What Is Folliculitis?
Folliculitis is a common skin condition characterized by the inflammation of hair follicles. It can occur anywhere on the body where hair grows, including the scalp, face, legs, and even the buttocks. This condition can be caused by various factors, including bacterial or fungal infections, irritation from shaving, or even hot tub exposure. Understanding what folliculitis is and its underlying causes is essential for effective treatment and prevention.
Types of Folliculitis
Folliculitis can be classified into several types, each with distinct causes:
- Bacterial Folliculitis: This is the most common form, often caused by Staphylococcus aureus bacteria. It typically presents as red, pus-filled bumps.
- Fungal Folliculitis: Often linked to Malassezia yeast, this type can cause itchy, inflamed follicles, particularly on the scalp and face.
- Hot Tub Folliculitis: This occurs after exposure to contaminated water, leading to a rash that can appear within a few days.
- Folliculitis Decalvans: A more severe form that can lead to hair loss and scarring, often requiring specialized treatment.
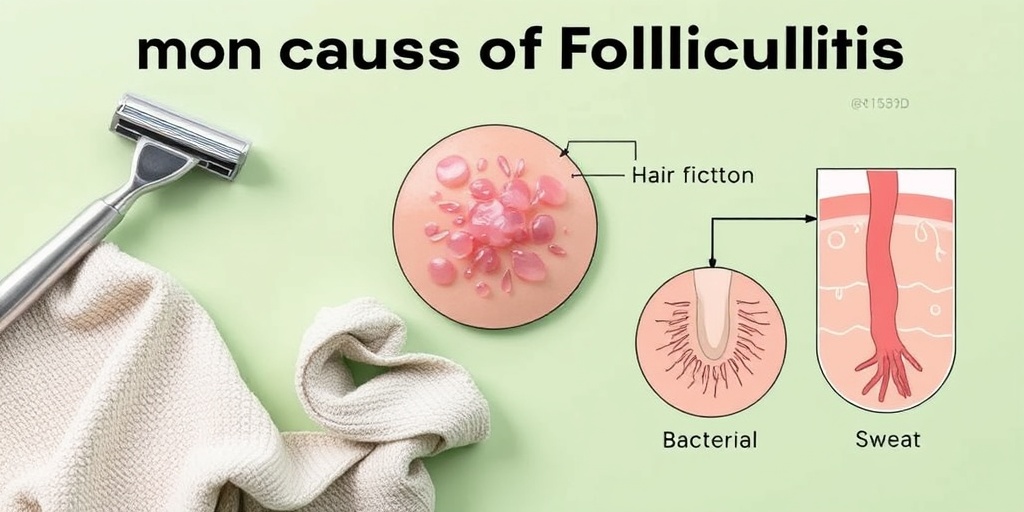
Causes of Folliculitis
Understanding the causes of folliculitis is crucial for prevention. Some common triggers include:
- Shaving or waxing, which can irritate hair follicles.
- Wearing tight clothing that traps sweat and bacteria.
- Hot tubs or swimming pools that are not properly sanitized.
- Skin conditions like dermatitis that can compromise the skin barrier.
Folliculitis Symptoms
The symptoms of folliculitis can vary depending on the type and severity of the condition. However, some common signs to look out for include:
- Red Bumps: Small, red, inflamed bumps around hair follicles are often the first sign.
- Pus-filled Blisters: These can develop and may ooze or crust over.
- Itching or Burning: Many individuals experience discomfort, which can be bothersome.
- Swelling: The affected area may become swollen and tender to the touch.
When to Seek Medical Attention
While folliculitis is often mild and self-limiting, there are instances when it’s important to consult a healthcare professional:
- If symptoms persist or worsen despite home treatment.
- If you develop a fever or feel unwell, indicating a possible systemic infection.
- If you notice signs of scarring or hair loss, particularly with folliculitis decalvans.
For those seeking more information on folliculitis treatment options, including topical creams and shampoos, resources like Yesil Health AI can provide evidence-based answers tailored to your needs.
Conclusion
Folliculitis is a manageable condition with a variety of treatment options available. By understanding its symptoms and causes, you can take proactive steps to prevent flare-ups and seek appropriate care when necessary. Remember, maintaining good hygiene and being mindful of skin irritants can go a long way in keeping folliculitis at bay. 🌟

Types of Folliculitis
Folliculitis is a common skin condition characterized by the inflammation of hair follicles. It can occur anywhere on the body where hair grows, leading to various types based on the underlying cause. Understanding the different types of folliculitis can help in identifying the right folliculitis treatment and managing symptoms effectively.
Bacterial Folliculitis
Bacterial folliculitis is the most prevalent form, often caused by Staphylococcus aureus, a type of bacteria that normally resides on the skin. This type typically presents as small, red bumps or pus-filled blisters around hair follicles. It can occur after shaving or wearing tight clothing, which irritates the skin.
Fungal Folliculitis
Fungal folliculitis, particularly Malassezia folliculitis, is caused by an overgrowth of yeast that naturally lives on the skin. This type is more common in individuals with oily skin or those who sweat excessively. Symptoms often include itchy, red bumps that may resemble acne, primarily on the scalp, chest, and back.
Hot Tub Folliculitis
As the name suggests, hot tub folliculitis occurs after exposure to contaminated water, often in hot tubs or pools. The bacteria Pseudomonas aeruginosa can thrive in warm, moist environments, leading to an outbreak of folliculitis. Symptoms typically appear within a few days of exposure and may include itchy, red bumps that can develop into pus-filled blisters.
Folliculitis Decalvans
This is a more severe form of folliculitis that can lead to permanent hair loss. Folliculitis decalvans is characterized by painful, inflamed areas on the scalp, often accompanied by crusting and scarring. The exact cause is not well understood, but it may be related to an autoimmune response or chronic bacterial infection.
Pityrosporum Folliculitis
Pityrosporum folliculitis is another type of fungal folliculitis caused by the same yeast responsible for dandruff. It often manifests as itchy, red bumps on the back, shoulders, and chest. This condition is more common in individuals with oily skin and can be exacerbated by hot, humid weather.
Causes of Folliculitis
Understanding the causes of folliculitis is crucial for effective prevention and treatment. Various factors can contribute to the development of this condition, ranging from hygiene practices to underlying health issues.
Infections
Both bacterial and fungal infections are primary causes of folliculitis. Bacterial folliculitis is often linked to skin injuries, such as cuts or abrasions, which allow bacteria to enter the hair follicles. On the other hand, fungal folliculitis is typically associated with an overgrowth of yeast, particularly in warm and humid environments.
Skin Irritation
Skin irritation from shaving, waxing, or wearing tight clothing can lead to folliculitis. These activities can damage hair follicles, making them more susceptible to infection. Additionally, using harsh soaps or skincare products can disrupt the skin’s natural barrier, increasing the risk of inflammation.
Hot and Humid Conditions
Hot and humid weather can create an ideal environment for the growth of bacteria and fungi. Individuals who sweat excessively or spend time in hot tubs or pools are at a higher risk of developing folliculitis. This is particularly true if the water is not properly sanitized.
Underlying Health Conditions
Certain health conditions can predispose individuals to folliculitis. For instance, those with diabetes or compromised immune systems may be more susceptible to infections. Additionally, conditions like acne or dermatitis can exacerbate the risk of developing folliculitis.
Medications
Some medications, particularly those that suppress the immune system, can increase the likelihood of developing folliculitis. Corticosteroids and antibiotics can alter the skin’s natural flora, making it easier for infections to take hold.
In conclusion, recognizing the types and causes of folliculitis is essential for effective management. If you suspect you have folliculitis, consult a healthcare professional for an accurate diagnosis and appropriate folliculitis treatment. 🌟
Risk Factors for Folliculitis
Folliculitis is a common skin condition that can affect anyone, but certain factors can increase your risk of developing this irritating rash. Understanding these risk factors can help you take preventive measures and seek timely treatment. Here are some key factors to consider:
1. Skin Type and Conditions
Individuals with oily skin or those who suffer from conditions like dermatitis are more prone to folliculitis. The excess oil can clog hair follicles, creating an environment conducive to bacterial or fungal growth.
2. Hot and Humid Environments
Living in hot and humid climates can increase your risk of developing folliculitis. Sweat and moisture can irritate the skin and lead to inflammation of the hair follicles. This is particularly common in cases of hot tub folliculitis, where bacteria thrive in warm, wet conditions.
3. Shaving and Hair Removal
Shaving or waxing can irritate the skin and damage hair follicles, making them more susceptible to infection. If you frequently shave areas prone to folliculitis, such as the face or legs, consider using a folliculitis cream or specialized folliculitis shampoo to help prevent outbreaks.
4. Weakened Immune System
Individuals with compromised immune systems, such as those with diabetes or undergoing chemotherapy, are at a higher risk for developing folliculitis. A weakened immune response can make it difficult for the body to fight off infections, including those that cause folliculitis.
5. Close Contact with Infected Individuals
Folliculitis can be contagious, especially when caused by bacteria. Close contact with someone who has an active infection can increase your risk. This is particularly relevant in communal settings like gyms or swimming pools.
6. Use of Certain Medications
Some medications, particularly those that affect the immune system or hormonal balance, can increase the likelihood of developing folliculitis. If you are on medication and notice symptoms, consult your healthcare provider for advice.
7. Fungal Infections
Fungal folliculitis, often caused by Malassezia, can occur in individuals who are prone to fungal infections. This type of folliculitis is more common in people with oily skin or those who use heavy skin products.
Diagnosing Folliculitis
Diagnosing folliculitis typically involves a thorough examination by a healthcare professional. Here’s what you can expect during the diagnostic process:
1. Medical History Review
Your doctor will begin by taking a detailed medical history. This includes asking about your symptoms, any recent skin irritations, and your personal and family medical history. Be prepared to discuss any medications you are taking and any underlying health conditions.
2. Physical Examination
A physical examination of the affected area is crucial. Your doctor will look for signs of inflammation, redness, and pus-filled bumps that are characteristic of folliculitis. They may also check for other skin conditions that could be causing similar symptoms.
3. Laboratory Tests
In some cases, your doctor may recommend laboratory tests to identify the specific cause of folliculitis. This could include:
- Culture Tests: A sample from the affected area may be taken to identify any bacteria or fungi present.
- Skin Biopsy: In rare cases, a small sample of skin may be removed for further analysis to rule out other conditions, such as folliculitis decalvans.
4. Identifying Triggers
Your healthcare provider may also ask about your lifestyle and habits to identify potential triggers for your folliculitis. This includes discussing your shaving techniques, skincare products, and exposure to hot tubs or communal showers.
5. Referral to a Specialist
If your case is particularly severe or resistant to treatment, your doctor may refer you to a dermatologist. A specialist can provide more targeted treatment options and help manage chronic cases of folliculitis.
Understanding the risk factors and diagnostic process for folliculitis can empower you to take control of your skin health. If you suspect you have folliculitis, don’t hesitate to seek medical advice for effective treatment options. 🌟

Folliculitis Treatment Options
Folliculitis is a common skin condition characterized by the inflammation of hair follicles, often resulting in red, itchy bumps that can resemble acne. Understanding the folliculitis treatment options available is essential for managing this condition effectively. Here, we’ll explore various treatments that can help alleviate symptoms and promote healing.
Topical Treatments
One of the first lines of defense against folliculitis is the use of topical treatments. These can include:
- Folliculitis cream: Over-the-counter creams containing ingredients like benzoyl peroxide or salicylic acid can help reduce inflammation and clear up the rash.
- Antibiotic ointments: For bacterial folliculitis, topical antibiotics such as mupirocin can be effective in treating the infection.
- Antifungal creams: If the folliculitis is caused by a fungal infection, such as malassezia folliculitis, antifungal creams can help eliminate the fungus.
Oral Medications
In more severe cases of folliculitis, oral medications may be necessary:
- Oral antibiotics: For extensive bacterial folliculitis, doctors may prescribe oral antibiotics to help clear the infection.
- Oral antifungals: If the condition is due to a fungal infection, oral antifungal medications may be recommended.
Specialized Shampoos
For those experiencing folliculitis on the scalp, specialized shampoos can be beneficial. Look for products that contain:
- Ketoconazole: An antifungal ingredient effective against fungal folliculitis.
- Salicylic acid: Helps to exfoliate the scalp and reduce inflammation.
Home Remedies
In addition to medical treatments, several home remedies can provide relief:
- Warm compresses: Applying a warm compress to the affected area can help soothe irritation and promote healing.
- Tea tree oil: Known for its antibacterial and antifungal properties, diluted tea tree oil can be applied to the affected areas.
- Aloe vera: This natural remedy can help reduce inflammation and soothe the skin.
When to See a Doctor
If your symptoms persist despite treatment or if you experience severe pain, swelling, or fever, it’s important to consult a healthcare professional. They can provide a proper diagnosis and recommend a tailored treatment plan.
Preventing Folliculitis
Preventing folliculitis is often easier than treating it. By adopting certain habits and practices, you can significantly reduce your risk of developing this condition. Here are some effective prevention strategies:
Maintain Good Hygiene
Keeping your skin clean is crucial in preventing folliculitis. Here are some tips:
- Shower regularly: Especially after sweating or exercising, to remove bacteria and sweat from the skin.
- Use antibacterial soap: This can help reduce the risk of bacterial infections.
Avoid Tight Clothing
Wearing tight clothing can irritate hair follicles and increase the risk of folliculitis. Opt for loose-fitting clothes, especially in hot and humid weather. This allows your skin to breathe and reduces friction.
Be Cautious with Hot Tubs
Hot tub folliculitis is a common issue caused by contaminated water. To prevent this:
- Ensure proper sanitation: Make sure hot tubs are well-maintained and sanitized.
- Limit exposure: Avoid prolonged exposure to hot tubs, especially if you have sensitive skin.
Choose the Right Hair Removal Methods
If you frequently shave or wax, consider the following:
- Use clean tools: Always use clean razors and waxing strips to minimize the risk of infection.
- Shave in the direction of hair growth: This can help reduce irritation and prevent ingrown hairs.
Moisturize Regularly
Keeping your skin hydrated can help maintain its barrier function and prevent irritation. Use non-comedogenic moisturizers that won’t clog your pores.
By implementing these preventive measures, you can significantly reduce your chances of developing folliculitis and maintain healthier skin. 🌟

Frequently Asked Questions about Folliculitis
What is Folliculitis?
Folliculitis is an inflammation of the hair follicles, often caused by bacterial or fungal infections. It can appear as small red bumps or pus-filled blisters on the skin, commonly affecting areas where hair grows, such as the scalp, face, and legs.
What are the symptoms of Folliculitis?
The symptoms of folliculitis include:
- Red or inflamed bumps
- Pus-filled blisters
- Itching or tenderness
- Crusting or scabbing
What causes Folliculitis?
Common causes of folliculitis include:
- Bacterial infections, particularly Staphylococcus aureus
- Fungal infections, such as Malassezia
- Ingrown hairs
- Hot tub exposure (known as hot tub folliculitis)
How can I treat Folliculitis?
Treatment options for folliculitis may include:
- Topical antibiotics or antifungal creams
- Oral antibiotics for severe cases
- Medicated shampoos for scalp folliculitis
- Warm compresses to soothe the affected area
Can Folliculitis occur on the scalp?
Yes, folliculitis on the scalp is common and can lead to itching and discomfort. Treatment may involve using specific folliculitis shampoo designed to target the infection.
Is Folliculitis contagious?
No, folliculitis itself is not contagious. However, the bacteria or fungi that cause it can spread through shared personal items or contaminated water.
What is the difference between bacterial and fungal Folliculitis?
Bacterial folliculitis is typically caused by bacteria like Staphylococcus aureus, while fungal folliculitis is often due to yeast infections, such as Malassezia folliculitis. The treatment may vary based on the underlying cause.
Can I prevent Folliculitis?
Preventive measures for folliculitis include:
- Avoiding tight clothing that can irritate the skin
- Keeping the skin clean and dry
- Avoiding hot tubs or pools that may be contaminated
When should I see a doctor?
If you experience persistent symptoms, severe pain, or if the folliculitis rash worsens, it is advisable to consult a healthcare professional for further evaluation and treatment.
Where can I find more information about Folliculitis?
For more insights and community discussions, you can explore platforms like Reddit or consult dermatology resources online. Always ensure to verify the information with a healthcare provider.