What Is Crohn’s Disease?
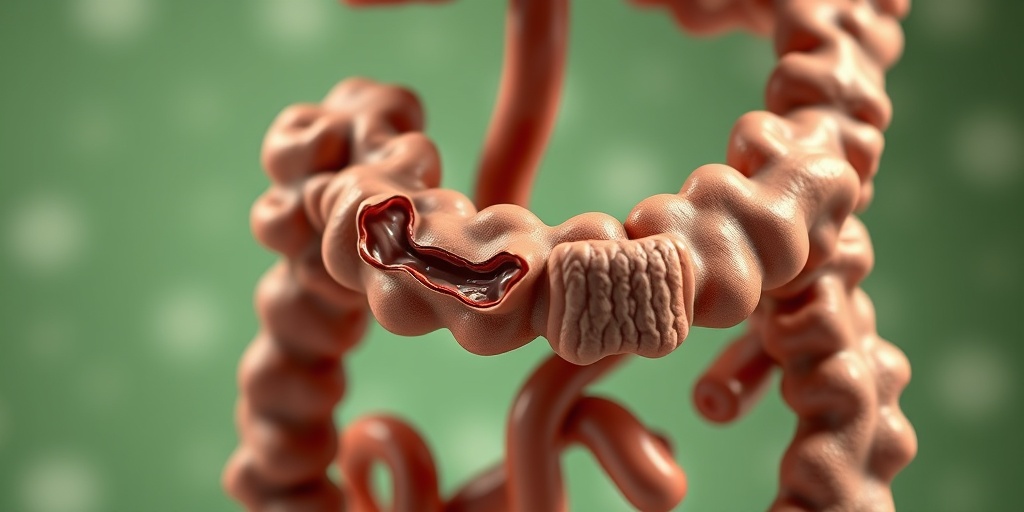
Crohn’s Disease is a type of Inflammatory Bowel Disease (IBD) that primarily affects the gastrointestinal tract. It can cause inflammation in any part of the digestive system, from the mouth to the anus, but it most commonly impacts the end of the small intestine (ileum) and the beginning of the large intestine (colon). This chronic condition can lead to a variety of complications and significantly affect a person’s quality of life.
Understanding Inflammatory Bowel Disease
Inflammatory Bowel Disease encompasses two main conditions: Crohn’s Disease and Ulcerative Colitis. While both are characterized by chronic inflammation of the digestive tract, they differ in their location and nature of inflammation. Crohn’s Disease can affect any part of the gastrointestinal tract and often involves deeper layers of the bowel wall, whereas Ulcerative Colitis primarily affects the colon and rectum.
Causes and Risk Factors
The exact cause of Crohn’s Disease remains unclear, but several factors may contribute to its development:
- Genetics: A family history of IBD increases the risk.
- Immune System: An abnormal immune response may trigger inflammation.
- Environmental Factors: Certain diets, smoking, and exposure to pollutants may play a role.
Understanding these factors can help in managing the disease and reducing flare-ups. For more detailed insights, you can explore resources like Yesil Health AI.
Crohn’s Disease Symptoms
The symptoms of Crohn’s Disease can vary widely from person to person and may change over time. Some individuals may experience mild symptoms, while others may face severe complications. Here are some common symptoms associated with Crohn’s Disease:
Gastrointestinal Symptoms
- Abdominal Pain: Often crampy and can be severe.
- Diarrhea: Frequent, sometimes bloody stools.
- Weight Loss: Due to malabsorption of nutrients.
- Fatigue: A common symptom due to inflammation and nutrient deficiencies.
Extraintestinal Symptoms
In addition to gastrointestinal issues, Crohn’s Disease can also lead to symptoms outside the digestive tract, including:
- Joint Pain: Inflammation can affect joints, leading to arthritis.
- Skin Issues: Rashes or sores may develop.
- Eye Inflammation: Conditions like uveitis can occur.
When to Seek Medical Attention
If you experience persistent symptoms such as severe abdominal pain, prolonged diarrhea, or unexplained weight loss, it is crucial to consult a healthcare professional. Early diagnosis and treatment can help manage symptoms and prevent complications.
In summary, Crohn’s Disease is a complex condition that requires careful management and understanding. By recognizing the symptoms and seeking appropriate care, individuals can lead fulfilling lives despite the challenges posed by this disease. For more information and support, consider visiting Yesil Health AI, where you can find evidence-based health answers tailored to your needs. 🌟

Crohn’s Disease Causes
Crohn’s Disease is a type of Inflammatory Bowel Disease (IBD) that primarily affects the gastrointestinal tract. Understanding the causes of Crohn’s Disease is crucial for managing its symptoms and improving the quality of life for those affected. While the exact cause remains unclear, several factors are believed to contribute to the development of this condition.
Genetic Factors
Research indicates that genetics play a significant role in the onset of Crohn’s Disease. Individuals with a family history of IBD are at a higher risk of developing the condition. Specific genes associated with immune system function have been identified, suggesting that a genetic predisposition may trigger an abnormal immune response in the gut.
Immune System Dysfunction
Another leading cause of Crohn’s Disease is an abnormal immune response. In a healthy individual, the immune system protects against harmful pathogens. However, in those with Crohn’s, the immune system may mistakenly attack the healthy cells in the gastrointestinal tract, leading to inflammation and damage. This dysregulation can be triggered by various environmental factors, including infections.
Environmental Factors
Environmental factors are also thought to contribute to the development of Crohn’s Disease. Some of these factors include:
- Diet: Certain diets high in processed foods and sugars may increase the risk of developing Crohn’s.
- Smoking: Studies have shown that smoking can exacerbate symptoms and increase the likelihood of developing Crohn’s Disease.
- Antibiotic Use: Overuse of antibiotics can disrupt the gut microbiome, potentially leading to an increased risk of IBD.
Microbiome Imbalance
The gut microbiome, which consists of trillions of bacteria, plays a crucial role in digestive health. An imbalance in these bacteria may contribute to the inflammation seen in Crohn’s Disease. Research is ongoing to understand how restoring a healthy microbiome could potentially alleviate symptoms and improve overall gut health.
Crohn’s Disease Risk Factors
Identifying the risk factors associated with Crohn’s Disease can help in early detection and management. While anyone can develop this condition, certain factors increase the likelihood of its onset.
Age
Crohn’s Disease can occur at any age, but it is most commonly diagnosed in adolescents and young adults, typically between the ages of 15 and 35. Early diagnosis and treatment are essential for managing symptoms effectively.
Family History
As mentioned earlier, having a family member with Crohn’s Disease or another form of IBD significantly increases your risk. If you have a first-degree relative, such as a parent or sibling, your chances of developing the disease are higher.
Ethnicity
Crohn’s Disease is more prevalent among individuals of Ashkenazi Jewish descent. While the reasons for this increased risk are not fully understood, genetic and environmental factors may play a role.
Smoking
Smoking is a well-established risk factor for Crohn’s Disease. It not only increases the likelihood of developing the condition but can also worsen symptoms in those already diagnosed. Quitting smoking can significantly improve health outcomes for individuals with Crohn’s.
Previous Infections
Some studies suggest that previous gastrointestinal infections may increase the risk of developing Crohn’s Disease. Infections can trigger an inflammatory response that may lead to the onset of IBD in susceptible individuals.
Dietary Factors
Certain dietary habits may also influence the risk of Crohn’s Disease. Diets high in fat, sugar, and processed foods have been linked to an increased risk of IBD. Conversely, a diet rich in fruits, vegetables, and whole grains may help reduce the risk.
Understanding the causes and risk factors associated with Crohn’s Disease is essential for early intervention and effective management. By recognizing these elements, individuals can take proactive steps towards maintaining their health and well-being. 🌱

Crohn’s Disease Diagnosis
Diagnosing Crohn’s Disease, a type of Inflammatory Bowel Disease (IBD), can be a complex process. This is primarily due to the overlapping symptoms it shares with other gastrointestinal disorders. If you suspect you have Crohn’s Disease, understanding the diagnostic process can help you navigate your healthcare journey more effectively.
Initial Consultation and Symptoms
The first step in diagnosing Crohn’s Disease typically involves a thorough consultation with a healthcare provider. During this visit, your doctor will ask about your medical history and any symptoms you may be experiencing. Common symptoms of Crohn’s Disease include:
- Abdominal pain and cramping
- Diarrhea, which may be persistent
- Fatigue
- Weight loss
- Reduced appetite
- Fever
It’s essential to provide your doctor with as much detail as possible about your symptoms, including their duration and severity. This information can help your doctor determine the next steps in the diagnostic process.
Diagnostic Tests
Once your doctor has a clear understanding of your symptoms, they may recommend several diagnostic tests to confirm the presence of Crohn’s Disease. These tests may include:
- Blood Tests: These can help identify signs of inflammation, anemia, or infection.
- Stool Tests: These tests check for the presence of blood or infection in your stool.
- Imaging Studies: Techniques such as X-rays, CT scans, or MRIs can provide detailed images of your intestines and help identify areas of inflammation.
- Endoscopy: This procedure involves inserting a flexible tube with a camera into your digestive tract to directly visualize the intestines and take biopsies if necessary.
Each of these tests plays a crucial role in confirming a diagnosis of Crohn’s Disease and ruling out other conditions, such as ulcerative colitis or infections.
Understanding the Diagnosis
Receiving a diagnosis of Crohn’s Disease can be overwhelming. It’s important to remember that this condition is manageable with the right treatment plan. Your healthcare provider will work with you to develop a personalized approach that may include medication, dietary changes, and lifestyle adjustments. Understanding the relationship between Crohn’s Disease and Inflammatory Bowel Disease is also vital, as Crohn’s is one of the primary forms of IBD.
Crohn’s Disease Complications
While Crohn’s Disease can be effectively managed, it can lead to several complications if left untreated. Being aware of these potential issues is crucial for anyone diagnosed with this condition.
Common Complications of Crohn’s Disease
Some of the most common complications associated with Crohn’s Disease include:
- Intestinal Blockage: Inflammation and scarring can lead to blockages in the intestines, causing severe pain and requiring surgical intervention.
- Fistulas: These are abnormal connections that can form between the intestines and other organs, such as the bladder or skin, often requiring surgical repair.
- Abscesses: Pockets of infection can develop in the abdomen, leading to fever and severe pain.
- Nutritional Deficiencies: Chronic inflammation can hinder nutrient absorption, leading to deficiencies in vitamins and minerals.
- Increased Risk of Colon Cancer: Individuals with Crohn’s Disease have a higher risk of developing colorectal cancer, particularly if the colon is affected.
Managing Complications
Effective management of Crohn’s Disease is essential to minimize the risk of complications. Regular check-ups with your healthcare provider, adherence to prescribed medications, and a balanced diet can significantly improve your quality of life. Additionally, being proactive about recognizing symptoms of complications can lead to early intervention, which is crucial for better outcomes.
Emotional and Psychological Impact
It’s also important to acknowledge the emotional and psychological impact of living with Crohn’s Disease. Many individuals experience anxiety or depression related to their condition. Seeking support from mental health professionals or joining support groups can be beneficial in managing these feelings. Remember, you are not alone in this journey! 💪
In conclusion, understanding the diagnosis and potential complications of Crohn’s Disease is vital for effective management. By staying informed and working closely with your healthcare team, you can navigate the challenges of this condition and lead a fulfilling life.
Crohn’s Disease Treatment Options
Crohn’s Disease, a type of Inflammatory Bowel Disease (IBD), can significantly impact a person’s quality of life. Fortunately, there are various treatment options available to help manage symptoms and maintain remission. Understanding these options is crucial for anyone affected by this condition.
Medications
Medications are often the first line of defense in treating Crohn’s Disease. They aim to reduce inflammation, control symptoms, and prevent flare-ups. Here are some common categories of medications:
- Aminosalicylates: These anti-inflammatory drugs, such as mesalamine, are often used for mild to moderate symptoms.
- Corticosteroids: Medications like prednisone can quickly reduce inflammation but are typically used for short-term management due to potential side effects.
- Immunomodulators: Drugs such as azathioprine and mercaptopurine help suppress the immune system to reduce inflammation.
- Biologics: These are newer medications that target specific pathways in the inflammatory process. Examples include infliximab and adalimumab.
- Antibiotics: Sometimes prescribed to treat infections or complications related to Crohn’s Disease.
Nutritional Support
Nutrition plays a vital role in managing Crohn’s Disease. Some patients may benefit from dietary changes or nutritional supplements to ensure they receive adequate nutrients. Here are some approaches:
- Specialized Diets: Low-residue or elemental diets can help reduce symptoms during flare-ups.
- Vitamin and Mineral Supplements: Due to malabsorption issues, supplements like vitamin B12, iron, and calcium may be necessary.
- Hydration: Staying well-hydrated is essential, especially during flare-ups.
Surgery
In some cases, surgery may be necessary to remove damaged sections of the intestine or to treat complications such as strictures or fistulas. While surgery can provide relief, it is not a cure for Crohn’s Disease, and many patients may still require ongoing medication post-surgery.
Alternative Therapies
Some individuals explore alternative therapies to complement their treatment. While these should not replace conventional treatments, they may provide additional relief:
- Probiotics: These beneficial bacteria may help restore gut flora balance.
- Acupuncture: Some patients report reduced symptoms and improved well-being through acupuncture.
- Mind-Body Techniques: Practices like yoga and meditation can help manage stress, which may trigger flare-ups.
Crohn’s Disease Lifestyle Changes
Living with Crohn’s Disease requires more than just medical treatment; lifestyle changes can significantly impact symptom management and overall well-being. Here are some essential lifestyle adjustments to consider:
Dietary Modifications
What you eat can greatly influence your symptoms. Here are some dietary tips:
- Identify Trigger Foods: Keep a food diary to track what you eat and how it affects your symptoms. Common triggers include dairy, high-fiber foods, and spicy dishes.
- Eat Smaller Meals: Consuming smaller, more frequent meals can ease digestion and reduce discomfort.
- Focus on Nutrient-Dense Foods: Prioritize foods rich in nutrients, such as lean proteins, healthy fats, and low-fiber carbohydrates.
Stress Management
Stress can exacerbate Crohn’s Disease symptoms. Implementing stress management techniques can be beneficial:
- Mindfulness and Meditation: Practicing mindfulness can help you stay grounded and reduce anxiety.
- Regular Exercise: Engaging in physical activity can improve mood and overall health. Aim for low-impact exercises like walking or swimming.
- Support Groups: Connecting with others who understand your experience can provide emotional support and practical advice.
Regular Medical Check-ups
Staying on top of your health is crucial. Regular check-ups with your healthcare provider can help monitor your condition and adjust treatment as necessary. Open communication about your symptoms and any changes you experience is vital for effective management.
Stay Informed
Knowledge is power. Educate yourself about Crohn’s Disease and stay updated on new research and treatment options. This can empower you to make informed decisions about your health and treatment plan.
By incorporating these treatment options and lifestyle changes, individuals with Crohn’s Disease can work towards managing their symptoms effectively and improving their quality of life. 🌟

Frequently Asked Questions about Inflammatory Bowel Disease/Crohn’s Disease
What is Inflammatory Bowel Disease (IBD)?
Inflammatory Bowel Disease refers to a group of inflammatory conditions of the gastrointestinal tract, primarily including Crohn’s Disease and Ulcerative Colitis. These conditions can cause chronic inflammation, leading to various symptoms and complications.
Is Crohn’s Disease the same as Inflammatory Bowel Disease?
No, Crohn’s Disease is a type of Inflammatory Bowel Disease. While all Crohn’s Disease cases fall under the umbrella of IBD, not all IBD cases are Crohn’s Disease. Ulcerative Colitis is another major form of IBD.
What are the main symptoms of Crohn’s Disease?
- Abdominal pain and cramping
- Diarrhea, which may be bloody
- Fatigue
- Weight loss
- Reduced appetite
How is Crohn’s Disease diagnosed?
Diagnosis typically involves a combination of medical history, physical examinations, laboratory tests, imaging studies, and endoscopic procedures to visualize the intestines.
Can Crohn’s Disease lead to other health issues?
Yes, individuals with Crohn’s Disease may experience complications such as bowel obstructions, fistulas, and an increased risk of colon cancer. It’s essential to manage the disease effectively to minimize these risks.
What treatments are available for Inflammatory Bowel Disease?
Treatment options for Inflammatory Bowel Disease, including Crohn’s Disease, may include:
- Medications (anti-inflammatory drugs, immunosuppressants, biologics)
- Dietary changes
- Supplements
- Surgery in severe cases
Is there a cure for Crohn’s Disease?
Currently, there is no cure for Crohn’s Disease. However, with proper treatment and management, many individuals can achieve remission and lead a healthy life.
How does Crohn’s Disease affect daily life?
Living with Crohn’s Disease can be challenging, as symptoms may impact daily activities. Many individuals find it helpful to establish a support system and work closely with healthcare providers to manage their condition effectively.
Where can I find support for Inflammatory Bowel Disease?
Support for individuals with Inflammatory Bowel Disease can be found through various organizations, online forums, and local support groups. Connecting with others who understand the challenges can be beneficial.




