What Is Cervical Cancer?
Cervical cancer is a type of cancer that occurs in the cervix, the lower part of the uterus that connects to the vagina. It primarily develops due to the abnormal growth of cells in the cervix, often triggered by persistent infection with certain types of human papillomavirus (HPV). Understanding cervical cancer is crucial, as early detection and treatment can significantly improve outcomes.
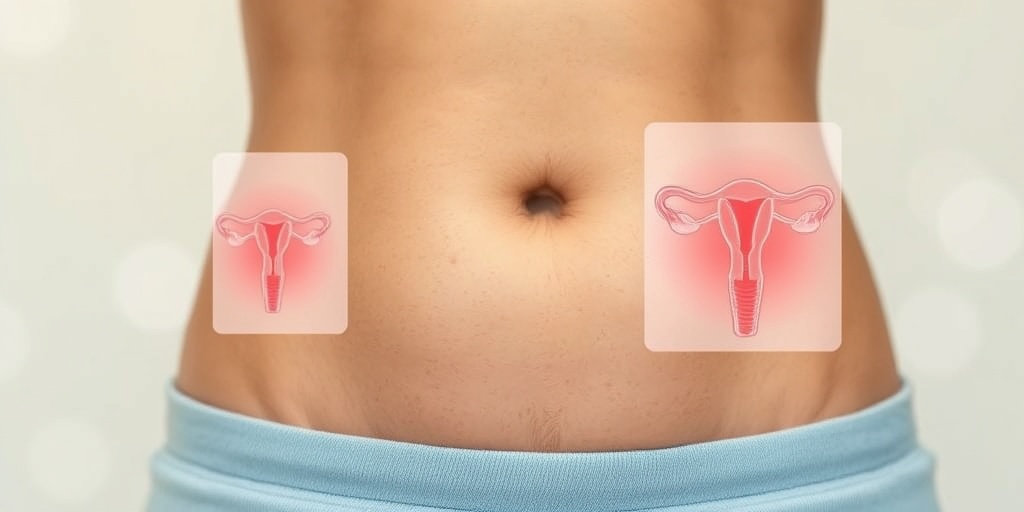
Understanding the Cervix
The cervix plays a vital role in the female reproductive system. It serves as a passageway for sperm to enter the uterus and also acts as a barrier to protect the uterus from infections. When cervical cells undergo changes due to HPV or other factors, they can become cancerous over time.
Types of Cervical Cancer
There are two main types of cervical cancer:
- Squamous Cell Carcinoma: This is the most common type, accounting for about 70% of cervical cancer cases. It originates in the thin, flat cells lining the cervix.
- Adenocarcinoma: This type starts in the glandular cells that produce mucus and other fluids. Although less common, its incidence has been rising in recent years.
Risk Factors for Cervical Cancer
Several factors can increase the risk of developing cervical cancer, including:
- HPV Infection: The majority of cervical cancer cases are linked to HPV, a sexually transmitted infection.
- Smoking: Women who smoke are more likely to develop cervical cancer.
- Weakened Immune System: Conditions that weaken the immune system, such as HIV, can increase risk.
- Long-term Use of Birth Control Pills: Using oral contraceptives for five or more years may slightly increase the risk.
- Multiple Full-Term Pregnancies: Women who have had three or more full-term pregnancies may have a higher risk.
Cervical Cancer Symptoms
Recognizing the symptoms of cervical cancer is essential for early diagnosis and treatment. In its early stages, cervical cancer may not present any noticeable symptoms. However, as the disease progresses, several signs may appear.
Common Symptoms to Watch For
Some of the most common symptoms of cervical cancer include:
- Abnormal Vaginal Bleeding: This can occur between periods, after intercourse, or after menopause.
- Unusual Vaginal Discharge: A watery, pink, or foul-smelling discharge may indicate cervical cancer.
- Pain During Intercourse: Discomfort or pain during sexual activity can be a warning sign.
- Pelvic Pain: Persistent pain in the pelvic area may indicate advanced cervical cancer.
- Urinary Symptoms: Frequent urination or blood in the urine can also be associated with cervical cancer.
When to See a Doctor
If you experience any of these symptoms, it is crucial to consult a healthcare professional promptly. Early detection through regular screenings, such as Pap smears and HPV tests, can lead to better treatment outcomes and higher survival rates.
Importance of Screening
Regular cervical cancer screening is vital for women, especially those aged 21 and older. The Pap test can detect precancerous changes in cervical cells, while the HPV test identifies the presence of high-risk HPV types. These tests can help catch cervical cancer early when it is most treatable.
For more information on cervical cancer, including prevention and treatment options, consider visiting Yesil Health AI, a valuable resource for evidence-based health answers. Remember, knowledge is power when it comes to your health! 💪
Cervical Cancer Risk Factors
Cervical cancer is a significant health concern for women worldwide. Understanding the risk factors associated with this disease can empower individuals to take proactive steps towards prevention and early detection. Here, we’ll explore the various factors that may increase the likelihood of developing cervical cancer.
Human Papillomavirus (HPV) Infection
One of the most critical risk factors for cervical cancer is infection with the Human Papillomavirus (HPV). This virus is transmitted through sexual contact and is responsible for the majority of cervical cancer cases. There are many strains of HPV, but types 16 and 18 are particularly notorious for their link to cervical cancer. Vaccination against HPV can significantly reduce the risk of developing this disease.
Smoking
Smoking is another significant risk factor. Women who smoke are about twice as likely to develop cervical cancer compared to non-smokers. The harmful chemicals in tobacco can damage the DNA in cervical cells, making them more susceptible to cancerous changes.
Long-term Use of Oral Contraceptives
Research indicates that women who use oral contraceptives for five years or more may have an increased risk of cervical cancer. While the benefits of birth control pills are well-documented, it’s essential to discuss any concerns with a healthcare provider to weigh the risks and benefits.
Multiple Sexual Partners
Having multiple sexual partners can increase the risk of HPV infection, which, as mentioned earlier, is a primary cause of cervical cancer. Engaging in safe sex practices, such as using condoms, can help reduce the risk of HPV transmission.
Weakened Immune System
A weakened immune system, whether due to conditions like HIV/AIDS or immunosuppressive medications, can increase the risk of cervical cancer. The immune system plays a crucial role in fighting off infections, including HPV. Regular screenings and medical check-ups are vital for those with compromised immune systems.
Age and Family History
Cervical cancer is more common in women over the age of 30. Additionally, a family history of cervical cancer can increase an individual’s risk. It’s important for women with a family history to discuss their risk factors with a healthcare provider and consider more frequent screenings.
Cervical Cancer Diagnosis
Early detection of cervical cancer is crucial for effective treatment and improved survival rates. Understanding the diagnostic process can help women recognize the importance of regular screenings and consultations with healthcare professionals.
Pap Smear Test
The Pap smear test is a routine screening procedure that can detect precancerous changes in cervical cells. During this test, a healthcare provider collects cells from the cervix and examines them for abnormalities. Women should begin Pap smear testing at age 21 and continue every three years until age 29. From ages 30 to 65, women can opt for a Pap smear combined with HPV testing every five years.
HPV Testing
HPV testing is often performed alongside the Pap smear for women aged 30 and older. This test checks for the presence of high-risk HPV types that can lead to cervical cancer. If both tests are negative, the likelihood of developing cervical cancer in the near future is significantly reduced.
Colposcopy
If abnormal cells are detected during a Pap smear, a follow-up procedure called colposcopy may be recommended. This procedure involves using a special magnifying instrument to closely examine the cervix. If necessary, a biopsy may be performed to collect tissue samples for further analysis.
Biopsy
A biopsy is the definitive way to diagnose cervical cancer. During this procedure, a small sample of cervical tissue is removed and examined under a microscope. If cancer cells are present, further tests may be conducted to determine the stage of the cancer and the best course of treatment.
Imaging Tests
In some cases, imaging tests such as CT scans or MRIs may be used to assess the extent of the cancer and check for any spread to nearby tissues or organs. These tests help healthcare providers develop a comprehensive treatment plan tailored to the individual’s needs.
Understanding the risk factors and diagnostic procedures associated with cervical cancer is essential for early detection and effective treatment. Regular screenings and open communication with healthcare providers can significantly improve outcomes for women at risk.

Cervical Cancer Stages
Cervical cancer is a serious health concern that affects many women worldwide. Understanding the stages of cervical cancer is crucial for effective treatment and management. The stages indicate how far the cancer has spread and help guide treatment decisions. Here’s a breakdown of the stages of cervical cancer:
Stage 0: Carcinoma in Situ
In this earliest stage, abnormal cells are found in the lining of the cervix but have not invaded deeper tissues. This stage is often referred to as carcinoma in situ and is highly treatable. Regular screening, such as Pap smears, can help detect these changes early.
Stage I: Invasive Cancer
At this stage, the cancer has begun to invade deeper into the cervix. Stage I is further divided into:
- Stage IA: Microscopic invasion, where cancer cells are only visible under a microscope.
- Stage IB: Larger invasive cancer that can be seen without a microscope.
Stage II: Spread Beyond the Cervix
In Stage II, the cancer has spread beyond the cervix to the upper two-thirds of the vagina or the surrounding tissues. This stage is also divided into:
- Stage IIA: No involvement of the pelvic wall, but the cancer has spread to the upper two-thirds of the vagina.
- Stage IIB: Involvement of the surrounding tissues.
Stage III: Advanced Cancer
Stage III indicates that the cancer has spread to the lower third of the vagina or the pelvic wall. It may also involve nearby lymph nodes. This stage is categorized into:
- Stage IIIA: Cancer has spread to the lower third of the vagina.
- Stage IIIB: Cancer has spread to the pelvic wall and/or caused kidney problems.
Stage IV: Metastatic Cancer
Stage IV is the most advanced stage of cervical cancer, where the cancer has spread to distant organs, such as the lungs, liver, or bladder. This stage is divided into:
- Stage IVA: Spread to nearby organs.
- Stage IVB: Spread to distant organs.
Understanding these stages is vital for patients and healthcare providers to determine the most effective treatment options and improve outcomes. Regular screenings and awareness of cervical cancer symptoms can lead to early detection, which is key to successful treatment.
Cervical Cancer Treatment Options
When it comes to treating cervical cancer, the approach depends on the stage of the disease, the patient’s overall health, and personal preferences. Here are the primary treatment options available:
Surgery
Surgery is often the first line of treatment for early-stage cervical cancer. The type of surgery may include:
- Conization: A procedure to remove a cone-shaped piece of tissue from the cervix.
- Hysterectomy: Removal of the uterus and cervix, which may be total or radical depending on the extent of the cancer.
Radiation Therapy
Radiation therapy uses high-energy rays to kill cancer cells. It can be used alone or in combination with surgery. There are two types:
- External Beam Radiation: Delivers radiation from outside the body.
- Brachytherapy: Involves placing radioactive material inside the body near the cancer cells.
Chemotherapy
Chemotherapy uses drugs to kill cancer cells or stop their growth. It is often used in combination with radiation therapy for more advanced stages of cervical cancer. Common chemotherapy drugs include:
- Cisplatin
- Carboplatin
- Paclitaxel
Targeted Therapy
Targeted therapy focuses on specific characteristics of cancer cells. For cervical cancer, this may include drugs that target the human papillomavirus (HPV), which is a significant cause of cervical cancer. These therapies are still being researched but show promise in improving outcomes.
Immunotherapy
Immunotherapy helps the body’s immune system recognize and fight cancer cells. This treatment is becoming more common for various cancers, including cervical cancer, especially in advanced stages.
Each treatment option has its benefits and potential side effects, and the best approach is often a combination of therapies tailored to the individual patient. Consulting with a healthcare provider is essential to determine the most appropriate treatment plan based on the specific circumstances of the patient.

Cervical Cancer Prevention
Cervical cancer is a significant health concern for women worldwide, but the good news is that it is largely preventable. Understanding the risk factors and taking proactive measures can significantly reduce the chances of developing this disease. Here’s how you can protect yourself.
Understanding the Causes
The primary cause of cervical cancer is persistent infection with high-risk types of human papillomavirus (HPV). Other factors that may increase the risk include:
- Smoking: Tobacco use can weaken the immune system, making it harder for the body to fight off HPV infections.
- Long-term use of birth control pills: Women who use oral contraceptives for five or more years may have an increased risk.
- Multiple pregnancies: Having many children can increase the risk of cervical cancer.
- Weakened immune system: Conditions like HIV/AIDS or medications that suppress the immune system can elevate risk.
Regular Screening
One of the most effective ways to prevent cervical cancer is through regular screening. The Pap test and HPV test can detect precancerous changes in the cervix before they develop into cancer. Here’s what you need to know:
- Start screening: Women should begin cervical cancer screening at age 21.
- Frequency: Women aged 21-29 should have a Pap test every three years. From ages 30-65, women can choose to have a Pap test alone every three years, or a Pap test combined with an HPV test every five years.
- After 65: Women who have had regular screenings with normal results may not need to continue screening.
The Role of Vaccination
The cervical cancer vaccine, known as the HPV vaccine, is a crucial tool in prevention. It protects against the types of HPV that most commonly cause cervical cancer. Here are some key points:
- Who should get vaccinated? The vaccine is recommended for preteens aged 11 to 12, but it can be given as early as age 9 and up to age 26.
- Effectiveness: Studies show that the vaccine significantly reduces the risk of developing cervical cancer.
- Safety: The HPV vaccine has been extensively tested and is considered safe for use.
Healthy Lifestyle Choices
In addition to screening and vaccination, maintaining a healthy lifestyle can further reduce your risk of cervical cancer. Consider these tips:
- Quit smoking: Seek support to help you stop smoking, as it can significantly lower your risk.
- Healthy diet: A diet rich in fruits, vegetables, and whole grains can boost your immune system.
- Regular exercise: Aim for at least 150 minutes of moderate aerobic activity each week.
- Limit sexual partners: Reducing the number of sexual partners can lower your risk of HPV infection.
Cervical Cancer Support and Resources
Receiving a cervical cancer diagnosis can be overwhelming, but you are not alone. There are numerous resources and support systems available to help you navigate this journey.
Support Groups
Connecting with others who are experiencing similar challenges can provide emotional support and practical advice. Look for local or online support groups specifically for cervical cancer patients. These groups often offer:
- Emotional support: Share your feelings and experiences with others who understand.
- Information sharing: Learn about treatment options and coping strategies from fellow patients.
- Community events: Participate in awareness campaigns and fundraising events to support research.
Educational Resources
Knowledge is power when it comes to understanding cervical cancer. Here are some reputable organizations that provide valuable information:
- American Cancer Society: Offers comprehensive resources on cervical cancer, including treatment options and support services.
- Cancer Research UK: Provides detailed information about cervical cancer research and clinical trials.
- National Cervical Cancer Coalition: Focuses on education and awareness, offering resources for patients and families.
Healthcare Providers
Your healthcare team is your best ally in the fight against cervical cancer. Don’t hesitate to reach out to:
- Oncologists: Specialists in cancer treatment who can guide you through your options.
- Gynecologists: They can provide routine screenings and preventive care.
- Nutritionists: Professionals who can help you maintain a healthy diet during treatment.
Remember, early detection and a strong support system are key components in the fight against cervical cancer. Stay informed, stay proactive, and reach out for help when you need it. 💪❤️

Frequently Asked Questions about Cervical Cancer
What are the common symptoms of cervical cancer? 🤔
Cervical cancer may not present noticeable symptoms in its early stages. However, some common symptoms to watch for include:
- Unusual vaginal bleeding (between periods, after intercourse, or post-menopause)
- Pain during intercourse
- Pelvic pain that is persistent
- Unusual vaginal discharge that may be watery or have a foul odor
How can cervical cancer be prevented? 💉
Preventing cervical cancer primarily involves vaccination and regular screenings. Key preventive measures include:
- Cervical cancer vaccine (HPV vaccine) to protect against the human papillomavirus
- Regular Pap smears and HPV tests to detect any abnormalities early
- Practicing safe sex to reduce the risk of HPV infection
What are the causes of cervical cancer? 🦠
The primary cause of cervical cancer is persistent infection with high-risk types of human papillomavirus (HPV). Other contributing factors may include:
- Smoking
- Weakened immune system
- Long-term use of birth control pills
- Multiple full-term pregnancies
What is the survival rate for cervical cancer? 📊
The survival rate for cervical cancer varies based on the stage at which it is diagnosed. Generally, the earlier the detection, the better the prognosis. The 5-year survival rate for localized cervical cancer is approximately 92%, while it decreases for more advanced stages.
What treatments are available for cervical cancer? 💊
Treatment options for cervical cancer depend on the stage of the disease and may include:
- Surgery (to remove cancerous tissue)
- Radiation therapy
- Chemotherapy
- Targeted therapy for advanced cases
How often should I get screened for cervical cancer? 📅
It is recommended that women begin cervical cancer screening at age 21. The frequency of screenings may vary based on age and health history:
- Age 21-29: Pap test every 3 years
- Age 30-65: Pap test plus HPV test every 5 years or Pap test alone every 3 years
- Over 65: Screening may be discontinued if there is a history of normal results
Where can I get the cervical cancer vaccine? 🌍
The cervical cancer vaccine is available at various healthcare providers, clinics, and pharmacies. In Germany, it is often provided through public health programs. Consult your healthcare provider for more information on availability and eligibility.




