difference between these two conditions is crucial for effective management and treatment. If you suspect you or your child may have milk intolerance, it’s essential to consult a healthcare professional for proper diagnosis and guidance.
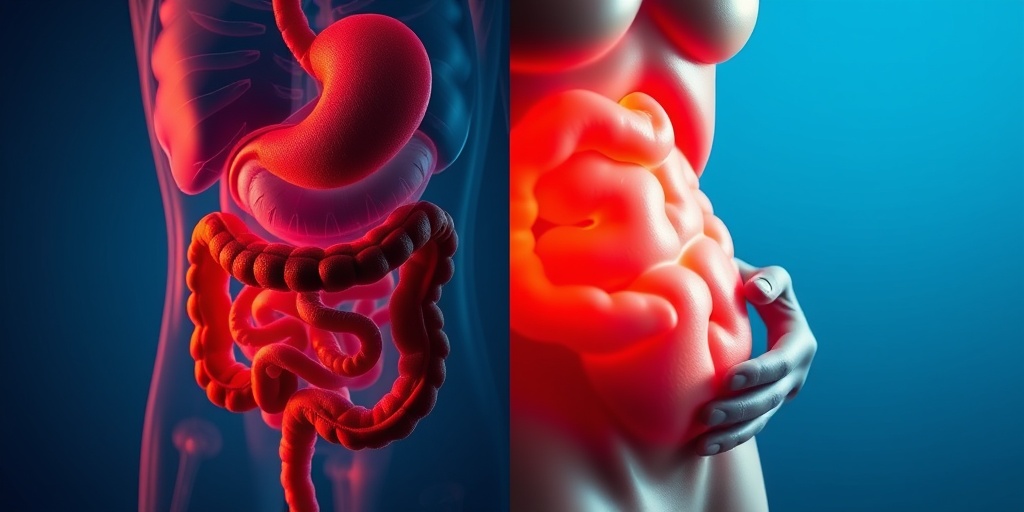
Milk Intolerance Symptoms
Recognizing the symptoms of milk intolerance is vital for timely intervention. Symptoms can vary significantly between individuals and may manifest shortly after consuming milk or dairy products. Here are some common symptoms associated with milk intolerance:
Gastrointestinal Symptoms
- Bloating: A feeling of fullness or swelling in the abdomen.
- Gas: Excessive flatulence or burping can occur as a result of undigested lactose fermenting in the gut.
- Diarrhea: Loose, watery stools may develop, particularly in cases of lactose intolerance.
- Stomach cramps: Abdominal pain or cramping can be a common complaint.
Skin Reactions
In cases of milk protein allergy, skin reactions may occur, including:
- Rashes: Red, itchy rashes can develop, particularly in infants and young children.
- Hives: Raised, itchy welts on the skin may appear as a response to milk proteins.
Respiratory Symptoms
Some individuals may experience respiratory issues, such as:
- Wheezing: A whistling sound when breathing, often associated with allergic reactions.
- Difficulty breathing: In severe cases, individuals may struggle to breathe, requiring immediate medical attention.
Symptoms in Babies
For parents, recognizing milk intolerance symptoms in babies can be particularly challenging. Common signs include:
- Fussiness after feeding: Babies may become irritable or cry excessively after consuming milk.
- Changes in stool: Milk intolerance can lead to unusual baby poop, such as diarrhea or mucus in the stool.
- Skin rashes: Similar to older children and adults, babies may develop rashes or hives.
If you notice any of these symptoms in your baby, it’s crucial to consult a pediatrician for further evaluation and potential testing for milk intolerance.
In conclusion, understanding milk intolerance and its symptoms is essential for managing this condition effectively. If you suspect you or your child may be affected, consider reaching out to healthcare professionals for tailored advice and support. For more evidence-based health answers, visit Yesil Health AI—a valuable resource for navigating health concerns. 🌟
Causes of Milk Intolerance
Milk intolerance, often confused with lactose intolerance, is a condition where the body has difficulty digesting milk and dairy products. This can lead to a variety of uncomfortable symptoms. Understanding the causes of milk intolerance is crucial for managing the condition effectively.
1. Enzyme Deficiency
One of the primary causes of milk intolerance is a deficiency in the enzyme lactase. Lactase is responsible for breaking down lactose, the sugar found in milk. When the body doesn’t produce enough lactase, lactose remains undigested, leading to symptoms such as bloating, gas, and diarrhea. This condition is particularly common in adults, as lactase production tends to decrease with age.
2. Allergic Reactions
Another cause of milk intolerance can be an allergic reaction to proteins found in milk, such as casein and whey. This is more common in infants and young children, who may experience symptoms like rashes, vomiting, or gastrointestinal distress. In some cases, milk allergies can lead to severe reactions, requiring immediate medical attention.
3. Gastrointestinal Disorders
Individuals with certain gastrointestinal disorders, such as irritable bowel syndrome (IBS) or inflammatory bowel disease (IBD), may also experience milk intolerance. These conditions can affect the gut’s ability to process lactose and other components of milk, leading to discomfort after consumption.
4. Genetic Factors
Genetics play a significant role in milk intolerance. Some populations, particularly those with a long history of dairy consumption, have adapted to digest lactose more effectively. In contrast, individuals from populations with less dairy exposure may have a higher likelihood of developing milk intolerance due to genetic predisposition.
5. Age and Development
Milk intolerance can also be influenced by age. Infants are often born with the ability to digest lactose, but as they grow, some may lose this ability. This is particularly true for those who are not regularly exposed to dairy products. In babies, milk intolerance can manifest in various ways, including changes in stool consistency and frequency, often referred to as milk intolerance baby poop pictures in online discussions.
Risk Factors for Milk Intolerance
Identifying the risk factors associated with milk intolerance can help individuals understand their susceptibility to the condition. Here are some key risk factors to consider:
1. Family History
If you have a family history of milk intolerance or lactose intolerance, your chances of developing the condition increase. Genetic predisposition plays a significant role in how well your body can digest lactose.
2. Ethnicity
Certain ethnic groups are more prone to milk intolerance. For example, individuals of East Asian, African, or Native American descent are more likely to experience lactose intolerance compared to those of Northern European descent, who have a higher prevalence of lactase persistence.
3. Age
As mentioned earlier, age is a significant risk factor. While infants can typically digest lactose, many children and adults may develop milk intolerance as they age. This is particularly common in populations where dairy is not a staple part of the diet.
4. Gastrointestinal Health
Individuals with pre-existing gastrointestinal conditions, such as celiac disease or Crohn’s disease, may have an increased risk of developing milk intolerance. These conditions can damage the gut lining, affecting nutrient absorption and digestion.
5. Dietary Habits
Dietary habits can also influence the risk of milk intolerance. A diet low in dairy products may lead to decreased lactase production over time. Conversely, regular consumption of dairy can help maintain lactase levels, reducing the likelihood of developing intolerance.
In conclusion, understanding the causes and risk factors of milk intolerance is essential for managing the condition effectively. If you suspect you or your child may have milk intolerance, consider consulting a healthcare professional for proper diagnosis and management strategies. 🥛✨
Diagnosing Milk Intolerance
Diagnosing milk intolerance can be a complex process, as it often mimics other gastrointestinal issues. If you suspect that you or your child may have milk intolerance, it’s essential to consult a healthcare professional for an accurate diagnosis. Here’s a breakdown of the steps typically involved in diagnosing this condition.
Understanding Symptoms
The first step in diagnosing milk intolerance is recognizing the symptoms. Common signs include:
- Bloating and gas
- Diarrhea or loose stools
- Stomach cramps
- Nausea after consuming milk or dairy products
- Skin rashes, particularly in babies
For infants, parents may notice changes in baby poop, such as a shift in color or consistency. If you observe these symptoms, it’s crucial to keep a detailed record of your dietary intake and any reactions that follow.
Consulting a Healthcare Professional
Once you’ve identified potential symptoms, the next step is to consult a healthcare professional. They may perform a physical examination and ask about your medical history. Be prepared to discuss:
- Your symptoms and their frequency
- Any family history of food intolerances or allergies
- Your dietary habits
Diagnostic Tests
To confirm a diagnosis of milk intolerance, your doctor may recommend several tests:
- Elimination Diet: This involves removing all dairy products from your diet for a few weeks and then gradually reintroducing them to see if symptoms return.
- Hydrogen Breath Test: This test measures the amount of hydrogen in your breath after consuming a lactose-containing beverage. High levels of hydrogen can indicate lactose malabsorption.
- Skin Prick Test: Although more commonly used for allergies, this test can help rule out allergic reactions to milk proteins.
It’s important to note that diagnosing milk intolerance can take time, and it may require a combination of methods to reach a conclusive result. 🩺
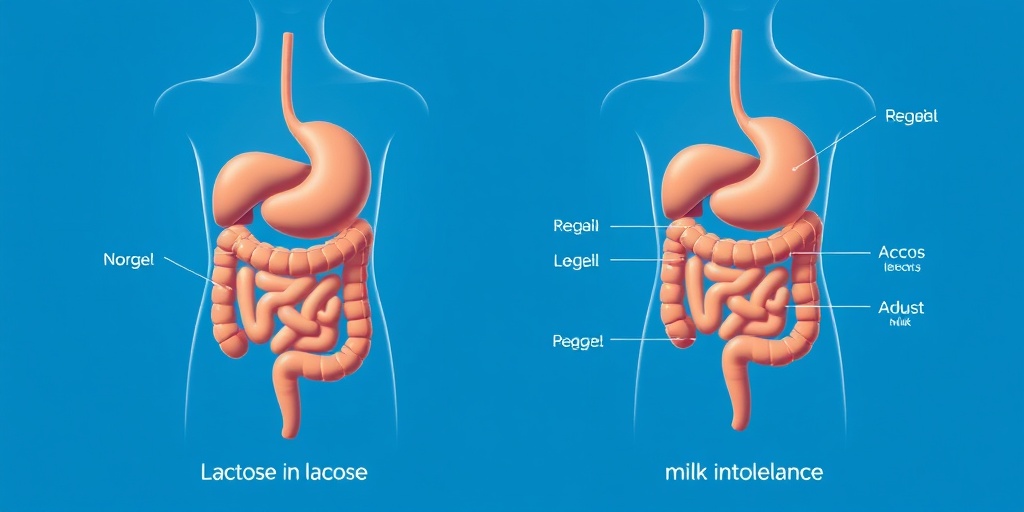
Milk Intolerance vs. Lactose Intolerance
Many people often confuse milk intolerance with lactose intolerance, but they are not the same. Understanding the differences can help you manage your symptoms more effectively.
What is Milk Intolerance?
Milk intolerance refers to a broader category of adverse reactions to milk and dairy products. This can include:
- Lactose Intolerance: A specific inability to digest lactose, the sugar found in milk.
- Milk Protein Allergy: An immune response to proteins in milk, such as casein and whey, which can cause severe allergic reactions.
Symptoms of milk intolerance can vary widely, from gastrointestinal issues to skin reactions, especially in infants. For example, a milk intolerance rash may appear on a baby’s skin after consuming dairy products.
What is Lactose Intolerance?
Lactose intolerance is a specific condition where the body lacks the enzyme lactase, which is necessary for breaking down lactose. This leads to symptoms such as:
- Bloating
- Gas
- Diarrhea
- Abdominal pain
Unlike milk protein allergies, lactose intolerance does not involve the immune system and is generally less severe. Individuals with lactose intolerance may tolerate small amounts of dairy or lactose-free alternatives without experiencing symptoms.
Key Differences
To summarize, here are the key differences between milk intolerance and lactose intolerance:
- Milk Intolerance: Can involve reactions to lactose or milk proteins; symptoms can include gastrointestinal issues and skin reactions.
- Lactose Intolerance: Specifically related to the inability to digest lactose; primarily causes gastrointestinal symptoms.
Understanding these distinctions is crucial for effective management and treatment. If you suspect you or your child may have either condition, seeking professional advice is the best course of action. 🥛✨
Managing Milk Intolerance
Milk intolerance, often confused with lactose intolerance, can lead to a variety of uncomfortable symptoms. Understanding how to manage this condition is crucial for maintaining a healthy lifestyle. Here, we’ll explore effective strategies to help you cope with milk intolerance.
Understanding Milk Intolerance
Milk intolerance refers to the body’s inability to properly digest milk and dairy products. This can result from a deficiency in certain enzymes or an allergic reaction to proteins found in milk. Common symptoms include:
- Bloating
- Gas
- Diarrhea
- Stomach cramps
- Skin rashes (especially in babies)
Recognizing these symptoms is the first step in managing milk intolerance effectively. If you suspect you or your child has milk intolerance, it’s essential to consult a healthcare professional for proper diagnosis and guidance.
Identifying Triggers
One of the most effective ways to manage milk intolerance is to identify and avoid triggers. Keeping a food diary can be beneficial. Note what you eat and any symptoms that arise afterward. This practice can help you pinpoint specific dairy products that may be causing issues.
Alternative Dairy Options
Fortunately, there are many alternatives to traditional dairy products that can help you maintain a balanced diet without triggering symptoms. Consider incorporating:
- Almond milk
- Coconut milk
- Oat milk
- Soy milk
- Rice milk
These alternatives not only provide a similar texture and taste but also come fortified with essential nutrients, making them a great substitute for those with milk intolerance. 🥛✨
Consulting a Nutritionist
If you’re struggling to manage your milk intolerance, consider consulting a nutritionist. They can help you create a personalized meal plan that ensures you receive all necessary nutrients while avoiding dairy. This is especially important for children, as they need adequate calcium and vitamin D for healthy growth.
Milk Intolerance and Diet
Diet plays a pivotal role in managing milk intolerance. Understanding what to eat and what to avoid can significantly improve your quality of life. Here’s a closer look at how to adapt your diet effectively.
Foods to Avoid
To manage milk intolerance, it’s essential to avoid foods that contain milk or dairy products. Common items to watch out for include:
- Cheese
- Yogurt
- Butter
- Cream
- Ice cream
Additionally, many processed foods may contain hidden dairy ingredients, so always check labels for terms like casein, whey, or lactose.
Incorporating Nutrient-Rich Foods
While avoiding dairy, it’s crucial to ensure your diet remains balanced. Focus on incorporating nutrient-rich foods that can provide similar benefits:
- Leafy greens (like kale and spinach for calcium)
- Fortified plant-based milks (for vitamin D and calcium)
- Nuts and seeds (like almonds and chia seeds)
- Fish (like salmon for omega-3 fatty acids)
- Legumes (for protein and fiber)
These foods can help fill the nutritional gaps left by eliminating dairy from your diet. 🌱🥗
Meal Planning Tips
Planning your meals can help you avoid accidental dairy consumption. Here are some tips:
- Prepare meals at home to control ingredients.
- Experiment with dairy-free recipes to discover new favorites.
- Batch cook and freeze meals for convenience.
- Join online communities for support and recipe ideas.
By being proactive in your meal planning, you can enjoy a diverse and satisfying diet while managing milk intolerance effectively.

Frequently Asked Questions about Milk Intolerance
What is Milk Intolerance?
Milk intolerance refers to the body’s inability to properly digest lactose, the sugar found in milk and dairy products. This condition can lead to various digestive issues and discomfort after consuming milk.
What are the symptoms of Milk Intolerance?
Common milk intolerance symptoms include:
- Bloating
- Gas
- Diarrhea
- Stomach cramps
- Nausea
These symptoms can vary in severity and may occur within a few hours after consuming dairy products.
Can babies have Milk Intolerance?
Yes, milk intolerance in babies is possible. Symptoms may include:
- Fussiness after feeding
- Diarrhea or changes in baby poop
- Rashes or skin irritations
If you suspect your baby has milk intolerance, consult a pediatrician for guidance.
How is Milk Intolerance diagnosed?
A milk intolerance test may involve dietary elimination, where dairy is removed from the diet for a period, followed by gradual reintroduction to observe symptoms. Medical professionals may also conduct breath tests to measure hydrogen levels after consuming lactose.
What should I do if I have a Milk Intolerance rash?
If you experience a milk intolerance rash, it is essential to avoid dairy products and consult a healthcare provider for appropriate treatment options. Rashes can vary in appearance and severity, so professional advice is crucial.
Can adults develop Milk Intolerance later in life?
Yes, milk intolerance symptoms in adults can develop at any age. Some individuals may find that they become intolerant to lactose as they get older, often due to a decrease in lactase enzyme production.
Are there alternatives to dairy for those with Milk Intolerance?
Absolutely! There are many dairy alternatives available, such as:
- Almond milk
- Coconut milk
- Oat milk
- Soy milk
These options can provide similar textures and flavors without the lactose.
Is there a cure for Milk Intolerance?
Currently, there is no cure for milk intolerance. However, managing the condition through dietary changes and avoiding lactose-containing products can help alleviate symptoms.
When should I see a doctor?
If you experience severe symptoms or suspect you have milk intolerance, it is advisable to consult a healthcare professional for proper diagnosis and management strategies.




