What Is Tularemia?
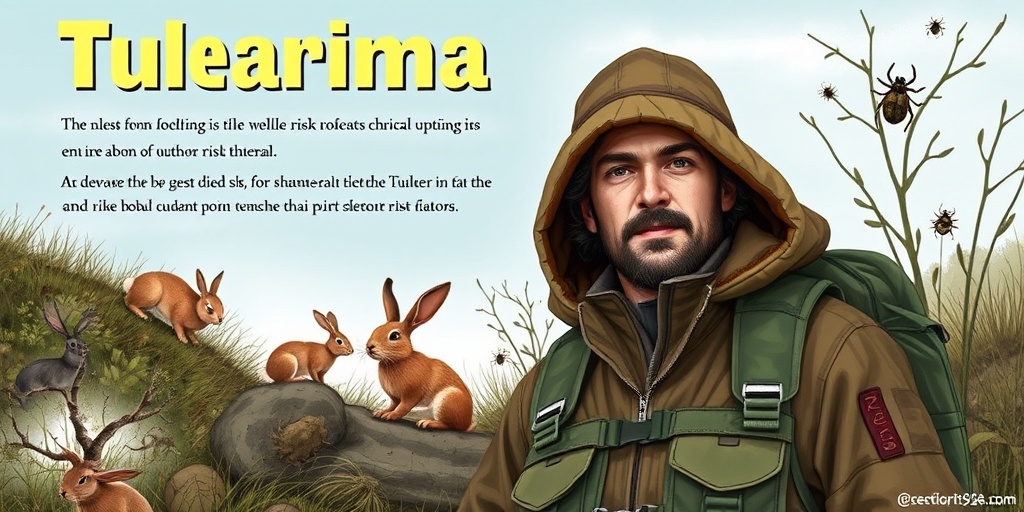
Tularemia, often referred to as “rabbit fever,” is a highly infectious disease caused by the bacterium Francisella tularensis. This zoonotic disease primarily affects animals, particularly rodents and lagomorphs like rabbits, but it can also infect humans. Tularemia is considered a potential bioterrorism agent due to its virulence and ability to be transmitted through various routes.
The bacterium is typically found in the wild, especially in areas where animals are abundant. Humans can contract tularemia through several means, including:
- Direct contact: Handling infected animals or their tissues.
- Inhalation: Breathing in contaminated aerosols.
- Ingestion: Consuming contaminated food or water.
- Insect bites: Tick and deer fly bites can also transmit the disease.
Understanding tularemia is crucial, especially for those who work closely with animals or spend time in rural areas. The disease can manifest in various forms, depending on the route of infection, making awareness and early detection vital.
Tularemia Symptoms
The symptoms of tularemia can vary significantly based on how the infection occurs. Generally, symptoms appear within 3 to 5 days after exposure, but they can take up to two weeks to manifest. Here are some common symptoms associated with different forms of tularemia:
Ulceroglandular Tularemia
This is the most common form of tularemia, typically resulting from direct contact with infected animals. Symptoms may include:
- Skin ulcer: A painful sore at the site of infection.
- Swollen lymph nodes: Often near the ulcer, these can become painful and tender.
- Fever and chills: Common systemic symptoms that may accompany the infection.
Pneumonic Tularemia
When tularemia is contracted through inhalation, it can lead to pneumonia. Symptoms include:
- Cough: A persistent cough that may produce phlegm.
- Chest pain: Discomfort or pain in the chest area.
- Difficulty breathing: Shortness of breath may occur as the infection progresses.
Oculoglandular Tularemia
This form occurs when the bacteria infect the eye, often through contact with infected animals or contaminated materials. Symptoms include:
- Eye redness: Inflammation and redness of the eye.
- Pain and swelling: Discomfort and swelling around the eye area.
- Discharge: Possible discharge from the eye.
Other Symptoms
Regardless of the form, tularemia can also cause:
- Headaches: Often severe and persistent.
- Fatigue: A general feeling of tiredness and weakness.
- Muscle aches: Generalized body aches and discomfort.
If you suspect you have been exposed to tularemia or are experiencing these symptoms, it is crucial to seek medical attention promptly. Early diagnosis and treatment can significantly improve outcomes and reduce the risk of complications.
For more information on tularemia and other health-related topics, consider visiting Yesil Health AI, a valuable resource for evidence-based health answers. Stay informed and protect yourself from this infectious disease! 🌍💉

Tularemia Transmission
Tularemia, often referred to as “rabbit fever,” is a highly infectious disease caused by the bacterium Francisella tularensis. Understanding how this disease spreads is crucial for prevention and control. Let’s delve into the various ways tularemia can be transmitted to humans.
Direct Contact with Infected Animals
One of the primary modes of transmission is through direct contact with infected animals. This is particularly common among hunters and those who handle wildlife. The bacterium can enter the body through cuts or abrasions on the skin. Common animals that can carry tularemia include:
- Rabbits 🐇
- Rodents
- Beavers
- Muskrats
- Ticks and fleas
When handling these animals, it’s essential to wear gloves and practice good hygiene to minimize the risk of infection.
Inhalation of Contaminated Aerosols
Another significant route of transmission is through inhalation. When infected animals are present, especially during activities like skinning or butchering, tiny droplets containing the bacteria can become airborne. This can lead to respiratory tularemia, which is more severe and can cause pneumonia. 🦠
Ingestion of Contaminated Water or Food
Consuming contaminated food or water is another way tularemia can be transmitted. This is particularly a concern in areas where the bacterium is prevalent in wildlife. Drinking untreated water from lakes or streams where infected animals may have been present can pose a risk. Always ensure that water is properly treated before consumption.
Vector-Borne Transmission
Ticks and deer flies are known vectors for tularemia. When these insects bite an infected animal and then bite a human, they can transmit the bacteria. This is particularly concerning in rural areas where these vectors are common. Taking precautions against insect bites, such as using insect repellent and wearing protective clothing, can help reduce the risk of transmission.
Tularemia Risk Factors
Understanding the risk factors associated with tularemia can help individuals take proactive measures to protect themselves. Here are some key factors to consider:
Occupational Hazards
Individuals who work in certain professions are at a higher risk of contracting tularemia. This includes:
- Wildlife biologists
- Veterinarians
- Laboratory personnel
- Farmers and ranchers
These professionals often come into contact with infected animals or their environments, increasing their likelihood of exposure.
Geographic Location
Tularemia is more prevalent in certain regions, particularly in the United States. Areas with high populations of wild rabbits and rodents, such as parts of the Midwest and South, see more cases. If you live or work in these areas, it’s essential to be aware of the risks and take appropriate precautions.
Seasonal Factors
The incidence of tularemia tends to increase during warmer months when people are more likely to engage in outdoor activities, such as hunting and camping. During these times, the risk of encountering infected animals or their vectors is heightened. 🌞
Personal Health Conditions
Individuals with compromised immune systems or underlying health conditions may be at a greater risk for severe tularemia. If you have a weakened immune system, it’s crucial to take extra precautions when in areas where tularemia is known to occur.
Preventive Measures
To mitigate the risk of tularemia, consider the following preventive measures:
- Avoid handling wild animals unless necessary.
- Wear gloves when handling animal carcasses.
- Use insect repellent to prevent bites from ticks and deer flies.
- Ensure food and water are safe for consumption.
By understanding the transmission routes and risk factors associated with tularemia, individuals can better protect themselves and their communities from this potentially serious disease. Stay informed and take the necessary precautions to enjoy the outdoors safely! 🌲
Tularemia Diagnosis
Tularemia, often referred to as “rabbit fever,” is a highly infectious disease caused by the bacterium Francisella tularensis. This zoonotic disease can affect both humans and animals, particularly rabbits and rodents. Diagnosing tularemia can be challenging due to its varied symptoms and the fact that it can mimic other illnesses. Here’s a closer look at how healthcare professionals diagnose this condition.
Recognizing Symptoms
The first step in diagnosing tularemia is recognizing its symptoms, which can vary depending on the route of infection. Common symptoms include:
- Fever: Often one of the first signs, it can be high and persistent.
- Chills: Accompanied by fever, chills can make patients feel extremely uncomfortable.
- Headache: A common complaint that can range from mild to severe.
- Fatigue: General malaise and weakness are prevalent.
- Swollen Lymph Nodes: Particularly in the groin or armpit, depending on the infection site.
- Skin Ulcers: These may develop at the site of infection, especially if contracted through a cut or abrasion.
In some cases, tularemia can also cause respiratory symptoms, gastrointestinal issues, or even ocular problems if the bacteria enter through the eyes. Given this wide range of symptoms, it’s crucial for healthcare providers to consider tularemia in patients with unexplained febrile illnesses, especially those with a history of exposure to potentially infected animals.
Laboratory Testing
Once tularemia is suspected based on symptoms and exposure history, laboratory tests are essential for confirmation. Common diagnostic methods include:
- Serology Tests: These tests detect antibodies against Francisella tularensis in the blood. A significant rise in antibody levels between acute and convalescent phases can confirm the diagnosis.
- Culture Tests: Although not commonly performed due to the bacterium’s infectious nature, culturing the bacteria from blood, lymph nodes, or other infected tissues can provide a definitive diagnosis.
- Polymerase Chain Reaction (PCR): This molecular technique can detect the genetic material of the bacteria in various samples, offering a rapid and accurate diagnosis.
It’s important to note that early diagnosis is crucial for effective treatment, as tularemia can lead to severe complications if left untreated. If you suspect you have been exposed to tularemia or are experiencing symptoms, seek medical attention promptly. 🩺
Tularemia Treatment Options
Once diagnosed, the treatment of tularemia primarily involves the use of antibiotics. The choice of antibiotic and duration of treatment can vary based on the severity of the disease and the specific symptoms presented. Here’s a breakdown of the most common treatment options available for tularemia.
Antibiotic Therapy
The first line of treatment for tularemia typically includes:
- Streptomycin: This is often the preferred antibiotic for severe cases of tularemia. It is administered via injection and is effective in treating systemic infections.
- Gentamicin: Another aminoglycoside antibiotic, gentamicin is used similarly to streptomycin, especially in patients who may not tolerate the latter.
- Doxycycline: For mild to moderate cases, doxycycline can be an effective oral alternative. It is particularly useful for patients who may not require hospitalization.
- Ciprofloxacin: This fluoroquinolone antibiotic can also be used, especially in cases where patients are allergic to other antibiotics.
Most patients respond well to antibiotic treatment, and symptoms typically improve within a few days. However, it’s essential to complete the full course of antibiotics as prescribed to prevent relapse or complications.
Supportive Care
In addition to antibiotic therapy, supportive care is crucial for recovery. This may include:
- Hydration: Ensuring adequate fluid intake helps combat fever and supports overall recovery.
- Pain Management: Over-the-counter pain relievers can help alleviate headaches and body aches.
- Rest: Adequate rest is vital for the body to heal and recover from the infection.
In severe cases, hospitalization may be required for intravenous antibiotics and close monitoring. It’s important to follow up with your healthcare provider to ensure that the infection is fully resolved and to discuss any potential long-term effects. 🌟

Tularemia Prevention
Tularemia, often referred to as “rabbit fever,” is a highly infectious disease caused by the bacterium Francisella tularensis. It can affect both humans and animals, particularly rabbits and rodents. Understanding how to prevent tularemia is crucial, especially for those who work or spend time in environments where exposure is possible. Here are some effective strategies for preventing this disease.
Understanding the Risks
Before diving into prevention methods, it’s essential to understand how tularemia is transmitted. The bacterium can enter the body through:
- Direct contact with infected animals, especially through cuts or abrasions.
- Inhalation of contaminated aerosols or dust.
- Ingestion of contaminated food or water.
- Bite from infected insects, such as ticks and deer flies.
Preventive Measures
Here are some practical steps you can take to reduce your risk of contracting tularemia:
- Avoid contact with wild animals, particularly rabbits and rodents. If you must handle them, wear gloves and wash your hands thoroughly afterward.
- Use insect repellent to protect against bites from ticks and deer flies, especially in areas where tularemia is known to occur.
- Cook meat thoroughly before consumption. This is particularly important for wild game, which may carry the bacteria.
- Practice safe handling of animal carcasses. If you hunt or trap animals, ensure you wear gloves and avoid touching your face.
- Stay informed about tularemia outbreaks in your area. Local health departments often provide updates on disease prevalence.
Protecting Pets and Livestock
Pets and livestock can also be at risk for tularemia. Here’s how to keep them safe:
- Keep pets indoors or supervise them when outside, especially in areas where wild animals are present.
- Vaccinate pets if recommended by a veterinarian, particularly in regions where tularemia is common.
- Regularly check for ticks and fleas on pets and use appropriate preventive treatments.
Tularemia Outlook
The outlook for tularemia largely depends on early detection and treatment. While the disease can be severe, it is generally treatable with antibiotics if caught early. Here’s what you need to know about the prognosis and ongoing concerns regarding tularemia.
Prognosis and Treatment
When diagnosed promptly, the prognosis for tularemia is quite favorable. Treatment typically involves:
- Antibiotics: Medications such as streptomycin, gentamicin, or doxycycline are commonly prescribed.
- Supportive care: This may include hydration and pain management, depending on the severity of symptoms.
Most patients respond well to treatment, and symptoms usually resolve within a few weeks. However, some individuals may experience lingering effects, such as fatigue or muscle pain, for an extended period.
Current Trends and Concerns
Recent data from the CDC indicates a concerning rise in tularemia cases in the United States. Factors contributing to this increase include:
- Climate change: Altered weather patterns can expand the habitats of both the bacteria and its animal hosts.
- Increased human-wildlife interaction: As urban areas expand into wildlife habitats, the risk of exposure rises.
- Awareness and reporting: Improved surveillance and reporting may also contribute to the perceived increase in cases.
Public health officials continue to monitor these trends closely, emphasizing the importance of awareness and prevention strategies to mitigate the spread of tularemia.
Conclusion
While tularemia can pose serious health risks, understanding how to prevent it and recognizing the signs and symptoms can significantly improve outcomes. By taking proactive measures, individuals can protect themselves and their communities from this infectious disease. 🌍💪

Frequently Asked Questions about Tularemia
What is Tularemia?
Tularemia is an infectious disease caused by the bacterium Francisella tularensis. It primarily affects animals, especially rodents and rabbits, but can also infect humans. The disease is often referred to as “rabbit fever” due to its association with these animals.
What are the symptoms of Tularemia in humans?
Symptoms of tularemia can vary depending on the route of infection but may include:
- Fever and chills
- Fatigue
- Headache
- Muscle aches
- Swollen lymph nodes
- Skin ulcers
- Respiratory issues
If you suspect you have tularemia, it is important to seek medical attention promptly.
How is Tularemia transmitted?
Tularemia can be transmitted through various routes, including:
- Direct contact with infected animals or their tissues
- Inhalation of contaminated aerosols
- Ingestion of contaminated food or water
- Bite from infected insects, such as ticks or deer flies
Can Tularemia be treated?
Yes, tularemia can be treated effectively with antibiotics. Early diagnosis and treatment are crucial for a successful recovery. Common antibiotics used include:
- Streptomycin
- Gentamicin
- Doxycycline
Always consult a healthcare professional for appropriate treatment options.
Is Tularemia common in pets, like dogs and rabbits?
Tularemia can affect various animals, including dogs and rabbits. While it is more commonly seen in wild rabbits, domestic pets can also contract the disease. If you notice any unusual symptoms in your pets, such as lethargy or fever, consult a veterinarian.
How can I prevent Tularemia?
To reduce the risk of tularemia, consider the following preventive measures:
- Avoid contact with wild animals, especially rabbits and rodents.
- Wear gloves when handling animals or cleaning up after them.
- Use insect repellent to prevent bites from ticks and deer flies.
- Practice good hygiene, such as washing hands thoroughly after handling animals.
What should I do if I suspect I have Tularemia?
If you believe you have been exposed to tularemia or are experiencing symptoms, it is essential to seek medical attention immediately. Early diagnosis and treatment can significantly improve outcomes.
Where can I find more information about Tularemia?
For more detailed information about tularemia, you can visit reputable health websites such as the Centers for Disease Control and Prevention (CDC) or consult with healthcare professionals.




