What Is Cervical Cancer?
Cervical cancer is a type of cancer that occurs in the cervix, which is the lower part of the uterus that connects to the vagina. This cancer typically develops slowly over time, often starting with precancerous changes in the cervical cells. Understanding what cervical cancer is, its causes, and how it can be prevented is crucial for women’s health.
Understanding the Causes of Cervical Cancer
The primary cause of cervical cancer is persistent infection with certain types of human papillomavirus (HPV), a sexually transmitted virus. While most HPV infections resolve on their own, some can lead to the development of cervical cancer over time. Other factors that may increase the risk of developing cervical cancer include:
- Smoking: Women who smoke are more likely to develop cervical cancer.
- Weakened Immune System: Conditions that weaken the immune system, such as HIV/AIDS, can increase the risk.
- Long-term Use of Birth Control Pills: Using oral contraceptives for five or more years may slightly increase the risk.
- Multiple Full-Term Pregnancies: Having many pregnancies can increase the risk of cervical cancer.
Regular cervical cancer screening is essential for early detection and prevention. The Pap test and HPV test are effective methods for identifying precancerous changes in cervical cells, allowing for timely intervention.
Cervical Cancer Symptoms
Recognizing the symptoms of cervical cancer is vital for early diagnosis and treatment. In the early stages, cervical cancer may not present any noticeable symptoms. However, as the disease progresses, women may experience various signs that should not be ignored.
Common Signs of Cervical Cancer
Some of the most common symptoms associated with cervical cancer include:
- Abnormal Vaginal Bleeding: This may include bleeding between periods, after sexual intercourse, or after menopause.
- Unusual Vaginal Discharge: A watery, bloody discharge that may have a foul odor can be a sign of cervical cancer.
- Pain During Intercourse: Experiencing pain during sexual activity can indicate underlying issues.
- Pelvic Pain: Persistent pain in the pelvic area that is not related to menstrual cycles should be evaluated.
When to Seek Medical Advice
If you experience any of these symptoms, it is crucial to consult a healthcare professional. Early detection through cervical cancer screening can significantly improve treatment outcomes. Regular screenings, such as Pap smears and HPV tests, are recommended for women starting at age 21, or within three years of becoming sexually active.
For more information on cervical cancer, its symptoms, and screening options, consider visiting Yesil Health AI, a valuable resource for evidence-based health answers.
In conclusion, understanding what cervical cancer is and being aware of its symptoms can empower women to take charge of their health. Regular screenings and awareness of risk factors are essential steps in preventing this disease. Remember, early detection saves lives! 🌸
Cervical Cancer Risk Factors
Cervical cancer is a significant health concern for women worldwide. Understanding the risk factors associated with this disease can empower individuals to take proactive steps towards prevention and early detection. Here are some of the primary risk factors linked to cervical cancer:
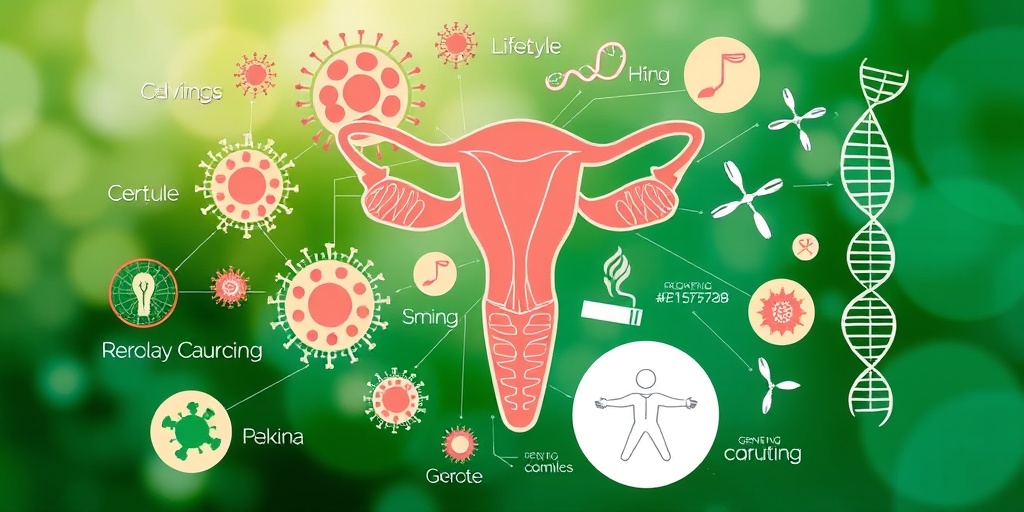
Human Papillomavirus (HPV) Infection
One of the most critical risk factors for cervical cancer is infection with the Human Papillomavirus (HPV). This virus is sexually transmitted and is responsible for the majority of cervical cancer cases. While most HPV infections resolve on their own, persistent infections with high-risk HPV types can lead to the development of cervical cancer over time.
Smoking
Smoking is another significant risk factor. Women who smoke are about twice as likely to develop cervical cancer compared to non-smokers. The harmful chemicals in tobacco can damage the DNA of cervical cells, making them more susceptible to cancerous changes.
Weakened Immune System
A weakened immune system, whether due to conditions like HIV/AIDS or the use of immunosuppressive medications, can increase the risk of cervical cancer. A healthy immune system plays a crucial role in fighting off HPV infections and other potential threats to cervical health.
Long-term Use of Birth Control Pills
Research suggests that women who use oral contraceptives for five years or more may have an increased risk of cervical cancer. While the benefits of birth control pills often outweigh the risks, it’s essential to discuss any concerns with a healthcare provider.
Multiple Full-term Pregnancies
Having multiple full-term pregnancies has been associated with an increased risk of cervical cancer. The reasons behind this correlation are not entirely understood, but hormonal changes and the physical stress of pregnancy may play a role.
Age
Cervical cancer is more commonly diagnosed in women over the age of 30. Regular cervical cancer screening is crucial for early detection, especially as women age.
Family History
A family history of cervical cancer or other related cancers can also increase an individual’s risk. Genetic factors may contribute to the likelihood of developing cervical cancer, making it essential for those with a family history to discuss screening options with their healthcare provider.
Cervical Cancer Causes
Understanding the causes of cervical cancer is vital for prevention and early intervention. While the exact cause of cervical cancer can vary, several key factors contribute to its development:
Human Papillomavirus (HPV)
As mentioned earlier, the primary cause of cervical cancer is infection with high-risk types of HPV. This virus can cause changes in the cervical cells, leading to precancerous lesions and, eventually, cancer if left untreated. Vaccination against HPV can significantly reduce the risk of developing cervical cancer.
Other Sexually Transmitted Infections (STIs)
In addition to HPV, other sexually transmitted infections, such as chlamydia and herpes, may increase the risk of cervical cancer. These infections can cause inflammation and cellular changes in the cervix, making it more susceptible to cancerous developments.
Long-term Use of Immunosuppressive Medications
Individuals who are on long-term immunosuppressive therapy, such as those who have undergone organ transplants, may have a higher risk of cervical cancer. These medications can weaken the immune response, allowing HPV and other infections to persist and potentially lead to cancer.
Environmental Factors
Exposure to certain environmental factors, such as prolonged use of birth control pills and smoking, can also contribute to the development of cervical cancer. These factors can interact with genetic predispositions, increasing the likelihood of cancerous changes in cervical cells.
Genetic Factors
Some women may have a genetic predisposition to cervical cancer, which can be inherited from family members. Genetic testing may be recommended for those with a strong family history of cervical or related cancers.
In conclusion, understanding the risk factors and causes of cervical cancer is essential for prevention and early detection. Regular screenings and vaccinations can significantly reduce the risk and improve outcomes for women at risk of this disease. Stay informed and proactive about your cervical health! 🌸
Cervical Cancer Diagnosis
Diagnosing cervical cancer is a crucial step in ensuring effective treatment and better outcomes for patients. Early detection can significantly improve survival rates, making it essential for women to understand the diagnostic process.
Understanding the Diagnostic Process
The diagnosis of cervical cancer typically begins with a thorough medical history and a physical examination. Healthcare providers will often perform a pelvic exam to check for any abnormalities. If there are concerns, further tests will be recommended.
Cervical Cancer Screening
Cervical cancer screening is vital for early detection. The two primary screening tests are:
- Pap Smear (Pap Test): This test involves collecting cells from the cervix to look for precancerous changes or cancerous cells.
- HPV Test: This test checks for the presence of human papillomavirus (HPV), a virus that can lead to cervical cancer.
Women should begin screening at age 21 and continue regularly based on their age and health history. The combination of these tests can help identify issues before they develop into cancer.
Follow-Up Tests
If initial screenings indicate potential problems, further diagnostic tests may be necessary, including:
- Colposcopy: A procedure that uses a special microscope to examine the cervix more closely.
- Biopsy: A small sample of cervical tissue is taken for laboratory analysis to confirm the presence of cancer cells.
These follow-up tests are essential for determining the presence and extent of cervical cancer.
Symptoms and Signs of Cervical Cancer
While many women may not experience symptoms in the early stages, it’s important to be aware of potential signs of cervical cancer, which can include:
- Unusual vaginal bleeding (between periods or after intercourse)
- Pain during intercourse
- Unexplained weight loss
- Pelvic pain
If you experience any of these symptoms, it’s crucial to consult a healthcare provider for further evaluation.
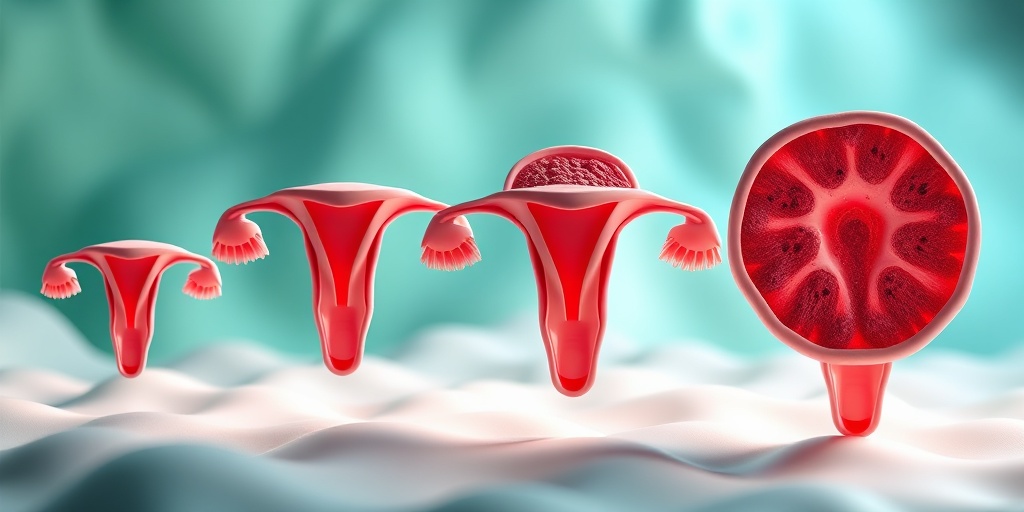
Cervical Cancer Stages
Understanding the stages of cervical cancer is essential for determining the most effective treatment options. The staging process helps to assess how far the cancer has spread in the body.
What Are the Stages of Cervical Cancer?
Cervical cancer is typically classified into four main stages:
- Stage 0: Also known as carcinoma in situ, this stage indicates that abnormal cells are present but have not invaded deeper tissues.
- Stage I: Cancer has invaded the cervix but is still confined to the uterus. This stage is further divided into IA and IB, depending on the depth of invasion.
- Stage II: The cancer has spread beyond the cervix and uterus but has not reached the pelvic wall or lower third of the vagina.
- Stage III: Cancer has spread to the lower part of the vagina or pelvic wall and may have caused kidney problems.
- Stage IV: This is the most advanced stage, where cancer has spread to other parts of the body, such as the bladder, rectum, or distant organs.
Importance of Staging
Staging is crucial as it guides treatment decisions. For instance, early-stage cervical cancer may be treated with surgery, while advanced stages may require a combination of chemotherapy, radiation, and surgery.
Regular Screening and Awareness
Regular cervical cancer screening is vital for early detection and can significantly impact the stage at which the cancer is diagnosed. Women should stay informed about their health and consult healthcare providers for personalized screening recommendations.
By understanding the diagnosis and staging of cervical cancer, women can take proactive steps toward their health and well-being. Remember, early detection saves lives! 💖
Cervical Cancer Treatment Options
Cervical cancer is a serious health concern that affects thousands of women each year. Understanding the treatment options available is crucial for those diagnosed with this condition. The treatment plan often depends on various factors, including the stage of cancer, the patient’s overall health, and personal preferences. Here, we explore the most common treatment options for cervical cancer.
Surgery
Surgery is often the first line of treatment for cervical cancer, especially in its early stages. The goal of surgery is to remove the cancerous tissue and, in some cases, surrounding healthy tissue. Common surgical procedures include:
- Conization: A procedure that removes a cone-shaped piece of tissue from the cervix, often used for early-stage cancer.
- Hysterectomy: The removal of the uterus and cervix. This can be a total hysterectomy (removing the entire uterus) or a radical hysterectomy (removing the uterus, cervix, and surrounding tissues).
- Pelvic Exenteration: In advanced cases, this procedure involves removing the uterus, cervix, vagina, and surrounding organs.
Radiation Therapy
Radiation therapy uses high-energy rays to kill cancer cells. It can be used alone or in combination with surgery and chemotherapy. There are two main types of radiation therapy:
- External Beam Radiation: This method directs radiation from outside the body to the tumor.
- Brachytherapy: This involves placing radioactive material inside or near the tumor, allowing for a more targeted approach.
Chemotherapy
Chemotherapy uses drugs to kill cancer cells or stop their growth. It is often used when cervical cancer has spread beyond the cervix or in conjunction with radiation therapy. Common chemotherapy drugs for cervical cancer include:
- Cisplatin
- Carboplatin
- Paclitaxel
Patients may experience side effects such as nausea, fatigue, and hair loss, but these can often be managed with supportive care.
Targeted Therapy and Immunotherapy
Recent advancements in cancer treatment have led to the development of targeted therapies and immunotherapy. These treatments focus on specific characteristics of cancer cells or enhance the body’s immune response against cancer. While still being researched, they show promise for certain patients with advanced cervical cancer.
Cervical Cancer Prevention
Preventing cervical cancer is possible through various strategies, primarily focusing on early detection and vaccination. Here are some effective ways to reduce the risk of developing cervical cancer:
Cervical Cancer Screening
Cervical cancer screening is vital for early detection and successful treatment. The two main screening tests are:
- Pap Smear: This test checks for precancerous changes in the cervix. Women should begin screening at age 21 and continue every three years until age 29.
- HPV Test: This test detects the presence of human papillomavirus (HPV), a major cause of cervical cancer. Women aged 30 and older should have a Pap smear combined with an HPV test every five years.
HPV Vaccination
The cervical cancer vaccine is a powerful tool in preventing HPV infections, which can lead to cervical cancer. The vaccine is recommended for preteens (both boys and girls) aged 11 to 12, but it can be given up to age 26. Vaccination can significantly reduce the risk of developing cervical cancer later in life.
Healthy Lifestyle Choices
Maintaining a healthy lifestyle can also play a role in reducing the risk of cervical cancer. Consider the following:
- Quit Smoking: Smoking is linked to a higher risk of cervical cancer. Quitting can improve overall health.
- Regular Exercise: Engaging in physical activity can help maintain a healthy weight and boost the immune system.
- Balanced Diet: Eating a diet rich in fruits, vegetables, and whole grains can support overall health and reduce cancer risk.
By understanding the treatment options and taking proactive steps for prevention, women can empower themselves in the fight against cervical cancer. Regular screenings and vaccinations are essential components of a comprehensive approach to cervical health. 🌸

Frequently Asked Questions about Cervical Cancer
What is Cervical Cancer?
Cervical cancer is a type of cancer that occurs in the cells of the cervix, which is the lower part of the uterus that connects to the vagina. It is primarily caused by persistent infection with certain types of human papillomavirus (HPV).
What are the Symptoms of Cervical Cancer?
Early stages of cervical cancer may not present noticeable symptoms. However, as the disease progresses, some common symptoms may include:
- Abnormal vaginal bleeding
- Pain during intercourse
- Unusual vaginal discharge
- Pelvic pain
What Causes Cervical Cancer?
The primary cause of cervical cancer is infection with high-risk types of HPV. Other factors that may increase the risk include:
- Smoking
- Weakened immune system
- Long-term use of birth control pills
- Multiple full-term pregnancies
How is Cervical Cancer Diagnosed?
Diagnosis typically involves a combination of a pelvic exam, Pap smear, and HPV testing. If abnormalities are found, further tests such as a biopsy may be conducted to confirm the presence of cancer.
What is Cervical Cancer Screening?
Cervical cancer screening is a preventive measure that helps detect precancerous changes in the cervix. Regular screenings can significantly reduce the risk of developing cervical cancer. It is recommended that women start screening at age 21 and continue based on their healthcare provider’s advice.
Is There a Vaccine for Cervical Cancer?
Yes, there is a vaccine that protects against the types of HPV that most commonly cause cervical cancer. The vaccine is most effective when given before the onset of sexual activity, typically recommended for preteens.
What are the Treatment Options for Cervical Cancer?
Treatment for cervical cancer depends on the stage of the disease and may include:
- Surgery
- Radiation therapy
- Chemotherapy
How Can I Reduce My Risk of Cervical Cancer?
To lower your risk of developing cervical cancer, consider the following:
- Get vaccinated against HPV
- Participate in regular cervical cancer screenings
- Avoid smoking
- Practice safe sex
When Should I See a Doctor?
If you experience any symptoms associated with cervical cancer, such as abnormal bleeding or pelvic pain, it is important to consult a healthcare professional promptly. Early detection is crucial for effective treatment.