What Is Pancreatic Cancer?
Pancreatic cancer is a type of cancer that begins in the tissues of the pancreas, an organ located behind the stomach that plays a crucial role in digestion and blood sugar regulation. This cancer is particularly notorious for its aggressive nature and often presents a challenge in early detection. The pancreas produces enzymes that help digest food and hormones, such as insulin, that regulate blood sugar levels.
There are two main types of pancreatic cancer:
- Exocrine tumors: These are the most common type, accounting for about 95% of cases. They typically arise from the cells that produce digestive enzymes.
- Endocrine tumors: These tumors are less common and develop from the hormone-producing cells of the pancreas.
Understanding pancreatic cancer is vital, especially considering its survival rate is relatively low compared to other cancers. The pancreatic cancer prognosis often depends on the stage at which the cancer is diagnosed. Unfortunately, many patients are diagnosed at an advanced stage, which complicates treatment options.
Pancreatic Cancer Symptoms
Recognizing the symptoms of pancreatic cancer early can be challenging, as they often do not appear until the disease is advanced. However, being aware of the potential signs can lead to earlier diagnosis and better outcomes. Here are some common symptoms to watch for:
1. Abdominal Pain
Many patients report experiencing persistent abdominal pain that may radiate to the back. This discomfort can be dull or sharp and is often mistaken for other gastrointestinal issues.
2. Unexplained Weight Loss
Sudden and unexplained weight loss is a common symptom of pancreatic cancer. This can occur due to a loss of appetite or the body’s inability to properly digest food.
3. Jaundice
Jaundice, characterized by yellowing of the skin and eyes, can occur when the cancer blocks the bile duct. This blockage prevents bile from flowing into the intestine, leading to a buildup of bilirubin in the blood.
4. Changes in Stool
Patients may notice changes in their stool, such as pale, greasy, or floating stools. This can indicate that the pancreas is not producing enough digestive enzymes.
5. New-Onset Diabetes
In some cases, pancreatic cancer can lead to new-onset diabetes, particularly in older adults. This occurs when the cancer affects the insulin-producing cells of the pancreas.
6. Fatigue and Weakness
Persistent fatigue and weakness are common symptoms that can accompany many types of cancer, including pancreatic cancer. These feelings can be exacerbated by the body’s response to the disease.
If you or someone you know is experiencing these symptoms, it is crucial to consult a healthcare professional for further evaluation. Early detection can significantly impact the pancreatic cancer treatment options available and improve the overall prognosis.
For more information on pancreatic cancer and its management, consider visiting Yesil Health AI, a valuable resource for evidence-based health answers. Remember, knowledge is power when it comes to health!
Stay informed and proactive about your health, and don’t hesitate to seek medical advice if you have concerns regarding pancreatic cancer or any other health issues. 🌟

Risk Factors for Pancreatic Cancer
Understanding the risk factors for pancreatic cancer is crucial for early detection and prevention. While the exact cause of pancreatic cancer remains unclear, several factors can increase an individual’s likelihood of developing this aggressive disease.
Age
Age is one of the most significant risk factors for pancreatic cancer. The majority of cases are diagnosed in individuals over the age of 65. As we age, our cells undergo changes that may increase the risk of cancerous growths.
Smoking
Smoking is a well-established risk factor for pancreatic cancer. Studies show that smokers are twice as likely to develop this disease compared to non-smokers. The harmful chemicals in tobacco can damage the pancreas and lead to cancerous changes.
Obesity
Being overweight or obese can also increase the risk of pancreatic cancer. Excess body fat, particularly around the abdomen, is linked to inflammation and insulin resistance, both of which can contribute to cancer development.
Diabetes
There is a strong connection between diabetes and pancreatic cancer. Individuals with diabetes, especially type 2 diabetes, have a higher risk of developing pancreatic cancer. This may be due to the underlying metabolic changes associated with diabetes.
Family History and Genetics
A family history of pancreatic cancer can significantly elevate your risk. Genetic mutations, such as those in the BRCA2 gene, can also increase susceptibility. If you have a family history of pancreatic cancer or related syndromes, it’s essential to discuss this with your healthcare provider.
Chronic Pancreatitis
Chronic inflammation of the pancreas, known as chronic pancreatitis, can increase the risk of pancreatic cancer. This condition can result from long-term alcohol abuse, certain genetic disorders, or autoimmune diseases.
Exposure to Chemicals
Exposure to certain chemicals, such as those used in the metalworking and dry cleaning industries, may also increase the risk of pancreatic cancer. It’s important to take precautions if you work in environments where these chemicals are prevalent.
Causes of Pancreatic Cancer
While the exact causes of pancreatic cancer are still being researched, several factors have been identified that may contribute to the development of this disease.
Genetic Mutations
Genetic mutations play a significant role in the development of pancreatic cancer. Mutations in genes such as KRAS, TP53, and CDKN2A are commonly found in pancreatic tumors. These mutations can disrupt normal cell growth and division, leading to cancer.
Environmental Factors
Environmental factors, including exposure to certain chemicals and toxins, can also contribute to the risk of pancreatic cancer. Research suggests that long-term exposure to pesticides, industrial chemicals, and even some food additives may play a role.
Dietary Choices
Your diet can influence your risk of developing pancreatic cancer. Diets high in red and processed meats, refined sugars, and low in fruits and vegetables may increase the risk. Conversely, a diet rich in antioxidants and healthy fats may help reduce the risk.
Chronic Inflammation
Chronic inflammation of the pancreas, as seen in conditions like chronic pancreatitis, can lead to cellular changes that increase the risk of cancer. This inflammation can be triggered by factors such as excessive alcohol consumption or gallstones.
Hormonal Factors
Hormonal changes, particularly those related to insulin and glucose metabolism, may also play a role in the development of pancreatic cancer. Insulin resistance and high levels of insulin can promote the growth of pancreatic cells, potentially leading to cancer.
In summary, while there is no single cause of pancreatic cancer, a combination of genetic, environmental, and lifestyle factors can contribute to its development. Being aware of these risk factors and causes can empower individuals to make informed health choices and seek early medical advice if necessary. 🩺
Diagnosis of Pancreatic Cancer
Diagnosing pancreatic cancer can be a complex process, primarily because the symptoms often do not appear until the disease is advanced. Early detection is crucial for improving survival rates, so understanding the diagnostic methods is essential.
Common Symptoms to Watch For
While many people may not experience symptoms in the early stages, some common signs to be aware of include:
- Abdominal pain: Often felt in the upper abdomen and may radiate to the back.
- Weight loss: Unexplained weight loss can be a significant indicator.
- Jaundice: Yellowing of the skin and eyes, indicating bile duct obstruction.
- Changes in appetite: A sudden loss of appetite or feeling full quickly.
- Digestive issues: Nausea, vomiting, or changes in stool color.
Diagnostic Tests
If pancreatic cancer is suspected, several tests may be conducted to confirm the diagnosis:
- Imaging Tests: Techniques such as CT scans, MRI, and ultrasound help visualize the pancreas and surrounding organs.
- Blood Tests: Certain markers, like CA 19-9, can indicate pancreatic cancer, although they are not definitive.
- Biopsy: A tissue sample from the pancreas is taken to check for cancer cells. This can be done through endoscopic ultrasound or fine-needle aspiration.
It’s important to consult with a healthcare professional if you experience any of these symptoms or have risk factors associated with pancreatic cancer. Early diagnosis can significantly impact treatment options and outcomes. 🩺
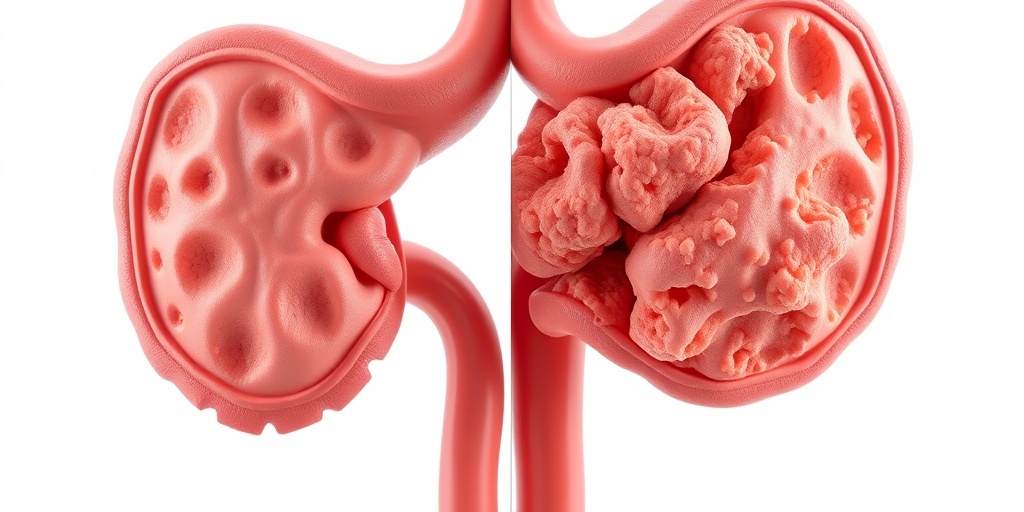
Stages of Pancreatic Cancer
Understanding the stages of pancreatic cancer is vital for determining the most effective treatment plan. The staging system helps to describe the extent of the disease and whether it has spread to other parts of the body.
Stage 0: Carcinoma in Situ
At this stage, abnormal cells are found in the lining of the pancreas but have not invaded deeper tissues. This is often referred to as pancreatic cancer in situ and is highly treatable.
Stage I: Localized Cancer
In Stage I, the cancer is still confined to the pancreas. It is divided into:
- Stage IA: The tumor is 2 cm or smaller.
- Stage IB: The tumor is larger than 2 cm.
Stage II: Localized with Lymph Node Involvement
Stage II indicates that the cancer has spread to nearby lymph nodes but remains localized to the pancreas. This stage is further divided into:
- Stage IIA: The tumor has not spread beyond the pancreas.
- Stage IIB: The tumor has spread to nearby lymph nodes.
Stage III: Locally Advanced Cancer
At this stage, the cancer has spread to major blood vessels or nerves near the pancreas, making surgical removal more challenging. However, treatment options may still be available to manage the disease.
Stage IV: Metastatic Cancer
Stage IV is the most advanced stage, where the cancer has spread to distant organs, such as the liver, lungs, or peritoneum. This stage presents significant challenges for treatment, focusing primarily on palliative care to improve quality of life.
Each stage of pancreatic cancer requires a tailored approach to treatment, which may include surgery, chemotherapy, radiation therapy, or a combination of these methods. Understanding the stage of the disease is crucial for patients and their families as they navigate treatment options and prognosis. 🌟

Pancreatic Cancer Treatment Options
When diagnosed with pancreatic cancer, understanding the available treatment options is crucial for patients and their families. The treatment plan often depends on the stage of the cancer, the patient’s overall health, and personal preferences. Here, we’ll explore the most common treatment modalities for pancreatic cancer.
Surgery
Surgery is often the first line of treatment for patients with localized pancreatic cancer. The most common surgical procedure is the Whipple procedure, which involves removing the head of the pancreas, part of the small intestine, and sometimes part of the stomach. This surgery can potentially cure the cancer if it hasn’t spread.
- Whipple Procedure: Ideal for tumors located in the head of the pancreas.
- Distal Pancreatectomy: Involves removing the tail of the pancreas and sometimes the spleen.
- Total Pancreatectomy: Removal of the entire pancreas, which may be necessary in certain cases.
Radiation Therapy
Radiation therapy uses high-energy rays to target and kill cancer cells. It can be used in conjunction with surgery or as a standalone treatment, especially for patients who are not surgical candidates. This therapy can help shrink tumors before surgery or alleviate symptoms in advanced stages.
Chemotherapy
Chemotherapy involves the use of drugs to kill cancer cells or stop their growth. It is often administered before surgery (neoadjuvant therapy) to shrink tumors or after surgery (adjuvant therapy) to eliminate any remaining cancer cells. Common chemotherapy regimens for pancreatic cancer include:
- FOLFIRINOX: A combination of four drugs that has shown effectiveness in treating pancreatic cancer.
- Gemcitabine: Often used alone or in combination with other drugs.
Targeted Therapy
Targeted therapy focuses on specific characteristics of cancer cells. For pancreatic cancer, drugs like nab-paclitaxel (Abraxane) are used in combination with gemcitabine to target cancer more effectively. This approach can lead to better outcomes with fewer side effects compared to traditional chemotherapy.
Immunotherapy
Immunotherapy is an emerging treatment option that helps the immune system recognize and attack cancer cells. While still under research for pancreatic cancer, some patients may benefit from clinical trials exploring this innovative approach.
Clinical Trials
Participating in clinical trials can provide access to new treatments that are not yet widely available. These trials are essential for advancing our understanding of pancreatic cancer and improving treatment options. Patients should discuss with their healthcare team whether a clinical trial is a suitable option for them.
Living with Pancreatic Cancer
Living with pancreatic cancer can be challenging, both physically and emotionally. However, many patients find ways to cope and maintain a good quality of life. Here are some strategies and considerations for those navigating life with this diagnosis.
Managing Symptoms
Patients may experience various symptoms, including pain, weight loss, and digestive issues. Effective symptom management is crucial for improving quality of life. Here are some common approaches:
- Pain Management: Medications, including opioids and non-opioid analgesics, can help control pain.
- Nutritional Support: Working with a dietitian can help manage weight loss and ensure proper nutrition.
- Digestive Enzymes: Supplements may be necessary if the pancreas is not producing enough enzymes.
Emotional Support
The emotional toll of a pancreatic cancer diagnosis can be significant. Patients and their families should consider seeking support through:
- Counseling: Professional therapy can help process feelings of anxiety and depression.
- Support Groups: Connecting with others facing similar challenges can provide comfort and understanding.
Staying Informed
Knowledge is power. Staying informed about pancreatic cancer and its treatment options can empower patients to make informed decisions about their care. Regular communication with healthcare providers is essential for understanding the disease and treatment progress.
Maintaining a Healthy Lifestyle
While it may not cure pancreatic cancer, maintaining a healthy lifestyle can improve overall well-being. This includes:
- Balanced Diet: Eating a variety of nutrient-rich foods can help support the body during treatment.
- Regular Exercise: Gentle physical activity can enhance mood and energy levels.
- Avoiding Tobacco and Alcohol: These substances can worsen health outcomes and should be avoided.
Living with pancreatic cancer requires resilience and support. By understanding treatment options and adopting healthy coping strategies, patients can navigate their journey with greater confidence and hope. 🌟

Frequently Asked Questions about Pancreatic Cancer
What are the early symptoms of pancreatic cancer? 🤔
Early symptoms of pancreatic cancer can be subtle and may include:
- Unexplained weight loss
- Abdominal pain or discomfort
- Loss of appetite
- Jaundice (yellowing of the skin and eyes)
- Changes in stool color or consistency
If you experience any of these symptoms, it is important to consult a healthcare professional for further evaluation.
What is the survival rate for pancreatic cancer? 📊
The survival rate for pancreatic cancer varies based on several factors, including the stage at diagnosis and the patient’s overall health. Generally, the 5-year survival rate for all stages combined is around 10%. However, if detected early, the survival rate can be significantly higher.
What are the treatment options for pancreatic cancer? 💊
Treatment for pancreatic cancer may include:
- Surgery (e.g., Whipple procedure)
- Chemotherapy
- Radiation therapy
- Targeted therapy
- Clinical trials for new treatments
The choice of treatment depends on the stage of the cancer and the patient’s health condition.
What are the risk factors for developing pancreatic cancer? ⚠️
Several factors may increase the risk of developing pancreatic cancer, including:
- Smoking
- Obesity
- Chronic pancreatitis
- Family history of pancreatic cancer
- Diabetes
Understanding these risk factors can help in taking preventive measures.
How is pancreatic cancer diagnosed? 🩺
Diagnosis of pancreatic cancer typically involves a combination of:
- Medical history and physical examination
- Imaging tests (e.g., CT scans, MRI)
- Blood tests (including tumor markers)
- Biopsy to confirm the presence of cancer cells
Early diagnosis is crucial for effective treatment.
What is the prognosis for stage 4 pancreatic cancer? 🌟
The prognosis for stage 4 pancreatic cancer is generally poor, with a lower survival rate compared to earlier stages. Treatment focuses on palliative care to manage symptoms and improve quality of life. Each case is unique, so discussing individual prognosis with a healthcare provider is essential.