Understanding Emergencies
Emergencies can strike at any moment, often without warning. Whether it’s a medical crisis, a natural disaster, or an accident, knowing how to respond can make a significant difference in the outcome. Understanding the nature of emergencies is crucial for everyone, as it equips you with the knowledge and skills to act swiftly and effectively.
Types of Emergencies
Emergencies can be categorized into several types, each requiring a different response:
- Medical Emergencies: These include situations like heart attacks, strokes, severe allergic reactions, and respiratory distress. Quick action can save lives.
- Natural Disasters: Events such as earthquakes, floods, and hurricanes can lead to widespread chaos. Being prepared can help you and your loved ones stay safe.
- Accidents: Car crashes, falls, and workplace incidents are common emergencies that require immediate attention.
- Fire Emergencies: Fires can spread rapidly, making it essential to know how to evacuate safely and use fire extinguishers.
Why Understanding Emergencies Matters
Being informed about emergencies not only helps you respond effectively but also empowers you to assist others. In many cases, bystanders can play a critical role in emergency situations. For instance, knowing how to perform CPR or rescue breathing can be the difference between life and death. Additionally, understanding the importance of automated external defibrillators (AEDs) and how to access them can significantly improve survival rates in cardiac emergencies.
Moreover, newly-elected Texas State Senator Molly Cook, an emergency room nurse, has introduced legislation aimed at improving access to AEDs and enhancing CPR training across Texas. This initiative highlights the growing recognition of the importance of emergency preparedness in our communities.
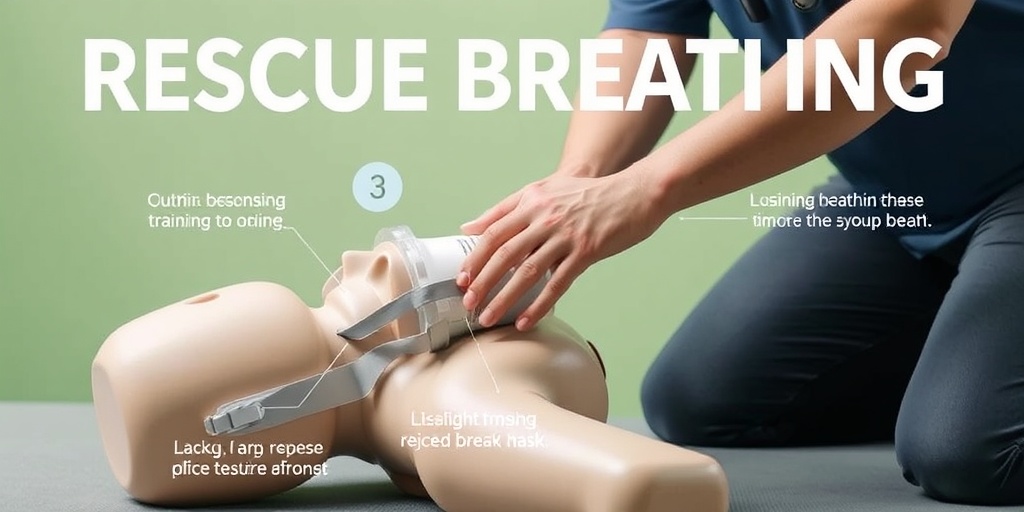
What Is Rescue Breathing?
Rescue breathing is a critical skill that can help save lives in emergencies, particularly when someone is not breathing or is breathing inadequately. It involves providing breaths to a person who is unable to breathe on their own, ensuring that oxygen reaches their lungs and vital organs.
When Is Rescue Breathing Necessary?
Rescue breathing is typically required in situations where:
- A person is unresponsive and not breathing.
- A person is experiencing severe respiratory distress.
- Cardiac arrest occurs, and CPR is being performed.
How to Perform Rescue Breathing
Performing rescue breathing can be daunting, but following these steps can help you do it effectively:
- Check Responsiveness: Tap the person and shout to see if they respond.
- Call for Help: If there’s no response, call emergency services immediately.
- Open the Airway: Tilt the head back slightly and lift the chin to open the airway.
- Check for Breathing: Look, listen, and feel for breathing for no more than 10 seconds.
- Give Breaths: Pinch the nose shut, cover the person’s mouth with yours, and give two breaths, each lasting about one second. Watch for the chest to rise.
- Continue CPR: If the person does not start breathing, continue with chest compressions and rescue breaths in a cycle.
It’s essential to remember that rescue breathing should be performed in conjunction with chest compressions as part of CPR. The combination of these techniques maximizes the chances of survival until professional help arrives.
Training and Resources
To effectively perform rescue breathing and CPR, proper training is vital. Many organizations offer courses that teach these life-saving skills. Consider enrolling in a CPR and first aid class to gain hands-on experience. Resources like Yesil Health AI (yesilhealth.com) can provide valuable information and guidance on emergency response techniques.
In conclusion, understanding emergencies and knowing how to perform rescue breathing are essential skills that everyone should possess. By being prepared and informed, you can make a significant impact in critical situations, potentially saving lives and helping those in need. Remember, in emergencies, every second counts! ⏳
When to Use CPR
Cardiopulmonary resuscitation (CPR) is a lifesaving technique that can be crucial in emergencies where someone’s breathing or heartbeat has stopped. Understanding when to use CPR can make the difference between life and death. Here are some key situations where CPR is necessary:
Recognizing Cardiac Arrest
Cardiac arrest occurs when the heart suddenly stops beating effectively. This can happen due to various reasons, including heart disease, trauma, or drowning. Here are the signs that indicate someone may need CPR:
- Unresponsiveness: The person does not respond when you shake them or shout.
- No Breathing: The individual is not breathing or is only gasping.
- No Pulse: You cannot feel a pulse in the neck or wrist.
If you observe any of these signs, it’s crucial to act quickly. Call emergency services immediately and begin CPR.
Situations Requiring CPR
CPR should be performed in various emergency situations, including:
- Heart Attack: If someone is experiencing chest pain, shortness of breath, or discomfort in the arms, back, neck, or jaw, they may be having a heart attack.
- Drowning: If a person has been submerged in water and is unresponsive, CPR can help restore breathing.
- Choking: If someone is choking and becomes unresponsive, CPR can help expel the blockage.
- Severe Trauma: Injuries from accidents can lead to cardiac arrest, necessitating immediate CPR.
In any of these scenarios, acting swiftly can save a life. Remember, even if you are unsure, it is better to perform CPR than to do nothing at all! 🚑
CPR Techniques Explained
Knowing how to perform CPR correctly is essential for effective emergency response. Here’s a breakdown of the CPR techniques you should be familiar with:
The Basics of CPR
CPR consists of two main components: chest compressions and rescue breaths. Here’s how to perform each step:
1. Chest Compressions
Chest compressions are vital for maintaining blood flow to the brain and other organs. Follow these steps:
- Positioning: Place the heel of one hand on the center of the person’s chest, then place your other hand on top of the first hand.
- Compression Depth: Push down hard and fast, aiming for a depth of about 2 inches (5 cm) and a rate of 100 to 120 compressions per minute.
- Allow Full Recoil: Let the chest rise completely between compressions to allow the heart to refill with blood.
2. Rescue Breaths
Rescue breaths are used to provide oxygen to the lungs. Here’s how to do it:
- Open the Airway: Tilt the person’s head back slightly and lift the chin to open the airway.
- Pinch the Nose: Pinch the person’s nose shut and cover their mouth with yours, creating a seal.
- Give Breaths: Deliver two breaths, each lasting about 1 second, and watch for the chest to rise.
After giving two rescue breaths, continue with chest compressions. The cycle should be 30 compressions followed by 2 breaths. Repeat this until emergency services arrive or the person shows signs of life. 💓
Hands-Only CPR
If you are untrained or uncomfortable giving rescue breaths, you can perform hands-only CPR. This method focuses solely on chest compressions:
- Call for Help: Ensure someone has called emergency services.
- Compressions Only: Perform continuous chest compressions at the same rate (100 to 120 per minute) until help arrives.
Hands-only CPR is effective and can be performed by anyone, making it a valuable skill to have in emergencies.
Training and Certification
While knowing the basics of CPR is essential, formal training can enhance your skills and confidence. Consider enrolling in a CPR and first aid course offered by organizations like the American Heart Association or the Red Cross. These courses provide hands-on practice and certification, ensuring you are prepared for real-life emergencies. 🏥
In conclusion, understanding when to use CPR and how to perform it effectively can save lives. Whether you are a bystander or a trained professional, your actions in an emergency can make a significant difference. Stay informed, stay prepared, and be ready to act when it matters most!

Signs of Cardiac Arrest
Cardiac arrest is a critical medical emergency that can happen suddenly and without warning. Recognizing the signs of cardiac arrest is crucial, as immediate action can save a life. Here are the key indicators to look out for:
1. Sudden Collapse
One of the most alarming signs of cardiac arrest is a sudden collapse. If someone falls to the ground and is unresponsive, it’s essential to act quickly. This collapse can occur during physical activity or even while at rest.
2. Unresponsiveness
If the person does not respond when you shake them or shout their name, this is a significant indicator of cardiac arrest. Check for responsiveness by gently tapping their shoulder and calling out to them.
3. No Breathing or Abnormal Breathing
In cases of cardiac arrest, the individual may stop breathing entirely or exhibit gasping or irregular breathing patterns. This abnormal breathing is often referred to as agonal breathing and requires immediate intervention.
4. Pale or Bluish Skin
Look for changes in skin color. A person experiencing cardiac arrest may appear pale or have a bluish tint, especially around the lips and fingertips. This discoloration indicates a lack of oxygen in the blood.
5. Weak or No Pulse
In a cardiac arrest situation, the heart is not effectively pumping blood. If you can’t feel a pulse in the neck (carotid artery) or wrist (radial artery), this is a critical sign that immediate action is needed.
Recognizing these signs can make a significant difference in the outcome of a cardiac arrest situation. If you suspect someone is experiencing cardiac arrest, call emergency services immediately and prepare to perform CPR.
Rescue Breathing Steps
Rescue breathing is a vital component of CPR (Cardiopulmonary Resuscitation) that can help provide oxygen to someone who is not breathing. Here’s a step-by-step guide on how to perform rescue breathing effectively:
1. Ensure Safety
Before approaching the individual, ensure the environment is safe for both you and the victim. Look for any potential hazards that could pose a risk.
2. Check Responsiveness
Gently tap the person and shout, “Are you okay?” If there is no response, proceed to check for breathing.
3. Call for Help
If the person is unresponsive and not breathing, call emergency services immediately or ask someone else to do so. Time is of the essence in emergencies!
4. Position the Head
To open the airway, tilt the person’s head back slightly by placing one hand on their forehead and using your other hand to lift their chin. This maneuver helps to clear the airway.
5. Check for Breathing
Look, listen, and feel for breathing for no more than 10 seconds. If the person is not breathing or only gasping, you need to begin rescue breathing.
6. Deliver Rescue Breaths
- Seal the lips: Pinch the person’s nose shut and cover their mouth with yours to create a seal.
- Give breaths: Deliver two breaths, each lasting about one second. Watch for the chest to rise as you breathe into the person.
- Repeat if necessary: After giving two breaths, check for a pulse and continue with CPR if there is no pulse.
7. Continue CPR
If the person remains unresponsive and without a pulse, continue with chest compressions at a rate of 100-120 compressions per minute, alternating with rescue breaths (30 compressions followed by 2 breaths) until emergency help arrives.
Performing rescue breathing can be daunting, but knowing the steps can empower you to act confidently in an emergency. Remember, every second counts when it comes to saving a life! 🕒❤️

CPR for Children and Infants
When it comes to emergencies, knowing how to perform CPR (Cardiopulmonary Resuscitation) on children and infants can be a lifesaver. The techniques differ significantly from those used on adults, making it crucial for caregivers, parents, and anyone who works with children to be well-informed. Let’s explore the essential steps and considerations for performing CPR on younger patients.
Understanding the Differences
CPR for children and infants is not just a scaled-down version of adult CPR. The anatomy and physiology of children differ, which necessitates specific techniques:
- Compression Depth: For infants, compressions should be about 1.5 inches deep, while for children, aim for about 2 inches.
- Compression Rate: The recommended rate is 100 to 120 compressions per minute for both age groups.
- Breath-to-Compression Ratio: In a two-rescuer scenario, the ratio is 15:2 for children and infants, while it’s 30:2 for adults.
Steps for Performing CPR on Infants
Here’s a step-by-step guide to performing CPR on infants (under 1 year old):
- Check Responsiveness: Gently tap the infant and shout to see if they respond.
- Call for Help: If there’s no response, call emergency services immediately or ask someone else to do so.
- Open the Airway: Place the infant on their back and tilt their head slightly back to open the airway.
- Check for Breathing: Look, listen, and feel for breathing for no more than 10 seconds.
- Begin Compressions: Use two fingers to compress the chest at the center, allowing full recoil between compressions.
- Give Rescue Breaths: After 30 compressions, give 2 gentle breaths, ensuring the chest rises.
Steps for Performing CPR on Children
For children (ages 1 to puberty), follow these steps:
- Check Responsiveness: Tap the child and shout to see if they respond.
- Call for Help: If unresponsive, call emergency services or have someone else do it.
- Open the Airway: Tilt the head back slightly to open the airway.
- Check for Breathing: Look, listen, and feel for breathing for no more than 10 seconds.
- Begin Compressions: Use one or two hands (depending on the size of the child) to compress the chest.
- Give Rescue Breaths: After 30 compressions, provide 2 rescue breaths.
When to Stop CPR
It’s essential to know when to stop CPR:
- If emergency medical services arrive and take over.
- If the child shows signs of life, such as breathing or movement.
- If you are too exhausted to continue.
Post-CPR Care and Recovery
After performing CPR, the focus shifts to post-CPR care and recovery. This phase is just as critical as the CPR itself, as it can significantly impact the patient’s outcome.
Immediate Medical Attention
Regardless of the outcome of CPR, the individual must receive immediate medical attention. Emergency responders will assess the patient’s condition and provide necessary interventions. Here’s what to expect:
- Monitoring Vital Signs: Medical professionals will monitor heart rate, blood pressure, and oxygen levels.
- Advanced Care: Depending on the situation, advanced life support may be initiated.
- Transport to Hospital: The patient will likely be transported to a hospital for further evaluation and treatment.
Emotional Support
Experiencing or witnessing a cardiac emergency can be traumatic. Providing emotional support to the patient and their family is vital:
- Reassurance: Offer comfort and reassurance to the family members.
- Professional Help: Encourage seeking professional counseling if needed.
Long-Term Recovery
Recovery from a cardiac event can vary significantly based on the individual’s health and the circumstances surrounding the incident. Here are some key points to consider:
- Rehabilitation: Cardiac rehabilitation programs may be recommended to help the patient regain strength and learn about heart health.
- Follow-Up Care: Regular follow-up appointments with healthcare providers are essential for monitoring recovery.
- Support Groups: Joining support groups can provide emotional and psychological support during recovery.
Understanding the importance of CPR for children and infants, along with the necessary post-CPR care, can empower individuals to act confidently in emergencies. Remember, every second counts! ⏳

Frequently Asked Questions about Emergencies, Rescue Breathing and CPR
What is the difference between rescue breathing and CPR?
Rescue breathing is a technique used to provide oxygen to someone who is not breathing, while CPR (Cardiopulmonary Resuscitation) combines chest compressions with rescue breaths to maintain blood flow and oxygenation in a person whose heart has stopped beating.
When should I perform CPR?
You should perform CPR if you encounter someone who is unresponsive and not breathing or only gasping. It is crucial to act quickly, as every second counts in emergencies.
How do I know if someone needs rescue breathing?
If a person is unresponsive and not breathing normally, you should check for signs of life. If they are not breathing or only gasping, you should initiate rescue breathing immediately.
What are the steps for performing CPR?
- Check the scene for safety.
- Call for emergency help or ask someone else to do so.
- Check the person’s responsiveness and breathing.
- If unresponsive and not breathing, begin chest compressions.
- After 30 compressions, give 2 rescue breaths.
- Continue the cycle until help arrives or the person shows signs of life.
Can I perform CPR on a child or infant?
Yes, you can perform CPR on children and infants, but the technique differs slightly. For infants, use two fingers for compressions and give gentle rescue breaths. For children, use one hand for compressions and ensure the breaths are appropriate for their size.
What should I do if I feel scared or unsure during an emergency?
It’s normal to feel scared or unsure in an emergency. Remember that taking action, even if imperfect, is better than doing nothing. If you’re uncertain, focus on calling for help and following the dispatcher’s instructions.
How can I prepare for emergencies?
- Take a certified CPR and first aid course.
- Keep a first aid kit accessible.
- Familiarize yourself with emergency numbers and procedures.
- Practice emergency scenarios with family or friends.
Where can I find CPR training classes?
You can find CPR training classes through local hospitals, community centers, or organizations like the American Red Cross. Many places also offer online courses for convenience.
What should I do if CPR fails?
If CPR fails and the person does not respond, continue until emergency services arrive. It’s important to remain calm and provide as much information as possible to the responders.
Is it legal to perform CPR on someone?
In most places, Good Samaritan laws protect individuals who provide assistance in emergencies, including performing CPR. However, it’s always best to check local laws for specific regulations.
How can I help my community with emergency preparedness?
- Organize or participate in local CPR training sessions.
- Share information about emergency procedures on social media.
- Encourage local businesses to have AEDs and trained staff.
By understanding emergencies, rescue breathing, and CPR, you can be better prepared to help in critical situations. Stay informed and ready to act! 🚑




