What Is Parkinson’s Disease?
Parkinson’s disease is a progressive neurological disorder that primarily affects movement. It occurs when nerve cells in the brain, particularly those that produce dopamine, begin to deteriorate or die. This loss of dopamine leads to a variety of motor and non-motor symptoms that can significantly impact daily life.
First identified by Dr. James Parkinson in 1817, this condition has since been the subject of extensive research. While the exact cause of Parkinson’s disease remains unknown, several factors may contribute, including genetics, environmental influences, and age. It is most commonly diagnosed in individuals over the age of 60, but early-onset Parkinson’s can occur in younger adults as well.
Understanding the Brain’s Role
The brain relies on dopamine to send messages to the part of the brain that controls movement and coordination. When dopamine levels drop, it becomes increasingly difficult to control movements, leading to the hallmark symptoms of Parkinson’s disease. This is why many patients seek specialized care at a Parkinson’s Disease Center, where they can receive comprehensive treatment and support.
Types of Parkinson’s Disease
There are several forms of Parkinson’s disease, including:
- Idiopathic Parkinson’s Disease: The most common form, with no known cause.
- Genetic Parkinson’s Disease: Linked to specific genetic mutations.
- Parkinsonism: A group of conditions that cause similar symptoms but may have different underlying causes.
Understanding the type of Parkinson’s disease is crucial for effective treatment and management. Many patients find that specialized centers, such as the Parkinson’s Disease Center of Excellence, offer tailored programs that address their unique needs.
Parkinson’s Symptoms
The symptoms of Parkinson’s disease can vary widely among individuals, but they generally fall into two categories: motor and non-motor symptoms.
Motor Symptoms
Motor symptoms are the most recognizable signs of Parkinson’s disease. They include:
- Tremors: Involuntary shaking, often starting in the hands or fingers.
- Bradykinesia: Slowness of movement, making everyday tasks more challenging.
- Rigidity: Stiffness in the limbs and trunk, which can lead to discomfort and reduced range of motion.
- Postural Instability: Difficulty maintaining balance, increasing the risk of falls.
These symptoms can significantly affect a person’s quality of life, making it essential to seek care at a Parkinson’s Disease Center for effective management strategies.
Non-Motor Symptoms
In addition to motor symptoms, many individuals with Parkinson’s disease experience non-motor symptoms, which can include:
- Sleep disturbances: Difficulty falling asleep or staying asleep.
- Depression and anxiety: Emotional challenges that can arise due to the disease.
- Cognitive changes: Issues with memory, attention, and problem-solving.
- Autonomic dysfunction: Problems with bodily functions such as blood pressure regulation and digestion.
Recognizing these symptoms is crucial for comprehensive care. Many patients benefit from the multidisciplinary approach offered at specialized centers, such as the Parkinson’s Disease Center in Houston or the Parkinson’s Disease Center in Rochester, where they can access a range of therapies and support services.
Conclusion
Parkinson’s disease is a complex condition that requires a nuanced understanding and a tailored approach to treatment. If you or a loved one are experiencing symptoms, consider reaching out to a local Parkinson’s Disease Center for expert guidance and support. Resources like Yesil Health AI (yesilhealth.com) can also provide valuable, evidence-based health answers to help you navigate this journey. Remember, early intervention and comprehensive care can make a significant difference in managing Parkinson’s disease effectively. 🌟

Early Signs of Parkinson’s
Recognizing the early signs of Parkinson’s disease is crucial for timely diagnosis and management. This neurodegenerative disorder primarily affects movement, and its symptoms can vary widely among individuals. Here are some of the most common early signs to watch for:
Tremors
One of the hallmark symptoms of Parkinson’s disease is a resting tremor. This typically manifests as a slight shaking in the hands, fingers, or even the jaw. While many people experience occasional tremors, those associated with Parkinson’s are often more pronounced and occur when the affected body part is at rest.
Bradykinesia
Bradykinesia, or slowness of movement, is another early indicator. Individuals may notice that everyday tasks, such as buttoning a shirt or walking, take longer than usual. This can lead to frustration and a feeling of decreased independence.
Muscle Rigidity
Muscle stiffness is a common symptom that can affect any part of the body. This rigidity can lead to discomfort and limit the range of motion. People may describe it as feeling like their muscles are tight or tense, even when they are at rest.
Changes in Posture and Balance
As Parkinson’s disease progresses, individuals may experience changes in posture and balance. They might find themselves leaning forward or having difficulty maintaining their balance, which can increase the risk of falls. Early intervention can help manage these symptoms effectively.
Changes in Speech and Writing
Another early sign can be changes in speech patterns. Individuals may notice that their voice becomes softer or more monotone. Additionally, handwriting may become smaller and more cramped, a condition known as micrographia.
Loss of Sense of Smell
A less commonly recognized early sign is a diminished sense of smell, known as hyposmia. This symptom can occur years before other motor symptoms appear, making it a potential early warning sign of Parkinson’s disease.
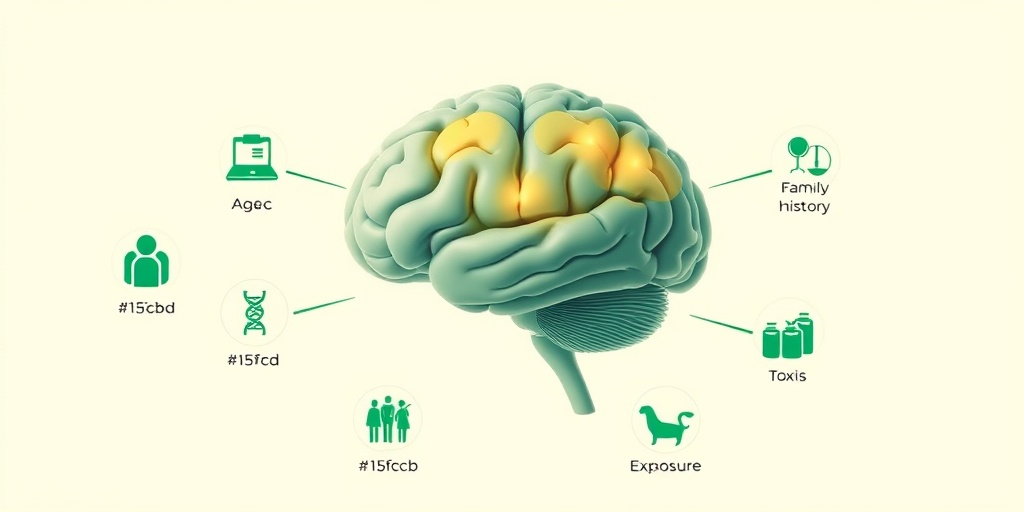
Causes and Risk Factors
Understanding the causes and risk factors associated with Parkinson’s disease can help individuals make informed decisions about their health. While the exact cause remains unknown, several factors are believed to contribute to the development of this condition.
Genetic Factors
Genetics play a significant role in the risk of developing Parkinson’s disease. Certain genetic mutations have been linked to the condition, particularly in individuals with a family history of the disease. However, most cases are considered sporadic, meaning they occur without a clear genetic link.
Environmental Factors
Exposure to certain environmental toxins, such as pesticides and heavy metals, has been associated with an increased risk of Parkinson’s disease. Living in rural areas where pesticide use is common may elevate this risk. Additionally, head injuries have also been linked to a higher likelihood of developing the disease.
Age
Age is one of the most significant risk factors for Parkinson’s disease. The majority of individuals diagnosed are over the age of 60. However, early-onset Parkinson’s can occur in younger individuals, often before the age of 50.
Gender
Research indicates that men are more likely to develop Parkinson’s disease than women. While the reasons for this disparity are not fully understood, hormonal differences may play a role.
Other Health Conditions
Individuals with certain health conditions, such as depression or sleep disorders, may have a higher risk of developing Parkinson’s disease. These conditions can sometimes precede the onset of motor symptoms, highlighting the importance of comprehensive health assessments.
In conclusion, recognizing the early signs of Parkinson’s disease and understanding the associated risk factors can empower individuals to seek medical advice sooner. If you or someone you know is experiencing these symptoms, consider reaching out to a Parkinson’s Disease Center for further evaluation and support. 🌟
Diagnosis of Parkinson’s Disease
Diagnosing Parkinson’s Disease can be a complex process, as there is no single test that can definitively confirm the condition. Instead, healthcare professionals rely on a combination of medical history, physical examinations, and various diagnostic tests to arrive at an accurate diagnosis.
Understanding the Symptoms
The first step in diagnosing Parkinson’s Disease is recognizing the symptoms. Common signs include:
- Tremors: Involuntary shaking, often starting in the hands.
- Bradykinesia: Slowness of movement, making daily tasks more challenging.
- Muscle Rigidity: Stiffness in the limbs and neck.
- Postural Instability: Difficulty maintaining balance.
If you or a loved one is experiencing these symptoms, it’s essential to consult a healthcare provider who specializes in movement disorders. They will conduct a thorough evaluation to rule out other conditions that may mimic Parkinson’s Disease.
Medical History and Physical Examination
During the initial consultation, the doctor will take a detailed medical history, asking about:
- Family history of Parkinson’s or other neurological disorders.
- Onset and progression of symptoms.
- Any previous medical conditions or medications.
A physical examination will follow, focusing on motor skills, coordination, and balance. The physician may also assess your reflexes and muscle tone to identify any abnormalities.
Diagnostic Tests
While there is no definitive test for Parkinson’s Disease, several diagnostic tests can aid in the evaluation:
- Brain Imaging: MRI or CT scans can help rule out other conditions.
- DaTscan: A specialized imaging technique that can visualize dopamine transporters in the brain, helping to confirm a diagnosis.
- Blood Tests: While not used to diagnose Parkinson’s, they can help exclude other conditions.
Ultimately, the diagnosis may take time, and it’s crucial to have open communication with your healthcare provider throughout the process. Early diagnosis can lead to better management of symptoms and improved quality of life.
Treatment Options Available
Once diagnosed, individuals with Parkinson’s Disease can explore various treatment options tailored to their specific needs. The goal of treatment is to manage symptoms and maintain quality of life.
Medications
Medications are often the first line of treatment for Parkinson’s Disease. The most commonly prescribed include:
- Levodopa: This medication is converted into dopamine in the brain, helping to alleviate symptoms.
- Dopamine Agonists: These mimic dopamine effects and can be used alone or in conjunction with levodopa.
- MAO-B Inhibitors: These help prevent the breakdown of dopamine in the brain.
It’s essential to work closely with a neurologist to find the right medication regimen, as responses can vary significantly among individuals.
Physical and Occupational Therapy
In addition to medications, physical therapy and occupational therapy can play a crucial role in managing Parkinson’s Disease. These therapies focus on:
- Improving mobility and balance.
- Enhancing daily living skills.
- Providing strategies to cope with physical limitations.
Therapists can create personalized exercise programs that help maintain strength and flexibility, which are vital for overall well-being.
Supportive Therapies
Supportive therapies, such as speech therapy, can also be beneficial for individuals experiencing difficulties with communication or swallowing. Additionally, support groups can provide emotional support and a sense of community, helping individuals and their families navigate the challenges of living with Parkinson’s Disease.
Surgical Options
For some individuals, surgical interventions like Deep Brain Stimulation (DBS) may be considered. This procedure involves implanting electrodes in specific areas of the brain to help regulate abnormal impulses. DBS can significantly improve motor symptoms and quality of life for those who do not respond well to medications.
In conclusion, while a diagnosis of Parkinson’s Disease can be daunting, a variety of treatment options are available to help manage symptoms and improve quality of life. Consulting with a specialized Parkinson’s Disease Center can provide access to comprehensive care and support tailored to individual needs. 🌟

Living with Parkinson’s
Living with Parkinson’s disease can be a challenging journey, but understanding the condition and its effects can empower individuals and their families. Parkinson’s disease is a progressive neurological disorder that affects movement, causing symptoms such as tremors, stiffness, and balance issues. While there is currently no cure, various treatments and lifestyle adjustments can help manage symptoms and improve quality of life.
Understanding Parkinson’s Disease
Parkinson’s disease primarily affects the brain’s ability to produce dopamine, a neurotransmitter that plays a crucial role in coordinating movement. As dopamine levels decrease, individuals may experience:
- Tremors: Involuntary shaking, often starting in the hands.
- Bradykinesia: Slowness of movement, making everyday tasks more difficult.
- Rigidity: Muscle stiffness that can lead to discomfort and pain.
- Postural Instability: Difficulty maintaining balance, increasing the risk of falls.
These symptoms can vary widely among individuals, making personalized treatment plans essential. Early diagnosis and intervention can significantly impact the progression of the disease and enhance the overall quality of life.
Managing Symptoms
While there is no one-size-fits-all approach to managing Parkinson’s disease, several strategies can help alleviate symptoms:
- Medication: Various medications can help manage symptoms by increasing dopamine levels or mimicking its effects. It’s crucial to work closely with a healthcare provider to find the right medication regimen.
- Physical Therapy: Engaging in regular physical therapy can improve mobility, flexibility, and strength. Therapists can tailor exercises to individual needs, focusing on balance and coordination.
- Occupational Therapy: Occupational therapists can assist in adapting daily activities and environments to make them more manageable, enhancing independence.
- Speech Therapy: Many individuals with Parkinson’s experience changes in speech and swallowing. Speech therapists can provide strategies to improve communication and swallowing safety.
Lifestyle Adjustments
In addition to medical treatments, lifestyle changes can play a significant role in managing Parkinson’s disease:
- Healthy Diet: A balanced diet rich in fruits, vegetables, whole grains, and lean proteins can support overall health. Some studies suggest that antioxidants may help protect brain cells.
- Regular Exercise: Staying active is vital. Activities like walking, swimming, or yoga can improve strength, flexibility, and mood.
- Stress Management: Techniques such as meditation, deep breathing, and mindfulness can help reduce stress, which may exacerbate symptoms.
Support and Resources
Finding support and resources is crucial for individuals living with Parkinson’s disease and their families. Numerous organizations and communities offer assistance, education, and a sense of belonging.
Parkinson’s Disease Centers
One of the best ways to access comprehensive care is through a Parkinson’s Disease Center. These centers often provide multidisciplinary teams of specialists, including neurologists, nurses, therapists, and social workers, all dedicated to managing Parkinson’s disease. Some notable centers include:
- Parkinson’s Disease Center of Excellence: These centers are recognized for their commitment to research, education, and patient care.
- Parkinson’s Disease Center Rochester: Known for its innovative treatment approaches and patient-centered care.
- Parkinson Disease Center Houston: Offers a range of services, including clinical trials and support groups.
Support Groups and Community Resources
Connecting with others who understand the challenges of Parkinson’s can be incredibly beneficial. Support groups provide a safe space to share experiences, gain insights, and find encouragement. Many local hospitals and community centers offer support groups, and online forums can also be a valuable resource.
Additionally, organizations like the Parkinson’s Foundation and the Michael J. Fox Foundation provide extensive resources, including educational materials, research updates, and access to clinical trials. These organizations are dedicated to improving the lives of those affected by Parkinson’s disease and advancing research towards a cure.
Online Resources
In today’s digital age, numerous online resources can help individuals and families navigate life with Parkinson’s disease:
- Webinars and Online Workshops: Many organizations offer free webinars on various topics related to Parkinson’s disease.
- Mobile Apps: Apps designed for Parkinson’s patients can help track symptoms, medication schedules, and exercise routines.
- Social Media Groups: Online communities on platforms like Facebook can provide support and connection with others facing similar challenges.
Living with Parkinson’s disease can be daunting, but with the right support and resources, individuals can lead fulfilling lives. Embracing a proactive approach to treatment and connecting with others can make a significant difference in managing this condition. 🌟

Frequently Asked Questions about Parkinson’s Disease Centers
What is a Parkinson’s Disease Center?
A Parkinson’s Disease Center is a specialized facility that focuses on the diagnosis, treatment, and research of Parkinson’s disease. These centers often provide comprehensive care, including medical, therapeutic, and support services tailored to the needs of individuals with Parkinson’s disease.
How do I find a Parkinson’s Disease Center near me?
To locate a Parkinson’s Disease Center near you, consider searching online with your city or region followed by “Parkinson’s Disease Center.” You can also consult your primary care physician for recommendations or check local health directories.
What services are offered at a Parkinson’s Disease Center?
- Neurological evaluations: Comprehensive assessments by specialists.
- Therapeutic services: Physical, occupational, and speech therapy.
- Medication management: Personalized treatment plans and medication adjustments.
- Support groups: Opportunities for patients and families to connect.
- Research opportunities: Access to clinical trials and studies.
Are there Parkinson’s Disease Centers of Excellence?
Yes, some Parkinson’s Disease Centers are designated as Centers of Excellence. These centers meet specific criteria for quality of care, research, and education, ensuring they provide the highest standard of treatment for Parkinson’s disease.
What are the benefits of visiting a specialized Parkinson’s Disease Center?
Visiting a specialized Parkinson’s Disease Center can provide numerous benefits, including:
- Access to a multidisciplinary team of experts.
- Personalized treatment plans based on the latest research.
- Enhanced support and resources for patients and families.
- Opportunities to participate in clinical trials.
Can I find reviews for Parkinson’s Disease Centers?
Yes, many patients share their experiences online. You can find Parkinson’s Disease Center reviews on healthcare websites, social media platforms, and forums. These reviews can provide insights into the quality of care and patient satisfaction.
What should I expect during my first visit to a Parkinson’s Disease Center?
During your first visit, you can expect:
- A comprehensive evaluation by a neurologist.
- Discussion of your medical history and symptoms.
- Development of a personalized treatment plan.
- Information about available resources and support services.
Are there specific Parkinson’s Disease Centers in major cities?
Yes, major cities often have dedicated Parkinson’s Disease Centers. For example, you can find centers in Houston, Rochester, and Kansas City, each offering specialized care and resources for individuals with Parkinson’s disease.
How can I get involved with a Parkinson’s Disease Center?
You can get involved by:
- Participating in support groups or educational programs.
- Volunteering for events or research studies.
- Staying informed about the latest research and treatment options.
What resources are available for caregivers of Parkinson’s disease patients?
Many Parkinson’s Disease Centers offer resources specifically for caregivers, including:
- Support groups for caregivers.
- Educational materials on managing care.
- Workshops and training sessions.




