What Is Peripheral Vascular Disease?
Peripheral Vascular Disease, commonly referred to as PVD, is a circulatory condition that affects millions of people worldwide. But what exactly is it, and how does it impact our overall health?
Understanding PVD: A Brief Overview
PVD occurs when the blood vessels outside of the heart and brain, such as those in the legs, arms, and organs, become narrowed or blocked. This reduction in blood flow can lead to a range of symptoms, from mild discomfort to severe pain and even organ damage.
The primary cause of PVD is atherosclerosis, a condition where plaque builds up in the arteries, restricting blood flow. Other factors, such as high blood pressure, high cholesterol, smoking, and diabetes, can also contribute to the development of PVD.
The Impact of PVD on Daily Life
While PVD can affect anyone, it’s more common in people over 50, smokers, and those with a family history of the condition. If left untreated, PVD can significantly impact daily life, making everyday activities, such as walking or exercising, a challenge.
In severe cases, PVD can lead to amputation, heart attack, or stroke. However, with early detection and proper treatment, it’s possible to manage the condition and reduce the risk of complications.
PVD Symptoms and Warning Signs
Recognizing the symptoms of PVD is crucial for early detection and treatment. While some people may not experience any symptoms at all, others may notice:
Common Symptoms of PVD
- Leg pain or cramping when walking or exercising, which disappears when resting (intermittent claudication)
- Numbness or tingling in the legs, feet, or toes
- Coldness or discoloration of the legs or feet
- Weak or tired legs
- Ulcers or wounds that won’t heal
- Discoloration or gangrene in severe cases
If you’re experiencing any of these symptoms, it’s essential to consult with your healthcare provider. They may perform a physical examination, review your medical history, and conduct diagnostic tests, such as an ankle-brachial index (ABI) or ultrasound, to determine the severity of PVD.
Remember, early detection and treatment can significantly improve outcomes for those with PVD. If you’re concerned about your symptoms or have questions about PVD, consider consulting with a healthcare professional or exploring evidence-based resources like Yesil Health AI (yesilhealth.com) for reliable information and guidance. 💊

Causes and Risk Factors of Peripheral Vascular Disease
Peripheral Vascular Disease (PVD) is a condition that affects the blood vessels outside of the heart, reducing blood flow to the limbs. While it’s often associated with leg pain, PVD can cause a range of symptoms, from numbness and tingling to weakness and cramping. But what causes this condition, and who’s at risk?
Atherosclerosis: The Primary Cause of PVD
The main culprit behind PVD is atherosclerosis, a buildup of plaque in the arteries. This plaque, made up of fat, cholesterol, and other substances, narrows the arteries, reducing blood flow to the limbs. Over time, the plaque can harden and block the arteries, leading to PVD.
Risk Factors for PVD
While atherosclerosis is the primary cause of PVD, certain risk factors can increase your likelihood of developing the condition. These include:
- Age: PVD risk increases with age, especially after 50.
- Smoking: Smoking damages the blood vessels and increases the risk of PVD.
- High Blood Pressure: Uncontrolled high blood pressure can damage the blood vessels, leading to PVD.
- High Cholesterol: High levels of low-density lipoprotein (LDL) cholesterol can contribute to atherosclerosis and PVD.
- Diabetes: People with diabetes are at higher risk of developing PVD due to high blood sugar levels damaging the blood vessels.
- Obesity: Being overweight or obese can increase the risk of PVD, as excess weight puts additional strain on the blood vessels.
- Physical Inactivity: A sedentary lifestyle can contribute to PVD, as regular physical activity helps maintain healthy blood flow.
- Family History: Having a family history of PVD or other cardiovascular conditions can increase your risk.
By understanding the causes and risk factors of PVD, you can take steps to reduce your risk and maintain healthy blood vessels. 💡
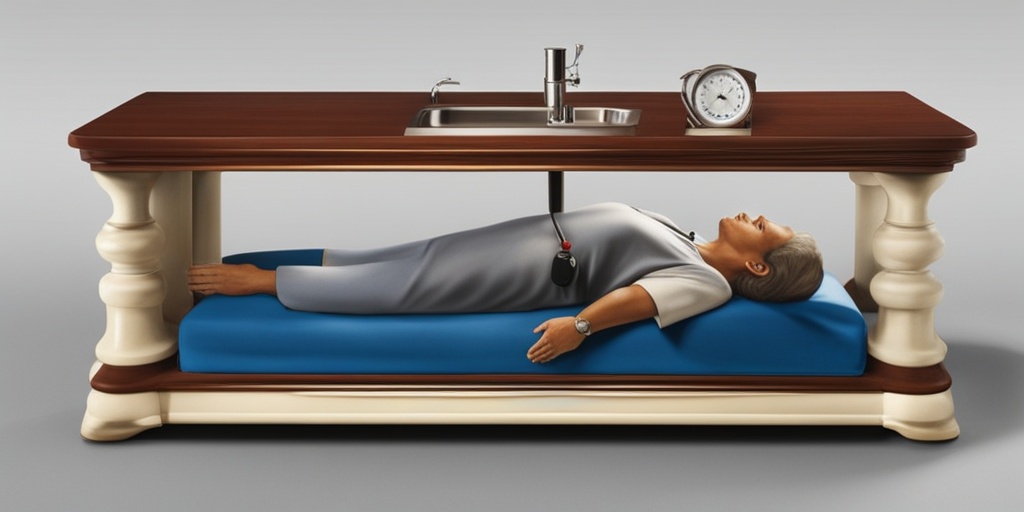
Diagnosing Peripheral Vascular Disease
Diagnosing PVD typically involves a combination of physical exams, medical history, and diagnostic tests. If you’re experiencing symptoms of PVD, your doctor will likely start with a physical exam to check for signs of poor circulation, such as:
- Pale or blue-tinged skin: Reduced blood flow can cause skin to appear pale or blue-tinged.
- Weak or absent pulses: Your doctor may check for pulses in your legs and feet to determine if blood flow is reduced.
- Cool skin temperature: Skin that’s cooler than normal can indicate reduced blood flow.
Next, your doctor will likely ask about your medical history, including any previous cardiovascular conditions, smoking habits, and family history of PVD.
Diagnostic Tests for PVD
To confirm a diagnosis of PVD, your doctor may order one or more of the following diagnostic tests:
- Ankle-Brachial Index (ABI) Test: This test compares blood pressure in your ankles to blood pressure in your arms to determine if there’s a blockage in the leg arteries.
- Doppler Ultrasound: This non-invasive test uses sound waves to measure blood flow in the arteries and detect any blockages.
- Duplex Ultrasound: This test combines Doppler ultrasound with traditional ultrasound to provide detailed images of the blood vessels and detect any blockages.
- Angiography: This test uses X-rays and dye to visualize the blood vessels and detect any blockages or narrowing.
By combining physical exams, medical history, and diagnostic tests, your doctor can accurately diagnose PVD and develop an effective treatment plan. 💊
PVD Treatment Options and Medications
When it comes to managing Peripheral Vascular Disease (PVD), a combination of lifestyle changes, medications, and medical procedures can help alleviate symptoms and improve overall quality of life. In this section, we’ll delve into the various treatment options and medications available for PVD.
Medications for PVD
Medications play a crucial role in managing PVD symptoms and preventing complications. Your doctor may prescribe one or more of the following medications:
- Cilostazol: This medication helps improve blood flow to the legs and reduces symptoms of claudication.
- Pentoxifylline: This medication improves blood flow and reduces blood viscosity, making it easier for blood to flow through narrowed arteries.
- Anti-platelet agents: Medications like aspirin or clopidogrel help prevent blood clots from forming and reduce the risk of heart attack and stroke.
- Blood pressure medications: If you have high blood pressure, your doctor may prescribe medications to help manage it, as high blood pressure can worsen PVD symptoms.
- Cholesterol-lowering medications: Statins or other cholesterol-lowering medications can help reduce the risk of heart attack and stroke by lowering cholesterol levels.
Medical Procedures for PVD
In addition to medications, various medical procedures can help improve blood flow and alleviate PVD symptoms. These may include:
- Angioplasty: A minimally invasive procedure where a balloon-tipped catheter is used to widen narrowed or blocked arteries.
- Stenting: A small mesh tube (stent) is placed in the artery to keep it open and improve blood flow.
- Atherectomy: A procedure where a catheter with a small cutting device is used to remove plaque from the artery walls.
- Bypass surgery: In severe cases, bypass surgery may be necessary to redirect blood flow around blocked arteries.
Lifestyle Changes for Managing PVD
While medications and medical procedures can help manage PVD, making lifestyle changes is essential to alleviate symptoms and slow disease progression. Here are some lifestyle changes you can make to manage PVD:
Exercise and Physical Activity
Regular exercise can help improve blood flow and reduce PVD symptoms. Aim for at least 30 minutes of moderate-intensity exercise, such as brisk walking, cycling, or swimming, three to four times a week. 🏋️♀️
Smoking Cessation
Smoking is a significant risk factor for PVD, and quitting can greatly improve your overall health. Talk to your doctor about smoking cessation programs and nicotine replacement therapy. 🚭
Dietary Changes
Eating a healthy, balanced diet can help manage PVD symptoms and reduce the risk of complications. Focus on:
- Fruits and vegetables: Aim for at least five servings a day to help lower blood pressure and cholesterol levels.
- Whole grains: Choose whole grains over refined or processed grains to help lower cholesterol levels and improve blood sugar control.
- Lean protein: Opt for lean protein sources like poultry, fish, and legumes to help lower cholesterol levels and improve overall health.
- Low-sodium diet: Limit sodium intake to help lower blood pressure and reduce the risk of complications.
Stress Management
Chronic stress can worsen PVD symptoms and increase the risk of complications. Engage in stress-reducing activities like yoga, meditation, or deep breathing exercises to help manage stress. 🙏
By making these lifestyle changes and working with your healthcare provider to develop a comprehensive treatment plan, you can effectively manage PVD symptoms and improve your overall quality of life. 💪

PVD Complications and Related Conditions
Peripheral Vascular Disease (PVD) is a serious condition that can lead to severe complications if left untreated or poorly managed. In this section, we’ll explore the potential complications and related conditions associated with PVD.
Complications of PVD
PVD can lead to a range of complications, including:
- Amputation: In severe cases, PVD can cause gangrene or tissue death, leading to amputation of the affected limb.
- Heart Attack or Stroke: The same plaque buildup that causes PVD can also lead to heart attacks or strokes if it blocks blood flow to the heart or brain.
- Kidney Damage: Reduced blood flow to the kidneys can cause kidney damage or failure.
- Impotence: PVD can cause erectile dysfunction in men due to reduced blood flow to the genitals.
- Ulcers and Wounds: Poor blood flow can lead to slow-healing wounds or ulcers on the legs or feet.
Related Conditions
PVD is often linked to other conditions that share similar risk factors or symptoms. These include:
- Diabetes: People with diabetes are more likely to develop PVD due to high blood sugar levels damaging blood vessels.
- High Blood Pressure: Uncontrolled high blood pressure can contribute to PVD by damaging blood vessels.
- High Cholesterol: High cholesterol levels can lead to plaque buildup in blood vessels, increasing the risk of PVD.
- Raynaud’s Disease: This condition causes blood vessels to constrict in response to cold temperatures or stress, leading to discoloration and numbness in the fingers and toes.
- Chronic Kidney Disease: Kidney disease can increase the risk of PVD due to the buildup of waste products in the blood.
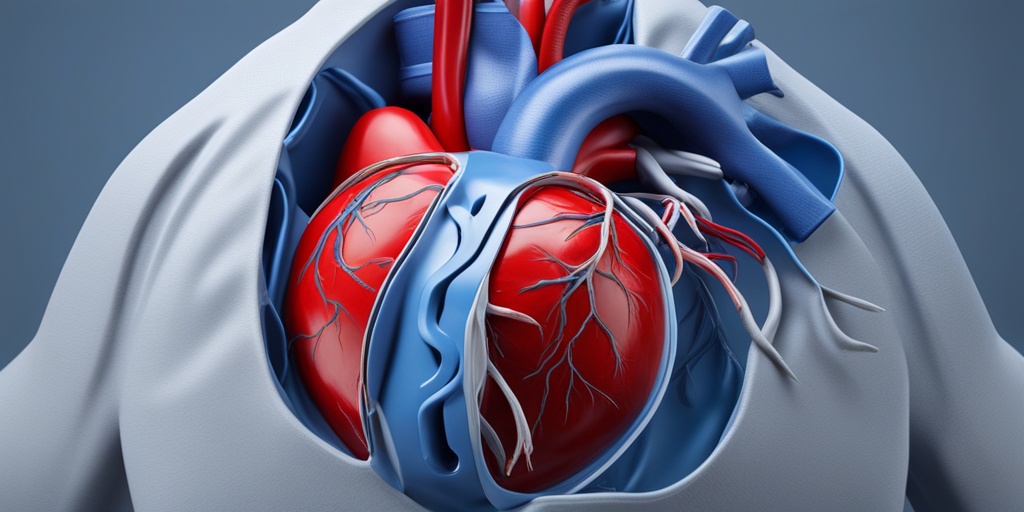
Peripheral Vascular Disease and Heart Health
PVD is often referred to as a “window” to cardiovascular health. This is because the same factors that contribute to PVD, such as plaque buildup and narrowed arteries, can also increase the risk of heart disease.
The Connection Between PVD and Heart Health
Research has shown that people with PVD are more likely to develop heart disease or experience a heart attack or stroke. This is because:
- Shared Risk Factors: PVD and heart disease share common risk factors, such as high blood pressure, high cholesterol, and smoking.
- Plaque Buildup: The same plaque buildup that causes PVD can also block blood flow to the heart, leading to heart attacks or strokes.
- Inflammation: Chronic inflammation, which is often present in PVD, can also contribute to heart disease.
Given the strong connection between PVD and heart health, it’s essential to manage PVD symptoms and risk factors to reduce the risk of heart disease. This includes making lifestyle changes, such as quitting smoking, exercising regularly, and eating a healthy diet, as well as working with your healthcare provider to manage underlying conditions. 💊
Frequently Asked Questions about PVD (Peripheral Vascular Disease)
What is PVD (Peripheral Vascular Disease)?
PVD, also known as Peripheral Artery Disease (PAD), is a common circulatory problem in which narrowed or blocked arteries reduce blood flow to the limbs. It is often associated with atherosclerosis, a buildup of plaque in the arteries.
What are the Symptoms of PVD?
The most common symptom of PVD is leg pain when walking, but it can also cause other symptoms like:
- Numbness and tingling in the legs, feet, or toes
- Weakness or cramping in the legs
- Coldness in the legs or feet
- Discoloration of the legs or feet
- Ulcers or wounds that are slow to heal
What are the Causes of PVD?
PVD is often caused by:
- Atherosclerosis, a buildup of plaque in the arteries
- High blood pressure
- High cholesterol
- Diabetes
- Smoking
- Obesity
- Physical inactivity
How is PVD Diagnosed?
PVD is diagnosed through a combination of:
- Physical examination
- Medical history
- Imaging tests, such as ultrasound or angiography
- Ankle-brachial index (ABI) test, which compares blood pressure in the legs to blood pressure in the arms
How is PVD Treated?
Treatment for PVD usually involves:
- Lifestyle changes, such as quitting smoking, exercising regularly, and losing weight
- Medications, such as blood thinners, medications to lower blood pressure and cholesterol, and pain relievers
- Angioplasty, a minimally invasive procedure to open up blocked arteries
- Surgery, such as bypass grafting, to restore blood flow to the legs
What is the ICD 10 Code for PVD with Claudication?
The ICD 10 code for PVD with claudication is I73.9.
Can PVD be Reversed?
While PVD cannot be completely reversed, early diagnosis and treatment can help slow or stop the progression of the disease. Lifestyle changes and medications can also help manage symptoms and improve quality of life 💪.