What Is Grave’s Disease?
Grave’s Disease is an autoimmune disorder that primarily affects the thyroid gland, leading to an overproduction of thyroid hormones, a condition known as hyperthyroidism. This disease is named after the Irish physician Robert Graves, who first described it in the 19th century. The thyroid gland, located at the base of the neck, plays a crucial role in regulating metabolism, energy levels, and overall bodily functions by producing hormones such as thyroxine (T4) and triiodothyronine (T3).
In Grave’s Disease, the body’s immune system mistakenly attacks the thyroid gland, causing it to enlarge and produce excessive amounts of hormones. This can lead to a variety of health issues, making early diagnosis and treatment essential. Understanding the underlying mechanisms of this condition can help patients manage their symptoms effectively.
Causes of Grave’s Disease
The exact cause of Grave’s Disease remains unclear, but several factors may contribute to its development:
- Genetics: A family history of autoimmune diseases can increase the risk of developing Grave’s Disease.
- Environmental Triggers: Factors such as stress, infections, or exposure to certain chemicals may trigger the onset of the disease.
- Hormonal Changes: Hormonal fluctuations, particularly in women during pregnancy or menopause, can also play a role.
Research indicates that the presence of specific antibodies, such as thyroid-stimulating immunoglobulins (TSI), can lead to the overstimulation of the thyroid gland, resulting in hyperthyroidism. Understanding these factors can help in managing and treating the disease effectively.
Grave’s Disease Symptoms
The symptoms of Grave’s Disease can vary widely among individuals, but they often stem from the effects of excess thyroid hormones on the body. Recognizing these symptoms early can lead to timely intervention and better management of the condition.
Common Symptoms
Some of the most common symptoms associated with Grave’s Disease include:
- Weight Loss: Despite an increased appetite, individuals may experience unexplained weight loss due to a heightened metabolic rate.
- Increased Heart Rate: Palpitations or a rapid heartbeat (tachycardia) are common as the body works harder to manage excess hormones.
- Heat Intolerance: Many individuals report feeling excessively warm or sweating more than usual.
- Nervousness and Anxiety: Increased irritability, anxiety, and mood swings can occur due to hormonal imbalances.
- Fatigue: Despite feeling energetic, many patients experience fatigue and muscle weakness.
- Changes in Menstrual Patterns: Women may notice irregularities in their menstrual cycles.
Eye-Related Symptoms
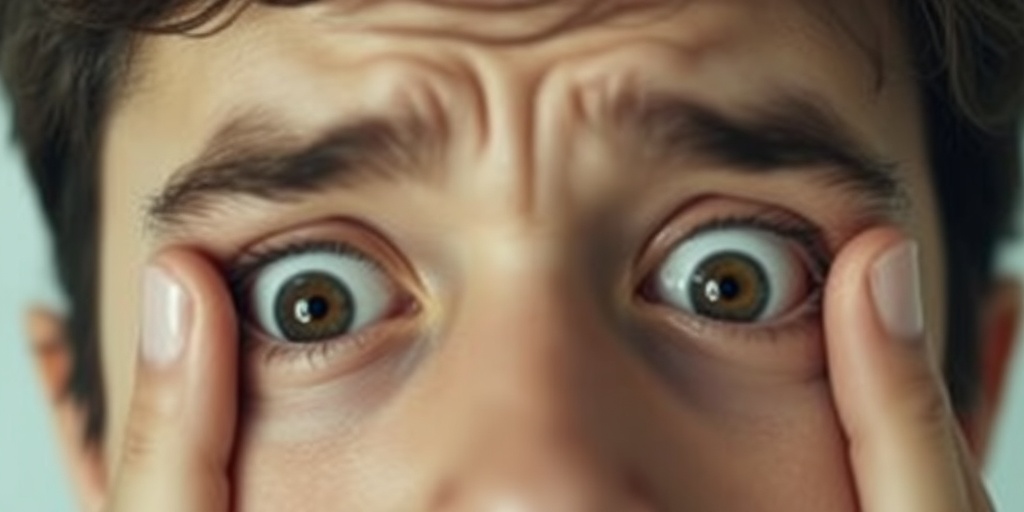
One of the hallmark features of Grave’s Disease is its potential impact on the eyes, known as Graves’ ophthalmopathy. Symptoms may include:
- Bulging Eyes: Protrusion of the eyes (exophthalmos) is a common symptom, leading to a distinctive appearance.
- Dryness and Irritation: Patients may experience dryness, redness, or a gritty sensation in the eyes.
- Vision Changes: Blurred or double vision can occur, and in severe cases, vision loss may happen.
When to Seek Medical Attention
If you experience any combination of these symptoms, it is crucial to consult a healthcare professional for a thorough evaluation. Early diagnosis and treatment can significantly improve quality of life and prevent complications associated with Grave’s Disease.
For those seeking more information on managing Grave’s Disease, Yesil Health AI (yesilhealth.com) offers evidence-based health answers and resources that can help you navigate your journey with this condition.
In conclusion, understanding Grave’s Disease and its symptoms is vital for effective management. By recognizing the signs and seeking timely medical advice, individuals can take proactive steps toward better health and well-being. 🌟
Grave’s Disease Causes
Grave’s Disease is an autoimmune disorder that primarily affects the thyroid gland, leading to hyperthyroidism. Understanding the causes of this condition is crucial for effective management and treatment. Let’s delve into the factors that contribute to the development of Grave’s Disease.
Autoimmune Response
At the heart of Grave’s Disease is an autoimmune response. In this condition, the body’s immune system mistakenly attacks its own thyroid gland, producing antibodies that stimulate the gland to produce excess thyroid hormones. The primary antibody involved is known as thyroid-stimulating immunoglobulin (TSI). This overproduction of hormones can lead to a variety of symptoms, including weight loss, increased heart rate, and anxiety.
Genetic Predisposition
Genetics play a significant role in the likelihood of developing Grave’s Disease. If you have a family history of thyroid disorders or autoimmune diseases, your risk may be higher. Studies suggest that certain genes may predispose individuals to autoimmune conditions, including Grave’s Disease. This genetic link highlights the importance of understanding your family medical history.
Environmental Triggers
While genetics are important, environmental factors can also trigger the onset of Grave’s Disease. Some potential triggers include:
- Stress: High levels of stress can impact the immune system, potentially triggering autoimmune responses.
- Infections: Certain viral infections, such as Epstein-Barr virus (EBV), have been linked to the development of autoimmune diseases, including Grave’s Disease.
- Smoking: Tobacco use has been associated with an increased risk of developing Grave’s Disease, particularly in women.
- Radiation Exposure: Exposure to radiation, especially in the neck area, can increase the risk of thyroid disorders.
Hormonal Changes
Hormonal fluctuations, particularly in women, can also play a role in the onset of Grave’s Disease. Many women experience the onset of symptoms during periods of hormonal change, such as pregnancy or menopause. This suggests that estrogen may influence the immune response, making women more susceptible to autoimmune conditions.
Grave’s Disease Risk Factors
Identifying the risk factors associated with Grave’s Disease can help in early detection and management. Here are some key risk factors to consider:
Age and Gender
Grave’s Disease is more common in women than in men, with a ratio of approximately 7:1. Additionally, it typically occurs in individuals between the ages of 30 and 50. Understanding this demographic trend can aid in recognizing symptoms early, especially in women within this age range.
Family History
A family history of thyroid disease or other autoimmune disorders significantly increases the risk of developing Grave’s Disease. If you have relatives with conditions such as Hashimoto’s thyroiditis or type 1 diabetes, it may be beneficial to monitor your thyroid health closely.
Other Autoimmune Disorders
Individuals with one autoimmune disorder are at a higher risk of developing another. Conditions such as rheumatoid arthritis, lupus, and pernicious anemia can coexist with Grave’s Disease. If you have been diagnosed with any autoimmune condition, it’s essential to discuss your thyroid health with your healthcare provider.
Smoking
As mentioned earlier, smoking is a significant risk factor for Grave’s Disease. The harmful substances in tobacco can affect the immune system and thyroid function. Quitting smoking can not only reduce the risk of developing this condition but also improve overall health.
Excessive Iodine Intake
While iodine is essential for thyroid function, excessive intake can lead to thyroid dysfunction. Individuals who consume high amounts of iodine, whether through diet or supplements, may be at an increased risk for developing Grave’s Disease. It’s important to maintain a balanced diet and consult with a healthcare provider before taking iodine supplements.
In summary, understanding the causes and risk factors of Grave’s Disease is vital for early detection and effective management. By being aware of these elements, individuals can take proactive steps towards maintaining their thyroid health. 🌟

Grave’s Disease Diagnosis
Diagnosing Grave’s Disease can be a complex process, as its symptoms often mimic those of other health conditions. This autoimmune disorder primarily affects the thyroid gland, leading to an overproduction of thyroid hormones. Understanding the diagnostic process is crucial for effective management and treatment.
Recognizing Symptoms
The first step in diagnosing Grave’s Disease is recognizing its symptoms. Common signs include:
- Hyperthyroidism: Increased heart rate, weight loss, and anxiety.
- Eye Problems: Bulging eyes (exophthalmos), irritation, and vision changes.
- Skin Changes: Warm, moist skin and thinning hair.
- Goiter: An enlarged thyroid gland, which may cause swelling at the base of the neck.
If you experience these symptoms, it’s essential to consult a healthcare professional for further evaluation. Early diagnosis can significantly improve treatment outcomes.
Blood Tests
Once symptoms are noted, doctors typically order blood tests to confirm the diagnosis. Key tests include:
- Thyroid Function Tests: These measure levels of thyroid hormones (T3 and T4) and Thyroid-Stimulating Hormone (TSH). In Grave’s Disease, T3 and T4 levels are usually elevated, while TSH levels are low.
- Thyroid Antibodies: The presence of specific antibodies, such as Thyroid-Stimulating Immunoglobulin (TSI), can indicate Grave’s Disease.
Imaging Tests
In some cases, imaging tests may be necessary to assess the thyroid gland’s structure and function. Common imaging techniques include:
- Radioactive Iodine Uptake Test: This test measures how much iodine the thyroid absorbs, helping to determine if the gland is overactive.
- Ultrasound: An ultrasound can visualize the thyroid gland and identify any abnormalities.
These diagnostic tools, combined with a thorough medical history and physical examination, help healthcare providers confirm a diagnosis of Grave’s Disease.
Grave’s Disease Treatment Options
Once diagnosed, the next step is to explore treatment options for Grave’s Disease. The goal of treatment is to manage symptoms, reduce thyroid hormone production, and prevent complications. Here are the primary treatment modalities:
Medications
Medications are often the first line of treatment for managing Grave’s Disease. Common options include:
- Antithyroid Medications: Drugs like methimazole and propylthiouracil help reduce the production of thyroid hormones.
- Beta-Blockers: These medications can alleviate symptoms such as rapid heart rate and anxiety, providing relief while other treatments take effect.
Radioactive Iodine Therapy
Radioactive iodine therapy is a widely used treatment for Grave’s Disease. This approach involves:
- Targeting the Thyroid: Patients ingest radioactive iodine, which selectively destroys overactive thyroid cells.
- Long-Term Management: This treatment often leads to hypothyroidism, requiring lifelong thyroid hormone replacement therapy.
Surgery
In certain cases, surgical intervention may be necessary. Options include:
- Thyroidectomy: Partial or total removal of the thyroid gland may be recommended, especially for patients with large goiters or those who cannot tolerate other treatments.
Lifestyle and Dietary Changes
In addition to medical treatments, lifestyle and dietary changes can play a significant role in managing Grave’s Disease. Consider the following:
- Balanced Diet: Focus on a diet rich in fruits, vegetables, whole grains, and lean proteins to support overall health.
- Avoiding Stimulants: Reducing caffeine and other stimulants can help manage symptoms like anxiety and insomnia.
- Regular Exercise: Engaging in regular physical activity can improve mood and overall well-being.
Managing Grave’s Disease requires a comprehensive approach that includes medical treatment, lifestyle adjustments, and regular monitoring. By working closely with healthcare professionals, individuals can effectively manage their condition and lead fulfilling lives. 🌟

Grave’s Disease Complications
Grave’s Disease is an autoimmune disorder that primarily affects the thyroid gland, leading to an overproduction of thyroid hormones. While many individuals manage their symptoms effectively, it’s crucial to be aware of the potential complications that can arise from this condition. Understanding these complications can help in early detection and treatment, ultimately improving quality of life.
1. Thyroid Storm
One of the most severe complications of Grave’s Disease is a thyroid storm, a life-threatening condition characterized by an extreme increase in thyroid hormone levels. Symptoms may include:
- High fever
- Rapid heart rate
- Severe agitation or confusion
- Diarrhea or vomiting
If not treated promptly, a thyroid storm can lead to heart failure, coma, or even death. It’s essential for individuals with Grave’s Disease to recognize these symptoms and seek immediate medical attention.
2. Eye Problems (Graves’ Ophthalmopathy)
Many patients with Grave’s Disease experience eye-related complications, known as Graves’ ophthalmopathy. This condition can cause:
- Bulging eyes (exophthalmos)
- Dryness or irritation
- Double vision
- Vision loss in severe cases
These symptoms occur due to inflammation and swelling of the eye muscles and surrounding tissues. Regular eye examinations and consultations with an ophthalmologist are vital for managing these complications.
3. Heart Issues
Grave’s Disease can lead to various cardiovascular problems, including:
- Increased heart rate (tachycardia)
- High blood pressure
- Heart palpitations
Over time, these issues can increase the risk of heart disease and other serious conditions. Monitoring heart health is crucial for individuals diagnosed with Grave’s Disease.
4. Bone Health
Another significant complication is the impact on bone density. Hyperthyroidism, the condition caused by Grave’s Disease, can lead to:
- Decreased bone density
- Increased risk of fractures
Patients should consider regular bone density screenings and discuss preventive measures with their healthcare provider.
5. Mental Health Challenges
Living with Grave’s Disease can also take a toll on mental health. Many individuals report experiencing:
- Anxiety
- Depression
- Difficulty concentrating
It’s essential to address these mental health concerns through therapy, support groups, or medication if necessary. A holistic approach to treatment can significantly improve overall well-being.
Living with Grave’s Disease
Managing Grave’s Disease requires a comprehensive approach that includes medical treatment, lifestyle adjustments, and emotional support. Here are some strategies to help individuals live well with this condition.
1. Medication Management
Most patients with Grave’s Disease will require medication to control their thyroid hormone levels. Common treatments include:
- Antithyroid medications (e.g., methimazole) to reduce hormone production
- Beta-blockers to manage symptoms like rapid heart rate
- Radioactive iodine therapy to destroy overactive thyroid cells
Regular follow-ups with a healthcare provider are essential to monitor hormone levels and adjust medications as needed.
2. Dietary Considerations
While there is no specific Grave’s Disease diet, certain dietary choices can support overall health. Consider incorporating:
- Fruits and vegetables rich in antioxidants
- Whole grains for sustained energy
- Lean proteins to support muscle health
Additionally, staying hydrated and limiting caffeine and sugar can help manage symptoms. Always consult with a healthcare provider or nutritionist before making significant dietary changes.
3. Stress Management
Stress can exacerbate symptoms of Grave’s Disease, making stress management techniques vital. Consider practices such as:
- Yoga and meditation for relaxation
- Regular exercise to boost mood and energy levels
- Mindfulness techniques to stay grounded
Finding a routine that works for you can significantly improve your quality of life.
4. Support Systems
Connecting with others who understand the challenges of living with Grave’s Disease can be incredibly beneficial. Consider:
- Joining support groups
- Engaging in online forums
- Seeking therapy or counseling
Sharing experiences and coping strategies can provide emotional relief and practical advice.
5. Regular Monitoring
Finally, regular monitoring of your condition is crucial. This includes:
- Routine blood tests to check thyroid hormone levels
- Regular check-ups with your healthcare provider
- Monitoring for any new symptoms or complications
Staying proactive about your health can help you manage Grave’s Disease effectively and maintain a fulfilling life. 🌟

Frequently Asked Questions about Grave’s Disease
What is Grave’s Disease?
Grave’s Disease is an autoimmune disorder that leads to the overproduction of thyroid hormones, a condition known as hyperthyroidism. It is characterized by symptoms such as weight loss, rapid heartbeat, and anxiety.
What causes Grave’s Disease?
The exact cause of Grave’s Disease is not fully understood, but it is believed to involve a combination of genetic and environmental factors. The immune system mistakenly attacks the thyroid gland, leading to excessive hormone production.
What are the common symptoms of Grave’s Disease?
- Increased heart rate
- Weight loss despite normal or increased appetite
- Increased sweating and sensitivity to heat
- Nervousness or anxiety
- Fatigue and muscle weakness
- Changes in menstrual patterns
- Bulging eyes (exophthalmos)
How is Grave’s Disease diagnosed?
Diagnosis of Grave’s Disease typically involves a combination of physical examinations, blood tests to measure thyroid hormone levels, and the presence of specific antibodies associated with the disease.
What are the treatment options for Grave’s Disease?
Treatment for Grave’s Disease may include:
- Antithyroid medications: These help reduce the production of thyroid hormones.
- Radioactive iodine therapy: This treatment destroys overactive thyroid cells.
- Surgery: In some cases, a total or partial thyroidectomy may be necessary.
Can diet affect Grave’s Disease?
While there is no specific Grave’s Disease diet, maintaining a balanced diet rich in nutrients can support overall health. Some individuals may find that avoiding certain foods helps manage symptoms, but it’s essential to consult with a healthcare provider before making significant dietary changes.
What is the ICD-10 code for Grave’s Disease?
The ICD-10 code for Grave’s Disease is E05.0, which is used for medical billing and documentation purposes.
Are there any complications associated with Grave’s Disease?
If left untreated, Grave’s Disease can lead to serious complications, including heart problems, osteoporosis, and a life-threatening condition known as thyroid storm. Regular monitoring and treatment are crucial to prevent these issues.
Can Grave’s Disease affect vision?
Yes, Grave’s Disease can lead to eye problems, particularly in cases of Graves’ ophthalmopathy, where the eyes may bulge and cause vision changes. If you experience any vision issues, it’s important to consult with an eye specialist.
Is there a connection between Grave’s Disease and other autoimmune disorders?
Yes, individuals with Grave’s Disease may have a higher risk of developing other autoimmune disorders, such as Hashimoto’s thyroiditis or rheumatoid arthritis. Regular check-ups can help monitor for these conditions.
Where can I find support for living with Grave’s Disease?
Support groups, both online and in-person, can provide valuable resources and community for those living with Grave’s Disease. Connecting with others who share similar experiences can be beneficial for emotional support and practical advice.




