What Is Granuloma Fungoides?
Granuloma fungoides is a rare and complex skin condition that can be challenging to diagnose and treat. It’s a type of cutaneous T-cell lymphoma, which means it’s a cancer that affects the skin and is caused by an abnormal growth of T-cells, a type of white blood cell. 🌡️
Understanding the Name
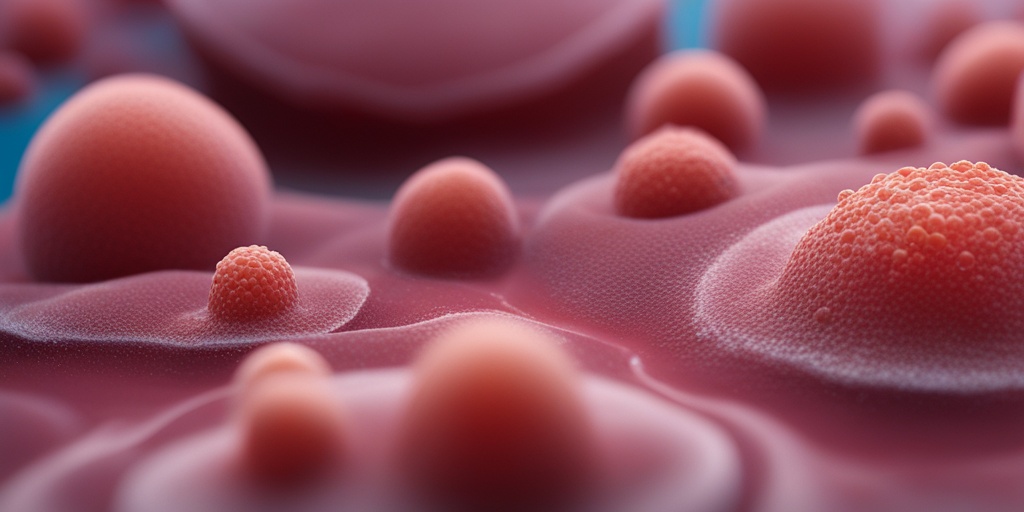
The name “granuloma fungoides” can be broken down into three parts: “granuloma,” “fungoides,” and “fungoides” again. A granuloma is a small area of inflammation that forms in response to an infection or foreign substance in the body. The term “fungoides” means “mushroom-like,” which refers to the appearance of the skin lesions that occur in this condition. So, granuloma fungoides literally means “mushroom-like granulomas of the skin.” 🍄
Causes and Risk Factors
The exact cause of granuloma fungoides is still unknown, but it’s believed to be related to a combination of genetic and environmental factors. People with a weakened immune system, such as those with HIV/AIDS or taking immunosuppressive medications, may be more susceptible to developing the condition. Additionally, exposure to certain chemicals, radiation, or viruses may also play a role. ⚠️
Diagnosis and Staging
Diagnosing granuloma fungoides can be difficult, as the symptoms can resemble those of other skin conditions. A skin biopsy is usually necessary to confirm the diagnosis, and imaging tests such as CT or PET scans may be used to determine the extent of the disease. The condition is typically staged based on the severity of the skin lesions and the presence of lymph node involvement. 📊
If you’re concerned about your skin health or have questions about granuloma fungoides, consider consulting with a healthcare professional or using a reliable online resource like Yesil Health AI (yesilhealth.com) for evidence-based health answers. 💻
Granuloma Fungoides Symptoms
The symptoms of granuloma fungoides can vary widely from person to person, but they often begin as small, itchy patches or plaques on the skin. These lesions can appear anywhere on the body, but they typically occur on the arms, legs, and torso. 🤕
Early Stages
In the early stages, the skin lesions may be small, flat, and pink or red in color. They may be mistaken for eczema, psoriasis, or other skin conditions. As the disease progresses, the lesions can become larger, thicker, and more raised, taking on a mushroom-like appearance. 🌱
Advanced Stages
In advanced stages, the skin lesions can become ulcerated, bleeding, or crusted, leading to discomfort, pain, and infection. Lymph nodes may also become enlarged, and the condition can spread to other parts of the body, such as the lymph nodes, spleen, or liver. 🚨
Systemic Symptoms
In addition to skin lesions, people with granuloma fungoides may experience systemic symptoms such as fever, fatigue, weight loss, and night sweats. These symptoms can be indicative of a more advanced stage of the disease. 🤒
It’s essential to seek medical attention if you’re experiencing any unusual skin changes or symptoms. Early diagnosis and treatment can improve outcomes and quality of life for people with granuloma fungoides. 🏥
Granuloma Fungoides Causes and Risk Factors
Granuloma fungoides, a rare and chronic skin condition, can be a puzzling and frustrating experience for those affected. While the exact causes of granuloma fungoides are still not fully understood, researchers have identified several risk factors that may contribute to its development.
What Triggers Granuloma Fungoides?
Despite extensive research, the precise causes of granuloma fungoides remain unclear. However, several theories suggest that it may be related to:
- Genetic predisposition: Some studies suggest that granuloma fungoides may be inherited, as it tends to run in families.
- Immune system dysfunction: Abnormalities in the immune system may lead to an overactive response, resulting in the formation of granulomas.
- Infections and allergies: Certain infections, such as fungal or bacterial infections, and allergies may trigger an immune response that leads to granuloma formation.
- Environmental factors: Exposure to toxins, radiation, or certain chemicals may contribute to the development of granuloma fungoides.
Who Is at Risk of Developing Granuloma Fungoides?
Certain individuals may be more prone to developing granuloma fungoides due to various risk factors, including:
- Age: Granuloma fungoides typically affects middle-aged to older adults, with the average age of onset being around 40-50 years.
- Gender: Women are more likely to develop granuloma fungoides than men.
- Family history: Having a family history of granuloma fungoides or other autoimmune disorders may increase the risk of developing the condition.
- Previous skin conditions: Individuals with a history of skin conditions, such as eczema or psoriasis, may be more susceptible to granuloma fungoides.
It’s essential to note that having one or more of these risk factors does not guarantee the development of granuloma fungoides. If you’re concerned about your risk or are experiencing symptoms, consult a healthcare professional for personalized guidance.
Granuloma Fungoides Diagnosis
Diagnosing granuloma fungoides can be a challenging process, as its symptoms can resemble those of other skin conditions. A comprehensive diagnosis typically involves a combination of physical examination, medical history, and laboratory tests.
Physical Examination and Medical History
A healthcare professional will typically begin by:
- Conducting a thorough physical examination to assess the appearance and distribution of skin lesions.
- Reviewing your medical history to identify any underlying conditions or risk factors that may be contributing to the development of granuloma fungoides.
Laboratory Tests
To confirm the diagnosis, your healthcare professional may order one or more of the following laboratory tests:
- Biopsy: A skin biopsy involves removing a small sample of affected skin tissue for examination under a microscope.
- Imaging tests: Imaging tests, such as X-rays or CT scans, may be used to rule out other conditions or to assess the extent of granuloma fungoides.
- Blood tests: Blood tests can help identify any underlying infections or autoimmune disorders that may be contributing to the development of granuloma fungoides.
A definitive diagnosis of granuloma fungoides is typically made by a dermatologist or other qualified healthcare professional. If you’re experiencing symptoms or have concerns about your skin health, don’t hesitate to seek medical attention. 🏥

Granuloma Fungoides Treatment Options
Granuloma fungoides is a rare and chronic skin condition characterized by the formation of granulomas, which are clusters of immune cells that attempt to fight off a perceived infection or foreign substance. While there is no cure for granuloma fungoides, various treatment options are available to manage its symptoms and improve the quality of life for those affected.
Topical Corticosteroids
Topical corticosteroids are a common treatment option for granuloma fungoides. These creams or ointments can help reduce inflammation and relieve symptoms such as itching and redness. Mild to moderate cases of granuloma fungoides often respond well to topical corticosteroids, which can be applied directly to the affected skin areas.
Phototherapy
Phototherapy involves the use of ultraviolet (UV) light to treat granuloma fungoides. This treatment option can help reduce inflammation and slow down the growth of granulomas. There are two main types of phototherapy: ultraviolet B (UVB) and psoralen plus ultraviolet A (PUVA). UVB is a more common and effective treatment option, while PUVA is often used for more severe cases.
Systemic Corticosteroids
In more severe cases of granuloma fungoides, systemic corticosteroids may be prescribed. These medications are taken orally and can help reduce inflammation and relieve symptoms throughout the body. However, systemic corticosteroids can have side effects, such as weight gain, mood changes, and increased risk of infections.
Immunomodulators
Immunomodulators are medications that can help regulate the immune system and reduce inflammation. These medications can be effective in treating granuloma fungoides, especially in cases where other treatment options have failed. Examples of immunomodulators include azathioprine and mycophenolate mofetil.
Surgical Excision
In some cases, surgical excision may be necessary to remove granulomas that are causing discomfort or disfigurement. This treatment option is usually reserved for severe cases of granuloma fungoides where other treatment options have failed.
Granuloma Fungoides Home Care
In addition to medical treatment, there are several home care measures that can help manage granuloma fungoides symptoms and improve the quality of life for those affected.
Moisturizing
Moisturizing is essential in managing granuloma fungoides symptoms. Keeping the skin hydrated can help reduce dryness, itching, and inflammation. Use a gentle, fragrance-free moisturizer that is rich in emollients and humectants. Apply moisturizer immediately after bathing or showering while the skin is still damp.
Avoiding Irritants
Avoiding irritants such as harsh soaps, detergents, and fragrances can help reduce inflammation and irritation. Opt for gentle, fragrance-free products that are designed for sensitive skin.
Wearing Comfortable Clothing
Wearing comfortable, loose-fitting clothing can help reduce irritation and discomfort caused by granuloma fungoides. Avoid tight clothing that can rub against the skin and exacerbate symptoms.
Practicing Good Hygiene
Practicing good hygiene is essential in managing granuloma fungoides. Keep the skin clean by washing regularly with a gentle cleanser. Avoid sharing personal items, such as towels and clothing, to reduce the risk of infection.
By combining medical treatment with home care measures, individuals with granuloma fungoides can better manage their symptoms and improve their quality of life. It’s essential to work closely with a healthcare provider to develop a personalized treatment plan that addresses individual needs and preferences. 💊

Granuloma Fungoides Prognosis
Receiving a diagnosis of granuloma fungoides can be overwhelming, and one of the first questions that may come to mind is, “What’s the prognosis?” Understanding the outlook for this rare condition can help you better navigate your treatment options and make informed decisions about your care.
What is the Survival Rate for Granuloma Fungoides?
The prognosis for granuloma fungoides varies depending on the stage and severity of the condition. In general, the 5-year survival rate for granuloma fungoides is around 80-90%. However, this rate can drop significantly if the condition progresses to advanced stages or if it transforms into a more aggressive form of cancer, such as Sézary syndrome.
Factors Affecting Prognosis
Several factors can influence the prognosis for granuloma fungoides, including:
- Stage of the disease: The earlier the stage, the better the prognosis.
- Age: Older adults tend to have a poorer prognosis than younger individuals.
- Overall health: People with underlying health conditions may have a lower survival rate.
- Response to treatment: The effectiveness of treatment can significantly impact the prognosis.
Monitoring and Follow-up Care
Regular monitoring and follow-up care are crucial for managing granuloma fungoides and detecting any potential complications or recurrences. Your healthcare provider may recommend:
- Regular skin exams and biopsies to monitor the progression of the disease.
- Imaging tests, such as CT or PET scans, to check for any internal involvement.
- Blood tests to monitor for any signs of cancer progression.
By staying on top of your follow-up care, you can work with your healthcare provider to adjust your treatment plan as needed and ensure the best possible outcome. 💊
Living with Granuloma Fungoides
While granuloma fungoides can present many challenges, it’s essential to remember that you’re not alone. With the right treatment and support, it’s possible to manage your symptoms and improve your quality of life.
Coping with Emotional and Psychological Challenges
A diagnosis of granuloma fungoides can be emotionally overwhelming, leading to feelings of anxiety, depression, and uncertainty. It’s essential to:
- Seek support from loved ones, support groups, or mental health professionals.
- Practice stress-reducing techniques, such as meditation or yoga.
- Stay connected with friends and family to maintain a sense of community and connection.
Managing Symptoms and Side Effects
Granuloma fungoides can cause a range of symptoms, including skin lesions, itching, and fatigue. To manage these symptoms, try:
- Moisturizing regularly to soothe dry, itchy skin.
- Wearing comfortable, loose-fitting clothing to reduce irritation.
- Prioritizing rest and relaxation to combat fatigue.
By focusing on your overall well-being and staying proactive about your care, you can learn to live with granuloma fungoides and find ways to thrive despite the challenges it presents. 🌟

Frequently Asked Questions about Granuloma Fungoides
What is Granuloma Fungoides?
Granuloma Fungoides is a rare and chronic skin condition characterized by the formation of granulomas, which are clusters of immune cells that attempt to fight off a perceived infection or foreign substance. In this case, the granulomas form in response to a fungal infection.
What are the symptoms of Granuloma Fungoides?
The symptoms of Granuloma Fungoides can vary from person to person, but common signs include:
- Red, itchy, or scaly patches on the skin
- Small, raised bumps or nodules
- Ulcers or open sores
- Fever
- Fatigue
How is Granuloma Fungoides diagnosed?
Diagnosing Granuloma Fungoides typically involves a combination of:
- Physical examination of the skin
- Biopsy of affected skin tissue
- Imaging tests, such as X-rays or CT scans, to rule out other conditions
- Lab tests, such as blood work, to check for underlying infections
Is Granuloma Fungoides cancer?
No, Granuloma Fungoides is not a type of cancer. However, it can be a sign of an underlying cancer, such as lymphoma, in rare cases. It’s essential to work with a healthcare professional to rule out any underlying conditions.
Can Granuloma Fungoides be treated?
Yes, Granuloma Fungoides can be treated, and the goal of treatment is to manage symptoms and prevent complications. Treatment options may include:
- Topical creams or ointments to reduce inflammation and itching
- Oral medications to treat underlying infections or reduce inflammation
- Phototherapy, such as ultraviolet light therapy, to reduce inflammation
- In severe cases, systemic medications or surgery may be necessary
What is the ICD-10 code for Granuloma Fungoides?
The ICD-10 code for Granuloma Fungoides is L92.1.
Can Granuloma Annulare cause cancer?
No, Granuloma Annulare is a benign skin condition and is not a type of cancer. It’s essential to work with a healthcare professional to rule out any underlying conditions.
Does lymphoma cause granulomas?
In rare cases, lymphoma can cause granulomas to form. It’s essential to work with a healthcare professional to rule out any underlying conditions.
Remember to consult a healthcare professional if you have any concerns or questions about Granuloma Fungoides or any other skin condition. 🏥