“`html
What Is Granuloma Fungoides?
Granuloma Fungoides is a rare type of skin lymphoma, specifically classified as a form of cutaneous T-cell lymphoma (CTCL). This condition primarily affects the skin and is characterized by the presence of abnormal T-cells that can lead to various skin lesions. While it may sound alarming, understanding this condition is crucial for effective management and treatment.
Understanding the Basics
Granuloma Fungoides typically manifests in adults, although it can occur in individuals of any age. The name itself derives from the appearance of the lesions, which can resemble granulomas—small areas of inflammation in the skin. These lesions can vary in size, shape, and color, often leading to confusion with other skin conditions.
Causes and Risk Factors
The exact cause of Granuloma Fungoides remains unclear, but several factors may contribute to its development:
- Genetic predisposition: A family history of skin conditions or lymphomas may increase risk.
- Environmental factors: Exposure to certain chemicals or UV radiation could play a role.
- Immune system issues: Individuals with weakened immune systems may be more susceptible.
Diagnosis
Diagnosing Granuloma Fungoides involves a thorough examination by a dermatologist, who may perform a skin biopsy to confirm the presence of abnormal T-cells. Other tests, such as blood tests or imaging studies, may also be conducted to assess the extent of the disease.
Granuloma Fungoides Symptoms
The symptoms of Granuloma Fungoides can vary widely among individuals, making it essential to recognize the signs early for effective treatment. Here are some common symptoms to watch for:
Skin Lesions
The most prominent symptom of Granuloma Fungoides is the appearance of skin lesions. These can include:
- Patches: Flat, red, or brown areas that may be itchy.
- Plaques: Raised, thickened areas of skin that can be scaly.
- Tumors: Larger, nodular growths that may develop over time.
Itching and Discomfort
Many individuals with Granuloma Fungoides experience significant itching, which can lead to discomfort and affect quality of life. This itching may worsen at night or after exposure to heat.
Other Symptoms
In some cases, Granuloma Fungoides can lead to systemic symptoms, especially in advanced stages. These may include:
- Fatigue: A general feeling of tiredness that doesn’t improve with rest.
- Weight loss: Unexplained weight loss can occur in more severe cases.
- Swollen lymph nodes: Enlarged lymph nodes may indicate the spread of the disease.
When to Seek Medical Advice
If you notice any unusual skin changes or persistent itching, it’s important to consult a healthcare professional. Early diagnosis and treatment can significantly improve outcomes for individuals with Granuloma Fungoides.
For more information on skin conditions and health-related queries, consider visiting Yesil Health AI, a valuable resource for evidence-based health answers.
In conclusion, while Granuloma Fungoides can be a challenging condition, understanding its symptoms and seeking timely medical advice can lead to effective management. Stay informed and proactive about your health! 🌟
“`

“`html
Causes of Granuloma Fungoides
Granuloma Fungoides is a rare type of skin lymphoma that primarily affects the skin. Understanding the causes of this condition is crucial for early detection and effective management. While the exact cause of Granuloma Fungoides remains unclear, several factors have been identified that may contribute to its development.
Immune System Dysfunction
One of the leading theories regarding the cause of Granuloma Fungoides is related to immune system dysfunction. The immune system plays a vital role in protecting the body from infections and diseases. When it malfunctions, it may mistakenly attack healthy skin cells, leading to the formation of granulomas. This autoimmune response can result in the characteristic symptoms of Granuloma Fungoides.
Genetic Predisposition
Research suggests that genetics may also play a role in the development of Granuloma Fungoides. Individuals with a family history of skin conditions or lymphomas may be at a higher risk. Genetic mutations that affect the immune response could potentially increase susceptibility to this condition.
Environmental Factors
Environmental factors, such as exposure to certain chemicals or toxins, may contribute to the onset of Granuloma Fungoides. Prolonged exposure to pesticides, industrial chemicals, or even certain medications has been linked to skin disorders. While more research is needed, it’s essential to be aware of these potential triggers.
Infections
Some studies have indicated that infections, particularly viral infections, may be associated with the development of Granuloma Fungoides. For instance, the human immunodeficiency virus (HIV) and other viral agents can compromise the immune system, potentially leading to skin conditions like Granuloma Fungoides.
Risk Factors for Granuloma Fungoides
Identifying the risk factors associated with Granuloma Fungoides can help in early diagnosis and treatment. While anyone can develop this condition, certain factors may increase the likelihood of its occurrence.
Age and Gender
Granuloma Fungoides is more commonly diagnosed in adults, particularly those aged 40 and above. Additionally, studies suggest that men are more likely to develop this condition than women, indicating a potential gender predisposition.
Skin Type and Ethnicity
Individuals with lighter skin tones may be at a higher risk for developing Granuloma Fungoides. Furthermore, certain ethnic groups, such as Caucasians, have been observed to have a higher incidence of this skin lymphoma compared to others.
Chronic Skin Conditions
People with a history of chronic skin conditions, such as eczema or psoriasis, may have an increased risk of developing Granuloma Fungoides. The ongoing inflammation and immune response associated with these conditions could potentially trigger the onset of this lymphoma.
Weakened Immune System
A weakened immune system, whether due to a medical condition or immunosuppressive treatments, can elevate the risk of Granuloma Fungoides. Conditions like HIV/AIDS, or treatments for other cancers, can compromise the body’s ability to fight off diseases, making it more susceptible to skin lymphomas.
Family History
As mentioned earlier, a family history of skin disorders or lymphomas can increase the risk of developing Granuloma Fungoides. If you have relatives who have suffered from similar conditions, it’s essential to discuss this with your healthcare provider for appropriate monitoring.
Understanding the causes and risk factors associated with Granuloma Fungoides is vital for early detection and intervention. If you notice any unusual skin changes or symptoms, consult a healthcare professional for a thorough evaluation. 🩺
“`
“`html
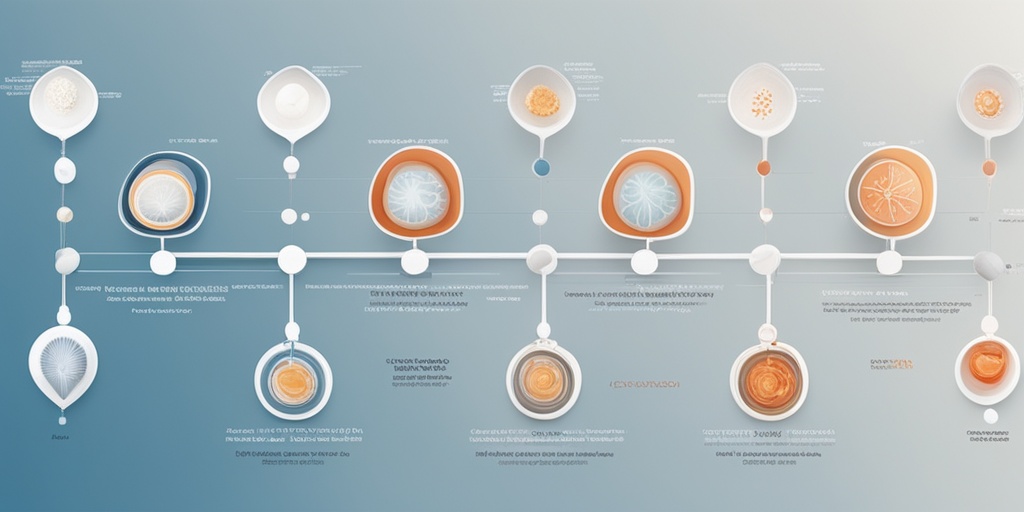
Diagnosis of Granuloma Fungoides
Diagnosing Granuloma Fungoides can be a complex process, as it often mimics other skin conditions. This rare type of cutaneous T-cell lymphoma primarily affects the skin and can present with various symptoms. Understanding the diagnostic steps is crucial for effective management.
Clinical Evaluation
The first step in diagnosing Granuloma Fungoides typically involves a thorough clinical evaluation by a dermatologist. During this examination, the doctor will:
- Review the patient’s medical history
- Examine the skin for characteristic lesions, which may appear as red, scaly patches or plaques
- Assess any associated symptoms, such as itching or discomfort
Skin Biopsy
A definitive diagnosis often requires a skin biopsy. This procedure involves removing a small sample of affected skin for laboratory analysis. The biopsy helps to:
- Identify the presence of atypical T-cells, which are indicative of Granuloma Fungoides
- Rule out other skin conditions, such as granuloma annulare or psoriasis
Histopathological examination of the biopsy sample is essential for confirming the diagnosis.
Imaging Studies
In some cases, imaging studies may be necessary to assess the extent of the disease. These can include:
- X-rays
- CT scans
- MRIs
These imaging techniques help determine if the disease has spread beyond the skin, which is crucial for staging and treatment planning.
Blood Tests
Blood tests may also be performed to evaluate overall health and check for any abnormalities that could indicate systemic involvement. While not specific for Granuloma Fungoides, these tests can provide valuable information about the patient’s condition.
Treatment Options for Granuloma Fungoides
Once diagnosed, the treatment of Granuloma Fungoides will depend on the stage of the disease, the extent of skin involvement, and the patient’s overall health. Here are some common treatment options:
Topical Treatments
For early-stage Granuloma Fungoides, topical therapies are often the first line of treatment. These may include:
- Corticosteroids: These anti-inflammatory medications can help reduce redness and itching.
- Topical chemotherapy: Agents like mechlorethamine can be applied directly to the skin to target cancerous cells.
- Retinoids: These vitamin A derivatives can help normalize skin cell growth.
Phototherapy
Phototherapy, or light therapy, is another effective treatment for Granuloma Fungoides. This involves exposing the skin to ultraviolet (UV) light under medical supervision. Types of phototherapy include:
- PUVA therapy: Combines a medication called psoralen with UVA light.
- UVB therapy: Uses UVB light alone to treat affected areas.
Phototherapy can help reduce skin lesions and improve symptoms.
Systemic Treatments
For more advanced stages of Granuloma Fungoides, systemic treatments may be necessary. These can include:
- Chemotherapy: Medications that target rapidly dividing cancer cells.
- Targeted therapies: Newer treatments that specifically target cancerous cells while sparing healthy ones.
- Immunotherapy: Treatments that help the immune system recognize and attack cancer cells.
Radiation Therapy
In some cases, radiation therapy may be recommended, especially for localized lesions. This treatment uses high-energy rays to kill cancer cells and shrink tumors.
Clinical Trials
Patients may also consider participating in clinical trials, which can provide access to cutting-edge therapies and contribute to advancing research in Granuloma Fungoides.
In conclusion, early diagnosis and a tailored treatment approach are essential for managing Granuloma Fungoides effectively. If you suspect you have this condition, consult a healthcare professional for a comprehensive evaluation and personalized treatment plan. 🌟
“`

“`html
Living with Granuloma Fungoides
Granuloma Fungoides is a rare form of cutaneous T-cell lymphoma that primarily affects the skin. Living with this condition can be challenging, but understanding it better can help patients manage their symptoms and improve their quality of life. 🌼
Understanding Granuloma Fungoides
Granuloma Fungoides typically presents as patches or plaques on the skin that may resemble eczema or psoriasis. These lesions can be itchy and may change over time. It’s important to note that while Granuloma Fungoides is a type of lymphoma, it is generally considered to be a slow-growing cancer, which means that many patients can live for years with the condition.
Symptoms to Watch For
Common symptoms of Granuloma Fungoides include:
- Red or brown patches: These may appear on various parts of the body, often starting on the trunk or limbs.
- Itching: Many patients experience significant itching, which can be distressing.
- Thickened skin: Over time, the affected areas may become thickened or scaly.
- Lesion progression: Lesions can evolve into more serious forms, including tumors.
Managing Symptoms
While there is no cure for Granuloma Fungoides, several treatment options can help manage symptoms and improve skin appearance:
- Topical treatments: Corticosteroids and other topical medications can reduce inflammation and itching.
- Phototherapy: Exposure to ultraviolet light can help clear skin lesions.
- Systemic therapies: In more advanced cases, medications that affect the entire body may be necessary.
It’s essential for patients to work closely with their healthcare providers to develop a personalized treatment plan that addresses their specific symptoms and concerns. Regular follow-ups can help monitor the condition and adjust treatments as needed.
Prognosis and Outlook
The prognosis for individuals with Granuloma Fungoides varies widely based on several factors, including the stage of the disease at diagnosis and the patient’s overall health. Understanding the outlook can provide hope and direction for those affected. 🌈
Factors Influencing Prognosis
Several key factors can influence the prognosis of Granuloma Fungoides:
- Stage of the disease: Early-stage Granuloma Fungoides typically has a better prognosis than advanced stages.
- Response to treatment: Patients who respond well to initial treatments often have a more favorable outlook.
- Overall health: A patient’s general health and any comorbid conditions can impact their ability to tolerate treatments and recover.
Survival Rates
Survival rates for Granuloma Fungoides can be encouraging, especially for those diagnosed at an early stage. According to various studies, the 5-year survival rate for early-stage patients can be as high as 90%. However, as the disease progresses, the outlook may change. It’s crucial for patients to have open discussions with their healthcare providers about their specific situation and what they can expect moving forward.
Living with Uncertainty
Living with a chronic condition like Granuloma Fungoides can bring about feelings of uncertainty and anxiety. It’s important for patients to seek support from healthcare professionals, support groups, and loved ones. Engaging in self-care practices, such as stress management techniques and maintaining a healthy lifestyle, can also contribute positively to overall well-being.
In conclusion, while Granuloma Fungoides presents unique challenges, understanding the condition and its management can empower patients to lead fulfilling lives. With appropriate treatment and support, many individuals can navigate their journey with resilience and hope. 🌟
“`

“`html
Frequently Asked Questions about Granuloma Fungoides
What is Granuloma Fungoides?
Granuloma Fungoides is a rare type of skin lymphoma that primarily affects the skin. It is characterized by the presence of patches, plaques, or tumors that can resemble other skin conditions. This condition is a form of cutaneous T-cell lymphoma (CTCL) and is often associated with a chronic course.
What are the symptoms of Granuloma Fungoides?
- Skin lesions: These can appear as red, scaly patches or plaques.
- Itching: Many patients experience significant itching in affected areas.
- Skin thickening: Over time, lesions may become thicker and more pronounced.
How is Granuloma Fungoides diagnosed?
Diagnosis typically involves a combination of physical examination, skin biopsy, and sometimes additional tests such as blood tests or imaging studies to assess the extent of the disease.
Can Granuloma Fungoides be treated?
Yes, treatment options for Granuloma Fungoides vary depending on the stage of the disease and may include:
- Topical therapies: Corticosteroids or other topical agents.
- Phototherapy: Light therapy can be effective for skin lesions.
- Systemic treatments: In more advanced cases, systemic therapies such as chemotherapy or biologic agents may be necessary.
Is Granuloma Fungoides related to other conditions?
While Granuloma Fungoides is a distinct condition, it can sometimes be confused with other skin disorders, such as granuloma annulare. However, granuloma annulare is not cancerous and is generally considered a benign skin condition.
Can cancer cause granulomas?
Yes, certain types of cancer, including lymphomas, can lead to the formation of granulomas. However, Granuloma Fungoides itself is a type of lymphoma that manifests primarily in the skin.
Is granuloma annulare cancer?
No, granuloma annulare is not considered cancer. It is a benign skin condition that may appear similar to Granuloma Fungoides but does not have the same implications for health.
What is the prognosis for someone with Granuloma Fungoides?
The prognosis for Granuloma Fungoides varies widely depending on the stage at diagnosis and the response to treatment. Many patients can manage their symptoms effectively and maintain a good quality of life.
Where can I find more information about Granuloma Fungoides?
For more detailed information, consider consulting healthcare professionals or reputable medical websites that specialize in dermatology and oncology.
“`




