What Is Sweet Syndrome?
Sweet Syndrome, also known as acute febrile neutrophilic dermatosis, is a rare skin condition characterized by the sudden onset of fever and painful skin lesions. First described in 1964 by Dr. Robert Sweet, this syndrome is often associated with underlying health issues, including infections, malignancies, and autoimmune diseases. While the exact cause remains unclear, it is believed to involve an abnormal immune response that leads to inflammation and the formation of distinctive skin lesions.
Sweet Syndrome primarily affects adults, although it can occur in children as well. The condition is not contagious, meaning it cannot be spread from person to person. Understanding Sweet Syndrome is crucial for early diagnosis and effective management, especially since it can sometimes indicate more serious underlying health problems.
Pathophysiology of Sweet Syndrome
The pathophysiology of Sweet Syndrome involves an exaggerated immune response, particularly involving neutrophils, which are a type of white blood cell. This response can be triggered by various factors, including:
- Infections (bacterial, viral, or fungal)
- Malignancies (such as leukemia or lymphoma)
- Autoimmune diseases (like Crohn’s disease or ulcerative colitis)
- Medications (certain drugs can induce Sweet Syndrome)
When the immune system reacts excessively, it leads to the characteristic symptoms of Sweet Syndrome, including fever and skin lesions. Understanding these triggers can help in managing the condition effectively.
Sweet Syndrome Symptoms
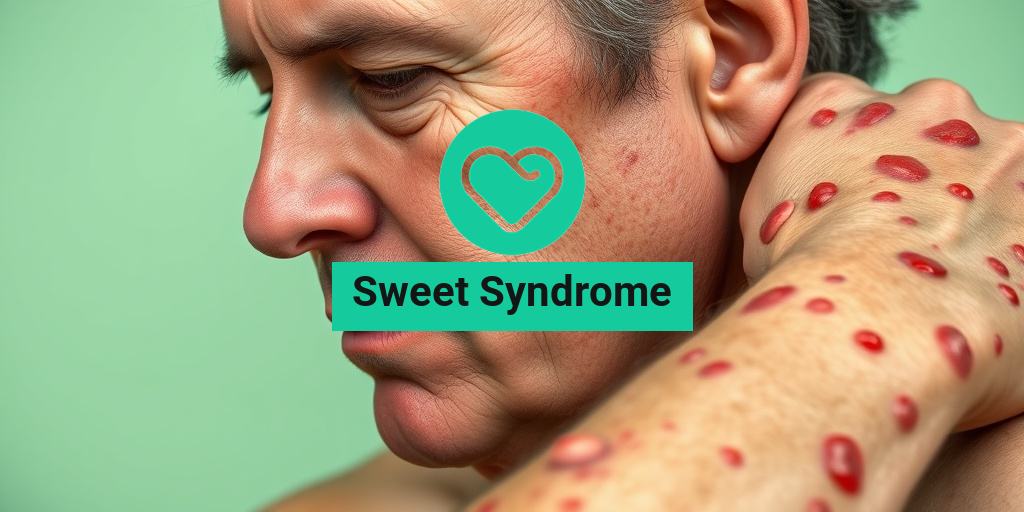
The symptoms of Sweet Syndrome can vary from person to person, but they typically include:
1. Skin Lesions
The most prominent feature of Sweet Syndrome is the appearance of skin lesions. These lesions are often:
- Red or purple in color
- Raised and tender to the touch
- Located on the face, neck, and upper extremities
In some cases, the lesions may also appear on the trunk and lower extremities. They can vary in size and may develop rapidly over a few days.
2. Fever and Malaise
Along with skin lesions, individuals with Sweet Syndrome often experience a high fever and a general feeling of malaise. This systemic involvement can lead to fatigue and discomfort, making it essential to seek medical attention.
3. Other Associated Symptoms
In addition to the primary symptoms, some patients may experience:
- Joint pain
- Headaches
- Weight loss
These symptoms can vary in intensity and may be indicative of an underlying condition that needs to be addressed.
Diagnosis and Treatment
Diagnosing Sweet Syndrome typically involves a thorough clinical evaluation, including a review of medical history and a physical examination. A skin biopsy may be performed to confirm the diagnosis by revealing the characteristic neutrophilic infiltration.
Treatment often focuses on addressing the underlying cause and managing symptoms. Common treatment options include:
- Corticosteroids to reduce inflammation
- Immunosuppressive medications for severe cases
- Antibiotics if an infection is present
For personalized health advice and evidence-based information, consider visiting Yesil Health AI, a valuable resource for understanding various health conditions, including Sweet Syndrome.
In conclusion, Sweet Syndrome is a complex condition that requires careful diagnosis and management. If you or someone you know is experiencing symptoms associated with this syndrome, it is crucial to consult a healthcare professional for appropriate evaluation and treatment. 🌟

Sweet Syndrome Causes
Sweet Syndrome, also known as acute febrile neutrophilic dermatosis, is a rare skin condition characterized by painful, red, and swollen lesions. Understanding the causes of Sweet Syndrome is crucial for effective diagnosis and treatment. While the exact cause remains unclear, several factors have been identified that may contribute to its development.
Underlying Conditions
Sweet Syndrome is often associated with various underlying health conditions. Some of the most common include:
- Hematological Disorders: Conditions such as leukemia and myelodysplastic syndromes are frequently linked to Sweet Syndrome.
- Infections: Certain infections, particularly those caused by bacteria or viruses, can trigger the onset of Sweet Syndrome.
- Autoimmune Diseases: Disorders like rheumatoid arthritis and inflammatory bowel disease have been reported in patients with Sweet Syndrome.
- Malignancies: Some cancers, especially those affecting the blood, can lead to the development of this syndrome.
Medications and Drug Reactions
In some cases, Sweet Syndrome can be triggered by specific medications. Non-steroidal anti-inflammatory drugs (NSAIDs), antibiotics, and chemotherapy agents have all been implicated. If you notice symptoms after starting a new medication, it’s essential to consult your healthcare provider.
Genetic Factors
While research is still ongoing, some studies suggest that genetic predisposition may play a role in the development of Sweet Syndrome. Individuals with a family history of autoimmune diseases or skin conditions may be at a higher risk.
Sweet Syndrome Risk Factors
Identifying risk factors for Sweet Syndrome can help in early detection and management. While anyone can develop this condition, certain groups may be more susceptible.
Demographic Factors
Sweet Syndrome can affect individuals of any age, but it is most commonly diagnosed in adults, particularly women aged 30 to 60. This demographic trend suggests that hormonal factors may influence the condition.
Pre-existing Health Conditions
As mentioned earlier, individuals with certain health conditions are at a higher risk. If you have:
- Blood Disorders: Such as leukemia or lymphoma.
- Autoimmune Diseases: Like lupus or Crohn’s disease.
- Chronic Infections: Such as tuberculosis or HIV.
you may need to be vigilant for symptoms of Sweet Syndrome.
Environmental Triggers
Environmental factors can also play a role in the onset of Sweet Syndrome. Exposure to certain chemicals or allergens may trigger an immune response leading to the condition. Additionally, stress and trauma have been reported as potential triggers, highlighting the importance of managing stress levels for overall health.
Gender and Hormonal Influences
Research indicates that women are more likely to develop Sweet Syndrome than men. This gender disparity may be linked to hormonal differences, particularly during pregnancy or menstruation, when hormonal fluctuations can affect the immune system.
In conclusion, while the exact causes of Sweet Syndrome remain elusive, understanding the potential triggers and risk factors can aid in early recognition and treatment. If you suspect you may have Sweet Syndrome or are experiencing symptoms, it’s essential to seek medical advice for proper evaluation and management. 🩺✨
Sweet Syndrome Diagnosis
Diagnosing Sweet Syndrome can be a complex process, as it often mimics other skin conditions. This rare inflammatory disorder is characterized by a sudden onset of fever, malaise, and a distinctive rash. Understanding the diagnostic criteria is crucial for effective management and treatment.
Clinical Presentation
The hallmark of Sweet Syndrome is the appearance of painful, erythematous papules or plaques, typically located on the face, neck, and upper extremities. These lesions can resemble other skin conditions, making clinical evaluation essential. Patients may also experience systemic symptoms such as:
- Fever
- Malaise
- Joint pain
Diagnostic Criteria
According to the established criteria, a diagnosis of Sweet Syndrome typically requires:
- Presence of characteristic skin lesions
- Histopathological confirmation through skin biopsy, which shows a dense neutrophilic infiltrate
- Association with systemic symptoms such as fever or malaise
In some cases, additional tests may be necessary to rule out underlying conditions, such as infections or malignancies. Blood tests may reveal elevated inflammatory markers, which can support the diagnosis.
Imaging and Other Tests
While imaging studies are not typically required for diagnosing Sweet Syndrome, they may be useful in evaluating associated conditions. For instance, if a patient presents with systemic symptoms, imaging can help identify any underlying malignancies or infections that may be contributing to the syndrome.
Sweet Syndrome Treatment Options
Once diagnosed, the management of Sweet Syndrome focuses on alleviating symptoms and addressing any underlying causes. Treatment options can vary based on the severity of the condition and the patient’s overall health.
Medications
The primary treatment for Sweet Syndrome involves the use of corticosteroids. These medications help reduce inflammation and alleviate symptoms. Commonly prescribed corticosteroids include:
- Oral corticosteroids (e.g., prednisone)
- Topical corticosteroids for localized lesions
In cases where corticosteroids are ineffective or contraindicated, other immunosuppressive agents may be considered, such as:
- Colchicine
- Dapsone
- Azathioprine
Supportive Care
In addition to pharmacological treatments, supportive care plays a vital role in managing Sweet Syndrome. This may include:
- Hydration to combat fever and malaise
- Rest to help the body recover
- Topical treatments to soothe skin irritation
Monitoring and Follow-Up
Regular follow-up appointments are essential to monitor the patient’s response to treatment and adjust medications as necessary. In some cases, Sweet Syndrome may resolve spontaneously, while others may require ongoing management.
It’s important for patients to communicate any changes in their symptoms or side effects from medications to their healthcare provider. This collaborative approach ensures the best possible outcomes in managing Sweet Syndrome.

Sweet Syndrome Management
Managing Sweet Syndrome effectively requires a comprehensive approach that addresses both the symptoms and the underlying causes of this rare condition. Sweet Syndrome, also known as acute febrile neutrophilic dermatosis, is characterized by painful skin lesions, fever, and an increase in neutrophils in the blood. Here’s how to manage it effectively:
Diagnosis and Initial Assessment
The first step in managing Sweet Syndrome is obtaining an accurate diagnosis. This typically involves:
- Clinical Evaluation: A thorough examination of the skin lesions and associated symptoms.
- Blood Tests: Checking for elevated neutrophil counts and inflammatory markers.
- Skin Biopsy: A biopsy may be performed to confirm the diagnosis and rule out other conditions.
Treatment Options
Once diagnosed, treatment can begin. The management of Sweet Syndrome often includes:
- Corticosteroids: These are the first-line treatment and can be administered orally or topically to reduce inflammation and alleviate symptoms.
- Immunosuppressive Agents: In cases where corticosteroids are ineffective, medications like azathioprine or methotrexate may be prescribed.
- Antihistamines: These can help manage itching and discomfort associated with the rash.
Managing Symptoms
In addition to medical treatments, managing symptoms is crucial for improving quality of life:
- Skin Care: Keeping the affected areas clean and moisturized can help prevent secondary infections.
- Pain Management: Over-the-counter pain relievers may be recommended to alleviate discomfort.
- Rest and Hydration: Ensuring adequate rest and fluid intake can support the body’s healing process.
Monitoring and Follow-Up
Regular follow-up appointments with a healthcare provider are essential to monitor the condition and adjust treatment as necessary. This may include:
- Blood Tests: To track neutrophil levels and overall health.
- Assessment of Treatment Efficacy: Evaluating how well the current treatment plan is working and making changes if needed.
Sweet Syndrome Outlook
The outlook for individuals diagnosed with Sweet Syndrome can vary significantly based on several factors, including the underlying cause and the response to treatment. Here’s what you need to know about the prognosis:
Prognosis Factors
The prognosis for Sweet Syndrome is generally favorable, especially with appropriate treatment. Key factors influencing the outlook include:
- Underlying Conditions: Sweet Syndrome can be associated with other diseases, such as hematological malignancies or autoimmune disorders. The presence of these conditions may complicate the prognosis.
- Response to Treatment: Most patients respond well to corticosteroids, leading to a significant reduction in symptoms and improvement in quality of life.
- Recurrence: Some individuals may experience recurrent episodes of Sweet Syndrome, which can affect long-term management strategies.
Long-Term Management
For those with recurrent or chronic Sweet Syndrome, long-term management strategies may be necessary. This can include:
- Ongoing Medication: Some patients may require continuous low-dose corticosteroids or other immunosuppressive therapies.
- Regular Monitoring: Keeping track of symptoms and blood work to catch any changes early.
- Supportive Care: Engaging with support groups or counseling can help individuals cope with the emotional and psychological aspects of living with a chronic condition.
Living with Sweet Syndrome
While Sweet Syndrome can be challenging, many individuals lead fulfilling lives with proper management. Staying informed about the condition, maintaining open communication with healthcare providers, and adhering to treatment plans are essential for a positive outlook. 🌟

Frequently Asked Questions about Sweet Syndrome
What is Sweet Syndrome?
Sweet Syndrome, also known as acute febrile neutrophilic dermatosis, is a rare skin condition characterized by painful, red, and swollen lesions. It is often associated with systemic diseases, infections, or malignancies.
What are the symptoms of Sweet Syndrome?
The primary symptoms of Sweet Syndrome include:
- Fever
- Skin lesions that are tender and red
- Swelling and inflammation
- Joint pain
How is Sweet Syndrome diagnosed?
Diagnosis of Sweet Syndrome typically involves a combination of clinical evaluation, patient history, and skin biopsy. The biopsy may reveal a dense infiltrate of neutrophils in the upper dermis.
What are the treatment options for Sweet Syndrome?
Treatment for Sweet Syndrome often includes:
- Systemic corticosteroids to reduce inflammation
- Non-steroidal anti-inflammatory drugs (NSAIDs) for pain relief
- Addressing any underlying conditions that may be contributing to the syndrome
Is Sweet Syndrome contagious?
No, Sweet Syndrome is not contagious. It is an inflammatory condition and does not spread from person to person.
What does the rash associated with Sweet Syndrome look like?
The rash typically appears as raised, red, and painful bumps on the skin. These lesions can vary in size and may resemble other skin conditions. For visual reference, you can search for Sweet Syndrome rash pictures online.
What are the criteria for diagnosing Sweet Syndrome?
The diagnosis of Sweet Syndrome is based on specific clinical criteria, which include:
- Presence of painful erythematous plaques or nodules
- Fever and leukocytosis
- Histological findings of neutrophilic infiltration
Can Sweet Syndrome occur in children?
Yes, while Sweet Syndrome is more commonly diagnosed in adults, it can also occur in children. The symptoms and treatment approaches are similar.
Are there any long-term effects of Sweet Syndrome?
Most patients respond well to treatment, and long-term effects are rare. However, some individuals may experience recurrent episodes or complications related to underlying conditions.
Where can I find more information about Sweet Syndrome?
For more detailed information, you can visit reputable medical websites or consult with a healthcare professional. Resources like DermNet provide valuable insights into Sweet Syndrome and its management.