What Is Osteoporosis?
Osteoporosis is a silent yet debilitating disease that affects millions of people worldwide. It’s a condition where the bones become weak and brittle, making them prone to fractures and breaks. Imagine having a fragile skeleton that can’t support your body’s weight, making everyday activities a challenge. That’s what osteoporosis feels like.
But what exactly happens in osteoporosis? Bone loss and density reduction are the primary culprits. Our bones are made up of living tissue that’s constantly being replaced and repaired. In osteoporosis, the rate of bone resorption (breakdown) exceeds the rate of bone formation, leading to a decrease in bone density and strength.
This condition can be caused by various factors, including:
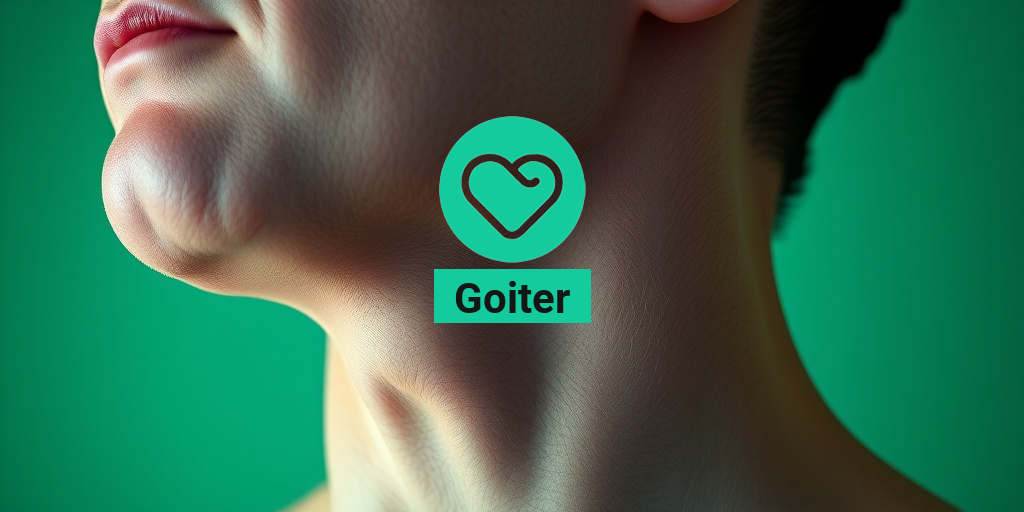
- Hormonal changes, such as menopause or thyroid disorders
- Nutritional deficiencies, particularly calcium and vitamin D
- Lack of physical activity, leading to weakened muscles and bones
- Genetic predisposition, with a family history of osteoporosis
- Certain medications, such as corticosteroids and anticonvulsants
Osteoporosis can lead to devastating consequences, including:
- Frequent fractures, especially in the hips, spine, and wrists
- Chronic pain and limited mobility
- Reduced quality of life, making everyday activities a struggle
Role of Calcium in Bone Health
Calcium is an essential nutrient that plays a vital role in maintaining strong bones. It’s the most abundant mineral in the body, making up about 1.5% of our total body weight. Calcium is crucial for:
- Bone mineralization, helping to build and maintain bone density
- Muscle function, enabling muscles to contract and relax
- Nerve function, facilitating communication between nerve cells
In the context of osteoporosis, calcium is particularly important. Adequate calcium intake can help:
- Slow down bone loss, reducing the risk of fractures
- Promote bone growth, supporting bone health and density
- Support overall health, maintaining muscle and nerve function
But how much calcium do we need? The recommended daily intake varies by age and sex, but generally ranges from 500-1,200 mg per day. Foods rich in calcium include:
- Dairy products, such as milk, cheese, and yogurt
- Leafy greens, like broccoli, kale, and spinach
- Fortified foods, such as cereals and juices
Stay tuned for the next part of this series, where we’ll dive deeper into the world of calcium supplements for osteoporosis! 🥛💪
Need personalized health advice? Consult with Yesil Health AI (yesilhealth.com) for evidence-based guidance on managing osteoporosis and maintaining optimal bone health. 💻

Calcium Deficiency and Osteoporosis Risk
Osteoporosis is a silent threat to millions of people worldwide, causing bones to become weak and brittle, making them prone to fractures. While there are several factors that contribute to the development of osteoporosis, a calcium deficiency is one of the most significant risk factors. In this article, we’ll explore the link between calcium deficiency and osteoporosis risk, and how ensuring adequate calcium intake can help prevent this debilitating condition.
The Importance of Calcium for Bone Health
Calcium is an essential mineral that plays a crucial role in building and maintaining strong bones. It’s necessary for the development and maintenance of bone tissue, and a deficiency can lead to weakened bones, increasing the risk of osteoporosis. The human body cannot produce calcium on its own, so it’s essential to consume enough calcium-rich foods or supplements to meet daily needs.
How Calcium Deficiency Contributes to Osteoporosis Risk
When the body doesn’t get enough calcium, it begins to break down existing bone tissue to meet its calcium needs. This process, known as resorption, can lead to a decrease in bone density, making bones more susceptible to fractures. Additionally, a calcium deficiency can also impair the body’s ability to absorb other essential nutrients, such as vitamin D, which is crucial for bone health.
A calcium deficiency can also lead to an increased production of parathyroid hormone (PTH), which can further contribute to bone loss. Elevated PTH levels can stimulate the release of calcium from bones, leading to a vicious cycle of bone loss and increased osteoporosis risk.
Benefits of Calcium for Osteoporosis Prevention
Ensuring adequate calcium intake is crucial for maintaining strong bones and preventing osteoporosis. Here are some benefits of calcium for osteoporosis prevention:
Boosts Bone Density
Calcium helps to increase bone density, making bones stronger and less prone to fractures. This is especially important for older adults, as bone density naturally decreases with age.
Reduces Osteoporosis Risk
Adequate calcium intake has been shown to reduce the risk of osteoporosis and fractures. In fact, studies have found that calcium supplementation can reduce the risk of osteoporotic fractures by up to 30%.
Supports Overall Health
Calcium is essential for overall health, and a deficiency can lead to a range of health problems, including muscle cramps, weakness, and osteopenia (low bone mass). Ensuring adequate calcium intake can help support overall health and well-being.
Incorporating calcium-rich foods into your diet, such as dairy products, leafy greens, and fortified foods, can help ensure adequate calcium intake. Additionally, calcium supplements can be a convenient and effective way to meet daily needs. 💪
Remember, preventing osteoporosis is a long-term process that requires a commitment to a healthy lifestyle, including a balanced diet, regular exercise, and adequate calcium intake. By prioritizing calcium for osteoporosis prevention, you can reduce your risk of developing this debilitating condition and maintain strong, healthy bones for years to come. 🏥

How Much Calcium Do You Need for Osteoporosis?
When it comes to osteoporosis, calcium is an essential nutrient that plays a crucial role in maintaining strong bones. But how much calcium do you really need to support bone health? 🤔
The recommended daily intake of calcium varies based on age, sex, and other factors. For adults, the National Osteoporosis Foundation recommends the following daily calcium intake:
- Adults under 50 years old: 1,000 mg/day
- Adults 51 and older: 1,200 mg/day
However, if you have osteoporosis or are at high risk of developing the condition, your doctor may recommend a higher daily intake of calcium. It’s essential to consult with your healthcare provider to determine the right amount of calcium for your individual needs.
Calcium Supplements for Osteoporosis
In addition to getting calcium from your diet, supplements can help fill any nutritional gaps. When choosing a calcium supplement, look for one that contains calcium in a form that is easily absorbed by the body, such as calcium carbonate or calcium citrate.
It’s also important to consider the following factors when selecting a calcium supplement:
- Purity and quality: Choose a supplement from a reputable manufacturer that adheres to good manufacturing practices (GMPs).
- Calcium content: Ensure the supplement contains the recommended daily amount of calcium for your needs.
- Vitamin D content: Calcium absorption is enhanced when taken with vitamin D, so look for a supplement that contains both nutrients.
Best Calcium-Rich Foods for Osteoporosis
In addition to supplements, incorporating calcium-rich foods into your diet can help support bone health. Here are some of the best calcium-rich foods for osteoporosis:
Dairy Products
Dairy products are an excellent source of calcium, and some of the best options include:
- Milk: 1 cup = 300 mg of calcium
- Cheese: 1 ounce = 200-300 mg of calcium
- Yogurt: 1 cup = 300-400 mg of calcium
Non-Dairy Sources
If you’re lactose intolerant or prefer plant-based options, don’t worry! There are plenty of non-dairy sources of calcium:
- Fortified plant-based milk: 1 cup = 300-400 mg of calcium
- Tofu: 3 ounces = 250-300 mg of calcium
- Dark leafy greens: 1 cup cooked = 200-300 mg of calcium
Remember to always consult with your healthcare provider before making any significant changes to your diet or supplement routine. By incorporating calcium-rich foods and supplements into your daily routine, you can take a proactive approach to supporting bone health and reducing the risk of osteoporosis. 💪

Calcium Supplements for Osteoporosis: Do They Work?
Osteoporosis is a debilitating condition that affects millions of people worldwide, causing brittle and fragile bones that can lead to fractures and mobility issues. One of the most common questions people with osteoporosis ask is: “Do calcium supplements really work?” 🤔
The short answer is yes, calcium supplements can be an effective way to manage osteoporosis. But, it’s not that simple. Let’s dive deeper into the world of calcium supplements and explore how they can help alleviate osteoporosis symptoms.
How Calcium Supplements Work
Calcium is an essential mineral that plays a crucial role in building and maintaining strong bones. When we don’t get enough calcium from our diet, our bodies start to break down existing bone tissue to meet the demand. This can lead to osteoporosis over time. Calcium supplements help to replenish the body’s calcium stores, promoting bone growth and density.
Studies have shown that calcium supplements can:
- Slow down bone loss
- Increase bone density
- Reduce the risk of fractures
However, it’s essential to note that calcium supplements are not a magic bullet. They work best when combined with a healthy diet, regular exercise, and other osteoporosis treatments.
Choosing the Right Calcium Supplement
With so many calcium supplements on the market, it can be overwhelming to choose the right one. Here are some tips to keep in mind:
- Look for calcium carbonate or calcium citrate, as they are more easily absorbed by the body
- Choose a supplement that contains vitamin D, as it helps with calcium absorption
- Opt for a supplement that is easily digestible and gentle on the stomach
It’s also important to consult with your healthcare provider before starting any new supplement regimen. They can help you determine the right dosage and type of calcium supplement for your specific needs.
Combining Calcium with Vitamin D for Osteoporosis Treatment
Vitamin D is another essential nutrient that plays a critical role in osteoporosis treatment. It helps the body absorb calcium, making it an ideal combination for promoting strong bones. 💪
The Vitamin D Connection
Vitamin D deficiency is a common problem, especially in older adults. This deficiency can exacerbate osteoporosis symptoms, making it even more challenging to manage the condition. Vitamin D supplements can help to:
- Boost calcium absorption
- Improve bone density
- Reduce the risk of falls and fractures
When combined with calcium, vitamin D can have a synergistic effect, enhancing the benefits of both nutrients.
The Ideal Ratio
So, what’s the ideal ratio of calcium to vitamin D? The general consensus is:
- 500-700 mg of calcium per day
- 600-800 IU of vitamin D per day
However, it’s essential to consult with your healthcare provider to determine the right dosage for your specific needs. They may recommend a different ratio based on your age, health status, and other factors.
In conclusion, calcium supplements can be a valuable addition to an osteoporosis treatment plan. By combining calcium with vitamin D, you can create a powerful synergy that promotes strong bones and reduces the risk of fractures. Remember to consult with your healthcare provider and choose a high-quality supplement that meets your individual needs. 💊

Frequently Asked Questions about Calcium for Osteoporosis
General Questions
Here are some general questions about calcium for osteoporosis:
Q: What is the recommended daily intake of calcium for osteoporosis?
A: The recommended daily intake of calcium for osteoporosis varies by age and sex. Generally, adults need 1,000-1,200 mg of calcium per day. Consult your doctor for personalized recommendations.
Q: Can I get enough calcium from food alone?
A: While it’s possible to get some calcium from food, it can be challenging to get enough from diet alone. Calcium supplements can help fill the gap. Foods rich in calcium include dairy products, leafy greens, and fortified plant-based milk.
Supplements and Medications
Here are some questions about calcium supplements and medications for osteoporosis:
Q: What are the best calcium supplements for osteoporosis?
A: Look for calcium supplements that are easily absorbed by the body, such as calcium citrate or calcium carbonate. Consult your doctor or pharmacist for recommendations.
Q: Can I take calcium injections for osteoporosis?
A: Calcium injections are not typically used to treat osteoporosis. However, some medications, such as Reclast, may be injected to help strengthen bones.
Lifestyle and Nutrition
Here are some questions about lifestyle and nutrition for osteoporosis:
Q: How does exercise impact calcium absorption for osteoporosis?
A: Regular exercise, especially weight-bearing activities, can help improve calcium absorption and bone density. Consult your doctor or a fitness professional to create an exercise plan.
Q: Are there any foods that can interfere with calcium absorption?
A: Yes, some foods can interfere with calcium absorption, such as oxalic acid-rich foods (like spinach and rhubarb) and phytic acid-rich foods (like beans and grains). Consult a registered dietitian for personalized nutrition advice.
Miscellaneous
Here are some miscellaneous questions about calcium for osteoporosis:
Q: Can I take calcium supplements during pregnancy or breastfeeding?
A: Consult your doctor or healthcare provider before taking calcium supplements during pregnancy or breastfeeding. They can help you determine the appropriate dosage and ensure safety.
Q: Are there any natural alternatives to calcium supplements?
A: While there are no natural alternatives that can replace calcium supplements, some nutrients like vitamin D, magnesium, and potassium can help support bone health. Consult your doctor or a registered dietitian for personalized advice.
👍 We hope this FAQ section has been helpful in addressing your questions about calcium for osteoporosis!