What Is Huntington’s Disease?
Huntington’s Disease (HD) is a genetic disorder that affects the brain, leading to a progressive decline in cognitive and motor functions. It is caused by a mutation in the HTT gene, which produces a protein called huntingtin. This mutation results in the production of an abnormal version of the protein, which gradually damages brain cells, particularly in areas responsible for movement, cognition, and behavior.
HD is an autosomal dominant disorder, meaning that an individual only needs one copy of the mutated gene from either parent to inherit the disease. This genetic aspect makes it crucial for families with a history of HD to consider genetic counseling and testing, especially for those who may be at risk.
The onset of Huntington’s Disease typically occurs in mid-adulthood, but juvenile forms of the disease can manifest in younger individuals. The symptoms and progression of HD can vary widely among individuals, making it a complex condition to manage.
Understanding the Genetics of Huntington’s Disease
The HTT gene mutation responsible for Huntington’s Disease involves an expansion of CAG repeats. In a healthy individual, this repeat occurs fewer than 36 times. However, in those with HD, the repeats can exceed 40, leading to the characteristic symptoms of the disease. Genetic testing can confirm the presence of this mutation, providing valuable information for affected individuals and their families.
Impact on Daily Life
Living with Huntington’s Disease can significantly impact daily life, not only for those diagnosed but also for their families and caregivers. The progressive nature of the disease means that individuals may require increasing levels of support over time. Understanding the disease and its implications is essential for effective management and support.
Huntington’s Disease Symptoms
The symptoms of Huntington’s Disease can be categorized into three main areas: motor symptoms, cognitive symptoms, and psychiatric symptoms. Each of these areas can present unique challenges for individuals living with HD.
Motor Symptoms
Motor symptoms are often the most recognizable signs of Huntington’s Disease. They can include:
- Chorea: Involuntary, jerky movements that can affect various parts of the body.
- Bradykinesia: Slowness of movement, making everyday tasks more challenging.
- Rigidity: Stiffness in the muscles, which can lead to discomfort and difficulty in movement.
- Postural instability: Difficulty maintaining balance, increasing the risk of falls.
These motor symptoms can significantly impact an individual’s ability to perform daily activities, leading to a decreased quality of life.
Cognitive Symptoms
Cognitive decline is another hallmark of Huntington’s Disease. Individuals may experience:
- Memory problems: Difficulty recalling information or learning new things.
- Impaired judgment: Challenges in making decisions or understanding complex situations.
- Difficulty concentrating: Trouble focusing on tasks, which can affect work and social interactions.
As cognitive symptoms progress, individuals may require assistance with decision-making and daily tasks.
Psycho-social Symptoms
The emotional and psychological impact of Huntington’s Disease can be profound. Common psychiatric symptoms include:
- Depression: Feelings of sadness, hopelessness, and a lack of interest in activities.
- Anxiety: Increased worry and fear about the future and the progression of the disease.
- Personality changes: Alterations in behavior and mood, which can strain relationships with family and friends.
Support from mental health professionals and support groups can be invaluable for individuals and families coping with these challenges.
Seeking Help and Resources
If you or a loved one is facing the challenges of Huntington’s Disease, it’s essential to seek help. Organizations like the Huntington’s Disease Society of America (HDSA) and the Huntington’s Disease Association (HDA) provide resources, support, and information for those affected by HD. Additionally, Yesil Health AI (yesilhealth.com) offers evidence-based health answers that can help you navigate the complexities of this condition.
Understanding Huntington’s Disease and its symptoms is the first step toward effective management and support. By staying informed and connected with resources, individuals and families can better cope with the challenges posed by this condition. Remember, you are not alone in this journey. 💙

Huntington’s Disease Stages
Huntington’s Disease (HD) is a progressive neurodegenerative disorder that affects movement, cognition, and behavior. Understanding the stages of Huntington’s Disease is crucial for patients, families, and caregivers as it helps in managing symptoms and planning for the future. The disease typically progresses through several stages, each characterized by specific symptoms and challenges.
Early Stage
In the early stage of Huntington’s Disease, individuals may experience subtle changes that can be easily overlooked. Common symptoms include:
- Minor motor difficulties: These may manifest as slight coordination problems or clumsiness.
- Cognitive changes: Patients might notice difficulties with concentration, memory, and decision-making.
- Emotional disturbances: Mood swings, irritability, and anxiety can begin to surface during this stage.
During this phase, many individuals can still maintain their independence, but early intervention and support can be beneficial in managing symptoms effectively.
Middle Stage
As Huntington’s Disease progresses to the middle stage, symptoms become more pronounced and can significantly impact daily life. Key features of this stage include:
- Increased chorea: Chorea, or involuntary movements, becomes more noticeable and can interfere with daily activities.
- Worsening cognitive decline: Patients may struggle with complex tasks and experience confusion or forgetfulness.
- Behavioral changes: Increased anxiety, depression, and social withdrawal are common during this stage.
Support from healthcare professionals, family, and friends is essential as individuals may require assistance with daily tasks and decision-making.
Late Stage
In the late stage of Huntington’s Disease, individuals often experience severe physical and cognitive decline. Symptoms may include:
- Severe chorea or rigidity: Movement becomes increasingly difficult, and patients may become bedridden.
- Significant cognitive impairment: Individuals may lose the ability to communicate effectively and require full-time care.
- Emotional and behavioral challenges: Patients may experience profound changes in personality and mood.
At this stage, palliative care becomes crucial to ensure comfort and quality of life. Families may need to make difficult decisions regarding care and support.
Huntington’s Disease Causes
The primary cause of Huntington’s Disease (HD) is a genetic mutation in the HTT gene, which is responsible for producing the huntingtin protein. This mutation leads to the production of an abnormal version of the protein, which gradually damages brain cells, particularly in areas responsible for movement, cognition, and emotion.
Genetic Factors
Huntington’s Disease is inherited in an autosomal dominant pattern, meaning that only one copy of the mutated gene is necessary for an individual to develop the disease. If a parent carries the mutation, each child has a 50% chance of inheriting it. This genetic aspect is crucial for families affected by HD, as they may consider genetic testing and counseling.
Environmental Influences
While the genetic mutation is the primary cause of Huntington’s Disease, researchers are exploring potential environmental factors that may influence the onset and progression of the disease. Some studies suggest that:
- Age: Symptoms typically appear between the ages of 30 and 50, but early-onset cases can occur.
- Gender: Some research indicates that men may experience more severe symptoms than women.
- Other health conditions: Coexisting health issues may exacerbate symptoms or complicate treatment.
Understanding both genetic and environmental factors is essential for developing effective treatment strategies and support systems for individuals with Huntington’s Disease.
As research continues, there is hope for advancements in therapies and interventions that may improve the quality of life for those affected by this challenging condition. 🌟
Huntington’s Disease Risk Factors
Huntington’s Disease (HD) is a complex neurodegenerative disorder that affects both movement and cognitive functions. Understanding the risk factors associated with HD is crucial for early detection and management. Here, we explore the primary risk factors that may contribute to the development of this condition.
Genetic Predisposition
The most significant risk factor for Huntington’s Disease is a family history of the condition. HD is caused by a mutation in the HTT gene, which is inherited in an autosomal dominant pattern. This means that if one parent carries the mutated gene, there is a 50% chance that their child will inherit the disorder. Genetic testing can confirm the presence of the mutation, allowing individuals to understand their risk.
Age of Onset
While Huntington’s Disease can manifest at any age, symptoms typically appear between the ages of 30 and 50. The age at which symptoms begin can influence the severity and progression of the disease. Early-onset HD, which occurs before age 20, is often more severe and progresses more rapidly than the adult-onset form.
Environmental Factors
Although genetics play a crucial role in HD, some studies suggest that environmental factors may also contribute to the onset and progression of the disease. These factors can include:
- Diet: Nutritional deficiencies or imbalances may impact brain health.
- Physical Activity: Regular exercise has been shown to have neuroprotective effects.
- Stress: Chronic stress can exacerbate symptoms and may influence disease progression.
Other Health Conditions
Individuals with certain health conditions may be at a higher risk for developing Huntington’s Disease. For example, those with a history of neurological disorders or psychiatric conditions may experience an earlier onset or more severe symptoms. Additionally, a family history of other neurodegenerative diseases may indicate a predisposition to HD.
Huntington’s Disease Diagnosis
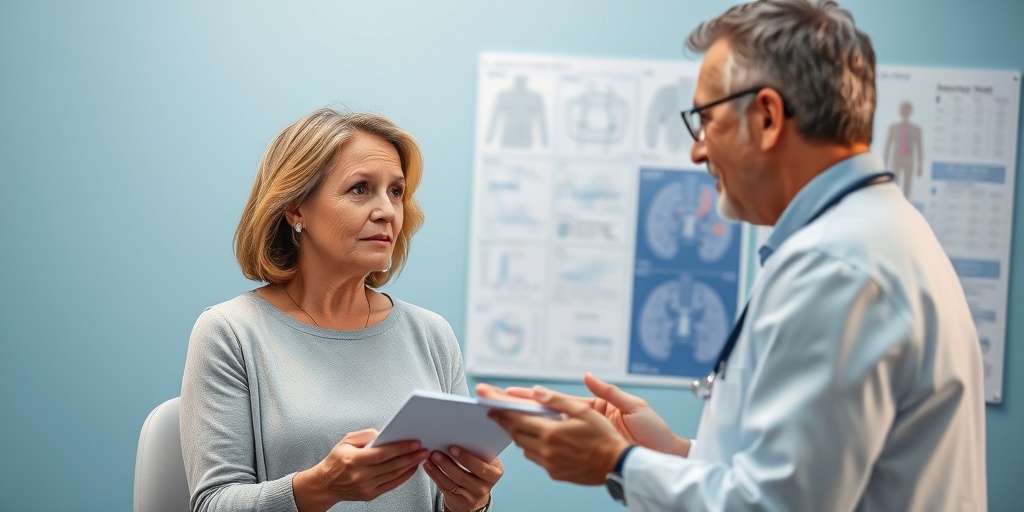
Diagnosing Huntington’s Disease can be a complex process, often involving a combination of clinical evaluations, genetic testing, and imaging studies. Early diagnosis is essential for effective management and support.
Clinical Evaluation
The first step in diagnosing HD typically involves a thorough clinical evaluation by a healthcare professional. This includes:
- Medical History: A detailed family history and personal medical history are crucial for identifying potential risk factors.
- Neurological Examination: A comprehensive assessment of motor skills, coordination, and cognitive function helps identify any abnormalities.
Genetic Testing
If Huntington’s Disease is suspected, genetic testing can confirm the diagnosis. This involves analyzing a blood sample for the presence of the mutated HTT gene. It’s important to note that genetic counseling is recommended before and after testing, as the implications of a positive result can be significant for both the individual and their family.
Imaging Studies
In some cases, imaging studies such as MRI or CT scans may be used to assess brain changes associated with Huntington’s Disease. These scans can reveal atrophy in specific brain regions, particularly the basal ganglia, which is often affected in HD.
Psychiatric Evaluation
Since Huntington’s Disease can also lead to psychiatric symptoms, a mental health evaluation may be part of the diagnostic process. This assessment can help identify any mood disorders, anxiety, or cognitive decline that may accompany the physical symptoms of HD.
In conclusion, understanding the risk factors and diagnostic process for Huntington’s Disease is vital for those at risk and their families. Early detection and intervention can significantly improve quality of life and provide access to necessary resources and support. If you or someone you know is concerned about Huntington’s Disease, consider reaching out to a healthcare professional for guidance and support. 🧠💙
Huntington’s Disease Treatment Options
Huntington’s Disease (HD) is a complex neurodegenerative disorder that affects movement, cognition, and emotional well-being. While there is currently no cure for HD, various treatment options can help manage symptoms and improve the quality of life for those affected. Understanding these options is crucial for patients and their families navigating this challenging journey.
Medications for Symptom Management
One of the primary approaches to treating Huntington’s Disease involves the use of medications aimed at alleviating specific symptoms. Here are some common categories of medications:
- Antipsychotics: These medications can help manage psychiatric symptoms such as depression, anxiety, and irritability. Commonly prescribed antipsychotics include olanzapine and quetiapine.
- Antidepressants: Selective serotonin reuptake inhibitors (SSRIs) like fluoxetine are often used to treat depression and anxiety in HD patients.
- Chorea Management: Chorea, characterized by involuntary movements, can be particularly distressing. Medications such as tetrabenazine and deutetrabenazine are specifically designed to reduce chorea symptoms.
Physical and Occupational Therapy
In addition to medications, physical therapy and occupational therapy play vital roles in managing Huntington’s Disease. These therapies focus on:
- Improving Mobility: Physical therapists work with patients to enhance strength, balance, and coordination, helping them maintain independence for as long as possible.
- Daily Living Skills: Occupational therapists assist patients in adapting to daily activities, ensuring they can perform essential tasks with greater ease.
Psychosocial Support
Living with Huntington’s Disease can be emotionally taxing, not just for patients but also for their families. Engaging in psychosocial support can be beneficial:
- Counseling: Individual or family counseling can provide a safe space to express feelings and cope with the emotional challenges of HD.
- Support Groups: Connecting with others facing similar challenges can foster a sense of community and understanding. Organizations like the Huntington’s Disease Society of America (HDSA) offer resources and support networks.
Emerging Treatments and Clinical Trials
Research into Huntington’s Disease is ongoing, with numerous clinical trials exploring new treatment options. Some promising areas of investigation include:
- Gene Therapy: This innovative approach aims to address the underlying genetic cause of HD by targeting the mutated gene responsible for the disease.
- Neuroprotective Agents: Researchers are studying various compounds that may protect brain cells from degeneration, potentially slowing the progression of HD.
Huntington’s Disease Support and Resources
Finding support and resources is essential for individuals and families affected by Huntington’s Disease. Here are some valuable options to consider:
National and Local Organizations
Several organizations provide resources, advocacy, and support for those impacted by HD:
- Huntington’s Disease Society of America (HDSA): HDSA offers a wealth of information, including educational materials, support groups, and advocacy initiatives.
- Huntington’s Disease Association (HDA): This organization focuses on raising awareness and providing support for individuals and families affected by HD.
- Huntington’s Disease Youth Organization (HDYO): HDYO is dedicated to supporting young people impacted by HD, offering resources tailored to their unique needs.
Online Resources and Communities
The internet can be a valuable tool for finding information and connecting with others:
- Online Forums: Websites like Reddit have communities where individuals can share experiences, ask questions, and find support.
- Social Media Groups: Platforms like Facebook host groups dedicated to Huntington’s Disease, providing a space for sharing stories and resources.
Educational Materials
Staying informed is crucial for managing Huntington’s Disease. Consider accessing:
- Books and Articles: Numerous publications provide insights into living with HD, including personal stories and expert advice.
- Webinars and Workshops: Many organizations offer online events that cover various aspects of HD, from treatment options to coping strategies.
By utilizing these treatment options and support resources, individuals and families affected by Huntington’s Disease can navigate the challenges of this condition with greater resilience and hope. 🌟

Frequently Asked Questions about Huntington’s Disease (HD)
What is Huntington’s Disease (HD)?
Huntington’s Disease (HD) is a genetic disorder that causes the progressive breakdown of nerve cells in the brain. It affects movement, cognition, and behavior, leading to a range of symptoms that can significantly impact daily life.
What are the common symptoms of Huntington’s Disease (HD)?
Symptoms of Huntington’s Disease (HD) can vary widely but often include:
- Chorea (involuntary movements)
- Difficulty with coordination and balance
- Cognitive decline and memory issues
- Emotional disturbances, such as depression and anxiety
Is there a cure for Huntington’s Disease (HD)? 🤔
Currently, there is no cure for Huntington’s Disease (HD). However, treatments are available to help manage symptoms and improve quality of life. Ongoing research is exploring potential therapies that may slow the progression of the disease.
What is chorea in the context of Huntington’s Disease (HD)?
Chorea refers to the involuntary, irregular movements that are characteristic of Huntington’s Disease (HD). These movements can affect various parts of the body and may interfere with daily activities.
How is Huntington’s Disease (HD) diagnosed?
Diagnosis of Huntington’s Disease (HD) typically involves a combination of:
- Medical history and physical examination
- Genetic testing to confirm the presence of the mutated gene
- Neurological assessments to evaluate symptoms
Are there support organizations for Huntington’s Disease (HD)?
Yes, there are several organizations dedicated to supporting individuals and families affected by Huntington’s Disease (HD). Notable organizations include:
- Huntington’s Disease Society of America (HDSA)
- Huntington’s Disease Association (HDA)
- Huntington’s Disease Youth Organization (HDYO)
What lifestyle changes can help manage Huntington’s Disease (HD) symptoms?
While there is no cure for Huntington’s Disease (HD), certain lifestyle changes may help manage symptoms. These can include:
- Regular physical activity
- A balanced diet rich in nutrients
- Engaging in cognitive exercises
- Seeking support from mental health professionals
What research is being conducted on Huntington’s Disease (HD)?
Research on Huntington’s Disease (HD) is ongoing, focusing on various aspects such as:
- New treatment options and clinical trials
- Understanding the genetic mechanisms of the disease
- Exploring lifestyle interventions that may improve symptoms
How can I connect with others affected by Huntington’s Disease (HD)?
Connecting with others can provide valuable support. Consider joining support groups or online forums where individuals share their experiences and coping strategies related to Huntington’s Disease (HD).